Related Topics
Philadelphia Medicine
The first hospital, the first medical school, the first medical society, and abundant Civil War casualties, all combined to establish the most important medical center in the country. It's still the second largest industry in the city.
Medical Economics
Some Philadelphia physicians are contributors to current national debates on the financing of medical care.
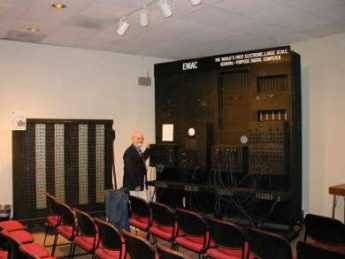
Computers, Digital Cameras, and Cellphones
Much of the early development of the electronic computer took place in Philadelphia. We lost the lead, but it might return.
Insurance in Philadelphia
Early Philadelphia took a lead in insurance innovation. Some ideas, like life insurance, flourished. Others have faded.
Philadelphia Economics
economics
Old Age
New topic 2019-04-09 16:04:33 description
Obamacare: Examination and Response
An appraisal of the Affordable Care Act and-- with some guesswork-- its tricky politics. Then, a way to capture major new revenue, even paying down existing Medicare debt, without raising premiums or harming quality care. Then, an offering of reforms even more basic, but more incremental. Finally, the briefest of statements about the basic premise.
Computerizing Medical Care
Note: This article was written in 1999, long before Computerized Medical Insurance Exchanges were such a disaster:
|
| First Computer |
My first encounter with a computer was in 1958, and I have loved them ever since. As president of what called itself the Delaware Valley Hospital Computing Society, I remember giving a dinner speech concluding as follows: "If you want to be happy for a day, get drunk. If you want to be happy for a week, get married. But if you want to be happy for a lifetime, get a computer!" After fifty years, my affection continues. But to be candid, billions of dollars about to be spent on computers in medical care will mostly be wasted. Even worse, like malpractice suits computers will induce behavioral changes in the system costing far more than the directly visible costs.
That's unpopular news at present since the National Business Coalition for Health has launched a major lobbying campaign to persuade Congress to spend an initial billion dollars inducing physicians to maintain an electronic medical record. Various health insurance companies already provide financial incentives to doctors to file electronic claims forms, eventually threatening to reject any claim submitted on paper. The American College of Physicians has established a rather large department to develop programs for physicians to use in their practices; twenty years ago the University of Indiana started much the same thing. The College of Physicians of Philadelphia has spent close to a million dollars on such a project. It is reported that Microsoft Corp. has a massive project underway to supply electronic medical records. It sounds fairly easy to obtain large research grants from the government to devise something, anything, useful in this area. In my own case, training funds really weren't necessary, since I eagerly got into the field when everybody was a beginner. I was just as good a beginner as any other beginner. But let me repeat: the electronic medical record has been in the past and will be for decades, an expensive digression. In health care, creating more administrative work isn't the solution, it is the problem.
For fifty years the problem with an electronic medical record was that it took too much of the doctor's time to complete his part of the input, and then cost him too much to pay employees to do the rest. Presumably, automatic voice recognition and dictation will soon make it possible to record doctor's notes without handwriting or typing. Since, however, the elimination of current paper forms and check-off boxes will create a major problem in organizing the dictation verbiage, it could add five or ten additional years before programmers manage to rearrange dictation material and effectively integrate it into organized form, complete with laboratory results, dictated x-ray and EKG reports, even small images of the original material. Temperature, blood pressure, weight, photographs and the like can all be readily integrated into the stored electronic record, but to do so usefully is an expensive programming project. Doctors are quite right to be anxious they will lose control of the usefulness of their records in order to ease the task of programmers, speed up the sluggish pace of development, and reduce what will surely be an unexpected cost overrun. Storage and retrieval of such records is known to be an achievable but expensive task, which however also risks sacrificing the speed and ease requirements of the medical task it is supposed to serve -- in the name of cost-effectiveness.
Computers are no longer an unfamiliar tool; physicians have altogether too much experience with "vaporware", unrealized promises of convenience, and the damaging effect on the medical quality of the philosophy of Quick and Dirty. To respond to their resistance to design blunders with an accusation of undue conservatism is to provoke an icy stare and gritted teeth. Inevitably, the effective use of automation will require a redesign of workflow with major disintermediation of "gopher" staff; after all, that is how cost savings are to be achieved. That will provoke outcry that physician time is the most expensive component in the process, but unfortunately, physicians will discover Information Specialists with a business background will brush that argument aside. The most overpaid people on the face of the earth are investment bankers, but information consultants have persuaded business executives that inefficiency of the investment process is more expensive than even an investment banker's time. Having been through this themselves, insurance executives are unlikely to pay the slightest attention to physicians dancing to a familiar old tune.
For all that, data input is not the real problem; it's just the first problem. It's in a class with data storage and retrieval, which is expensive and cumbersome when you add a need for instant access and total privacy. But costs will come down steadily, and eventually, we can expect automated fingerprints or other biological identification, and cheap instant retrieval. Doctors will be able to make rounds in the hospital with a computer in their pocket, record telephone calls in their entirety, dial automatically and whatnot. There are problems with wireless transmission inside buildings with steel girders, and legal requirements for signatures on narcotic orders, but if we are determined, these problems can be overcome as easily as they were with electronic check writing and stock brokerage. Cost may top twenty billion dollars in twenty years, but it all can be done if we insist.
But then you encounter the real problem. Information will accumulate in these records in staggering amounts. Even if you resolutely resist demands to have the nurses record every groan, and the orderlies file every laundry slip, the legitimately important medical information will be exposed as the massive heap of transients that they really are. Plaintiff lawyers will insist no scrap of data may be deleted, hospital administrators will insist on compliance, when in fact most of a doctor's concentrated effort is devoted to brushing aside momentarily distracting data in order to see what's going on and react to it instantly. When a quick look doesn't solve the problem, the doctor goes back for additional data. If you disrupt these skills and traditions of coping with information overload, evolved over centuries, you will at best impose frustrating delays on a complex system under pressure, and ultimately inspire elaborate systems of short-cuts. The Armed Forces are famous for paperwork, but even they know better than to ask a pilot for his Social Security number as he starts a bombing run. The hospital nursing profession has already just about collapsed under paperwork pressure. If you see five nurses in a hospital, three of them will be sitting down writing something. The terrible truth is that no one reads it, no one checks it, and ultimately it sits in the record room waiting for a plaintiff lawyer with unlimited time to sieve out some misrecorded misconception or uninformed conclusion. My faith in the computer is such that I feel sure that methods can be devised to produce periodic summaries, automatic alarm signals, and mostly effective prioritization of data elements. Unfortunately, medical care is changing at such a rapid rate that ad hoc automation of physician thought processes cannot keep up with the current pace of change in medical progress. You would think some things would be unthinkable, but since I can remember the organized campaign to suppress the CAT scan as an unnecessary expense, I confidently predict that programmer inability to keep up with some advance in medical care will at times lead to organized outcry that we should slow down the pace of improving medical care, so that computer clerks can keep up with it. But that is only a small part of the issue, which at its center is that physician time will be dissipated and his attention distracted by presenting him with unwieldy amounts of neatly printed, spell-checked, encrypted and de-encrypted, biometrically secure, hierarchically prioritized -- avalanches of data which are irrelevant to the issues of the moment. The goal is not, after all, an electronic record. The local goal is to decrease the cost of medical care by increasing the productivity of the physician, and the overarching goal is high-quality patient care at a reasonable price. Behind all that, since the impetus comes from NBCOH -- the ones paying the insurance premiums -- suggests that the local goal is not so much the improvement of care as oversight reassurance that cares provided has been as good and as cheap as possible. The goal is legitimate, but this cybernation approach looks to be self-defeating by being overly specific.
If the reader has the patience for it, let me now cite a historical example of the third-party tail wagging the medical dog. In this case, third-party health insurance similarly overextended its reach by imposing internal health system changes, trying to facilitate the role of monitoring it externally. Specifically, the system of diagnostic code numbers was changed from one devised by the medical profession for its purposes, into a different coding system devised outside medial profession sponsorship, which seemed to suit the needs of payment agencies better even though it suited medical purposes less. After twenty-five years, it is now clear that third-party payers have shot themselves in the foot on this matter, and everyone is worse off. The topic, please pardon the obscurity, is the diagnostic coding system.
To go back to beginnings, the American Medical Association perceived a need for a diagnostic coding system in the 1920s. Organizing or even merely indexing vast amounts of information about a disease required more specificity than freestyle verbal nomenclature could provide. Quite a distinguished panel of specialists and consultants then produced the Standard Nomenclature of Diseases (SNODO) which in time became the Standard Nomenclature of Diseases and Operations. In order to reduce ambiguity, this system developed a branching-tree code design for anatomy, linked to a branching-tree for causes of disease, ultimately linkable to a branching tree of procedures. These three sets of three-digit codes linked the components together with hyphens (000-000-000). The first digit of each was the most general, as in Digestive, Musculo-skeletal, etc. and subsequent digits were progressively more specific and detailed, as in "Digestive, large intestine, sigmoid colon". The causes of disease would resemble "Infections, bacterial, streptococcal". An example of Procedures would be "Incision, incision, and drainage, drainage and insertion of the drain". In nine digits, it was thus possible to represent " incision, drainage, and insertion of a drain into a streptococcal infection of the sigmoid colon". After a while, the codes grew from three to five and six digits, again repeated three times, so an immensely detailed, unambiguous description might be coded in fifteen digits by a physician who knew the rules but didn't own a codebook. This code was ultimately taken over by the Academy of Pathology, expanded and is called SNAP. The pathologists absolutely refused to give it up.
The rest of the profession gradually yielded to the pressure of hospital administration, who was pressured by the Association of Medical Record Librarians, responding to the views of outside statistical interests, particularly insurance. A simpler, shorter coding system was needed, they felt, concentrating on the thousand most common diseases. The International Classification of Diseases was produced, reducing the millions of SNODO diagnoses to 999 by heavy use of several varieties of "Miscellaneous" or "Not Otherwise Classifiable (NOC)". Since the goal was to count the incidence of common diseases, the coding system was stripped of any logical tree-branching and became a short list of what was most common, starting with 1 and going to 999. In time, of course, the common-ness of conditions changed, and various complaints from various directions forced the ICD to go to 4 digits, then five. Unanticipated conditions or complications eventually required the patchwork of some alpha "modifiers", and the original short hodge-podge became a long and bewildering hodge-podge. Coding accuracy declined markedly, but ho-hum. The health insurance companies paid the bill, no matter what the code said. At another place, we will discuss the entertaining way that Ross Perot became a billionaire out of the computer chaos of Blue Cross and Medicare at this time, but right now the central theme to follow is DRG, Diagnosis Related Groups. Try to follow, please.
By 1980, Medicare was fifteen years old. It was clear that certain things just had to be changed because the excuse that the system was new and untried was beginning to wear thin. The early designers of the system based their payments on auditing a hospital's yearly costs, auditing the proportion of patients who were Medicare beneficiaries, and paying a proportionate share. That was easy and reasonably accurate, but it had a rather significant flaw that it took no account of whether the patients needed to be in the hospital in the first place. Or whether they needed to stay so long. The response they adopted (in the Budget Reconciliation Act of 1983) is a measure of just how desperate they must have felt. Knowing full well how inaccurate the ICD coding system was in practice, it was all there was. Consultants, particularly at Yale, ran computer simulations of various subsets of ICD codes to find a formula that would produce approximately the same hospital payments as the system of cost reimbursement. If memory serves, the original formula was to divide the thousand ICD codes into 27 diagnosis-related groups (DRG). Eventually, the process was tweaked to seventy or eighty groups. Walter McNerny, then Past President of the American Hospital Association told Congress hospitals could live with this system, and promptly we had a system for paying out hundreds of millions of dollars. It was touted as a highly sophisticated advance in the arcane science of hospital reimbursement, so it must have included a lot of deliberate overpayment. I can remember trying to remonstrate with McNerny, who felt he didn't have time for the discussion. Physicians had very little to do with the DRG portion of the 1983 Medicare Amendments because the AMA had long insisted that physicians and hospitals go their separate ways on reimbursement. Russell Roth, who was president of the AMA at the time, recounted many times the episode in the Oval Office, when it was announced to Lyndon Johnson that Dwight D. Eisenhower"was in the next room waiting for him. LBJ excused himself to leave, and on the way out said to Wilbur Cohen, "Give him anything he wants." Things were destined to change, but at least for a very long time, physician and hospital reimbursements were strictly independent.
Originally published: Sunday, July 29, 2007; most-recently modified: Sunday, July 21, 2019