4 Volumes
Constitutional Era
American history between the Revolution and the approach of the Civil War, was dominated by the Constitutional Convention in Philadelphia in 1787. Background rumbling was from the French Revolution. The War of 1812 was merely an embarrassment.
Health Reform: Children Playing With Matches
Health Reform: Changing the Insurance Model
At 18% of GDP, health care is too big to be revised in one step. We advise collecting interest on the revenue, using modified Health Savings Accounts. After that, the obvious next steps would trigger as much reform as we could handle in a decade.
Consolidated Health Reform Volume
To unjumble topics
Obamacare: Examination and Response
An appraisal of the Affordable Care Act and-- with some guesswork-- its tricky politics. Then, a way to capture major new revenue, even paying down existing Medicare debt, without raising premiums or harming quality care. Then, an offering of reforms even more basic, but more incremental. Finally, the briefest of statements about the basic premise.
TABLE OF CONTENTS
foo
bar
sna
Annotated Table of Contents
CHAPTER ONE: Where Are We, And How Did We Get There?
--- Teddy Roosevelt started it, but politicians have shorter memories than historians. For practical purposes, Obamacare 2012 is an extension of the Clinton health proposal of 1991, with HMOs deleted, and computers added. It is useful to conjecture Bill Clinton's strategy, which would explain much of the present muddle. If Hillary runs, we could even see it tried for the third time.
2589 Clintoncare and Obamacare: Historical Foreword
1729 Picking Out the Raisins From the Pudding
2670 Welcome to Welfare
1714 Reforming Health Reform, New Jersey Style
2622 Children, Playing With Matches
2602 Text of AFFORDABLE CARE ACT, PL 111-148, March 23, 2010, Renamed HR 3590 https://www.gpo.gov/fdsys/pkg/BILLS-111hr3590enr/pdf/BILLS-111hr3590enr.pdf
2594 The Real Obamacare, Unveiled
2672 Text of Section 1501, renamed Section 5000A: MINIMUM COVERAGE
2639 Text of Section 1251 (H.R. 3590):PRESERVATION OF RIGHT
TO MAINTAIN EXISTING COVERAGE 2673 Proposal: Coordinate Sections 1501 and 1251
2676 Health Care and Education Reconciliation Act of 2010
CHAPTER TWO: The Supreme Court Has Its Say
--- The U.S. Supreme Court had nursed certain Constitutional issues since Franklin Roosevelt's court-packing days, but it was state Attorney Generals who propelled States' Rights into the central Constitutional issue of the first few days of Obamacare. Liberal academics have long flirted with remaking the whole Constitution, and President Obama once taught Constitutional Law. While extreme Liberals nurse Constitutional revision, most Liberal politicians would prefer to split Republican voters with a third party. It is too early to predict which party would suffer.
2624 State and Federal Powers: Historical Review 2250 Obamacare's Constitutionality
2289 Roberts the Second
2592 More Work for the U.S. Supreme Court: Revisit Maricopa
2625 What Can Supreme Court(s) Do About Tort Reform?
2613 ERISA Is Thrust Into the Battle
CHAPTER THREE: Sudden Fiasco Of Electronic Insurance
----At first, it seemed a minor programming problem had temporarily inconvenienced the Electronic Insurance Exchanges. The realization soon emerged that the whole program was sloppy and untested, requiring months of repair, if not the abandonment of Obamacare. If direct marketing gets discredited, it would be a pity. The underlying idea was good and achievable. But this implementation was a disaster.
1288 Money Bags
2603 Electronic Insurance Exchanges
2626 Streamline Health Insurance?
2604 Redesigning Electronic Insurance Exchanges
2611 Phasing In A Direct Premium Payment
2615 Creative Destruction for Health Insurance Companies
CHAPTER FOUR: Small, Quick Proposals to Extend Health Savings Accounts
----Here's our alternative proposal, first devised by John McClaughry and George Ross Fisher in 1980, enacted into Law in 19xx by Bill Archer, and now numbers more clients than Obamacare. It requires publicity more than legislation, but six small technical amendments could rapidly turn an experiment into a national program. It seems to save as much as 30% of premiums, without much disturbance of the healthcare delivery system.
2637 FIRST PROPOSAL, Amending HSAs To Include Tax Sheltering
2573 SECOND PROPOSAL:Spending Accounts into Savings Accounts
2611 THIRD : Phasing In Direct Premium Payments
2584 FOURTH: Investments Pay the Bill: Obstetrics Lengthens Duration, Deductible Reserve is the Kernel.
2607 FIFTH: Having Invested, How Do You Reimburse the Providers of Care?
2630 SIXTH: Indemnity and Service Benefits
2585 Foreword: Children Playing With Matches: Investigating and Debating the Healthcare System 09 2636 2606
CHAPTER FIVE: HSAs, Backwards and Forwards
----The above describes the HSA and how it might be more useful if tweaked a little. This next chapter is a much more grandiose version, expanding the simple idea into a proposal for lifetime health insurance and describing the enormous unsuspected potential. Ninety-year projections are never accurate and require many mid-course corrections. We propose a new institution to monitor and steer it and attempt to describe what might be encountered. The power of compound interest could well pay for most of healthcare, but it is unnecessary to over-reach. Paying for a third of our costs would be accomplishment enough.
2590 Health Insurance Design.
2638 Pay As You Go
2587 Predictions of Future Healthcare Costs: Quis Custodiat Ipsos Custodes?
2628 Average Lifetime Medicare Balance Sheet
2627 Shifting Money Backward in Time: Managing the Transition
2593 Economics of Chronic Disease and Catastrophic Illness
2634 Comments on Diagnosis Related Groups (DRG)
2635 Admonitions: Using the Transition to Lifetime Health Insurance as an Inflation Restraint
2473 An Unending Capacity to Generate New Problems
1734 Healthcare Reform for Lobbyists
2485 Cost Shifting, Reconsidered
2571 Proposed: A Republican and/or Conservative Healthcare Solution
2610
CHAPTER SIX; Reforms More Basic Than Obamacare
----Obamacare is just coverage extension by subsidies. The biggest flaws in our payment system are fifty years old and are the cause of most of the delivery system flaws. Meanwhile, Science is reducing disease costs by reducing disease, for all income brackets. By switching "medical" care into "health" care we keep authorizing new carpetbaggers to bill the insurance. Physicians received 20% of payments in 1980; now it is 7%, half of which is spent on overhead. Nevertheless, compound interest income could reduce costs greatly without changing healthcare. Lifetime insurance (above) could pay for about a third of future costs; direct cost efficiencies could probably save another third, leaving a third to be paid in cash. But don't make it entirely free, unless you want to make it entirely ruined.
2633 Stepping out of the Obamacare Frame
1730 What Obamacare Should Say But Doesn't
2616 The Coonskin Hat
2404 "They Don't Make That, Anymore"
2564 Last Cow in Philadelphia
2112 Paying for Assisted Living
1431 July 4, 1776: Patients in the Pennsylvania Hospital on Independence Day
1733 Obamacare And Its Repair, Executive Summary
2453 What's The Matter With a Conservative Answer?
Clintoncare and Obamacare: Historical Foreword
Twenty years after their Health Proposal was withdrawn from Congress in 1994, the Clintons can thank their lucky stars they withdrew it. One thing is clear; the Obama health insurance mandate followed a surprisingly similar early trajectory, beginning with a protracted flurry of publicity and astonishing promises that never materialized. But the Clinton plan was quietly sabotaged without much explanation before it got this far, nowadays almost pretending the subject had never been mentioned. In both cases, a President had proposed an adventure which the American public didn't want to undertake, but only one of them backed off.
As of this writing, the Affordable Care Act is a law actually in force, even though the party in opposition is determined to eliminate it as soon as it regains control, whereas the other party acts determined to conceal its real content for as long as it can. From its behavior, the Obama administration seems willing to provoke a Supreme Court contest, rather than conciliate a retreat. It seems unlikely the public will abandon its Constitution in order to preserve a health insurance plan, particularly when the President is running out of time to make it successful. Even if he could rescue a failing program, both foreign affairs and the financial crisis seem more urgently in need of his time and attention. We like to see signs of competitiveness in our President, but accomplishing what the Clintons, Harry Truman, and Theodore Roosevelt could not accomplish, does not strike most people as sufficiently useful. Some cynics feel his real strategy amounts to what they call in football, "playing for the breaks". Wait until your opponent makes a mistake. This book is written in the hope that both parties are as confused as they seem, remaining open to new ideas rather than rigidly following a playbook. Somewhere along a newer path, we might reset our compass to eliminating the disease as the route to reducing disease costs, instead of tinkering with insurance while we watch costs go up. For thousands of years, the elimination of disease has been an impossible dream. Not any more.
Let's begin with brief mentions of the Clinton Plan because it apparently set the original pattern. At its center was a national blueprint for Managed Care, called HMO (Health Management Organizations.) Leaders of large business, already intrigued by the notion of constraining national healthcare costs by clever management of the health insurance they provided their employees, had originally played along with the Clinton administration. As did their reluctant agents, the large-group health insurance companies. Together, Big Business and Big Insurance had previously taken a step away from state-regulated Blue Cross systems toward a nationally regulated ERISA system, in order to cross state lines more comfortably. Insurers were also having problems with their turf: the hospitals and the unions. Originally, hospitals had once, ninety years ago, joined with business to form locally based health insurance, often with small business and charitable foundations in the lead. However, insurance and the federal government eventually dominated (but underfunded) the health payment scene, with everybody unrealistically expecting business to pick up escalating costs that business could no longer control. And while business had to get along with its unions, it was disquieting to business leaders to find so much union influence infiltrating nonprofit insurance leadership. Hence they were uneasy to find so much interest in unionizing hospitals, so much involvement in partisan politics. Furthermore, the old actors were uneasy with the new actors looking for control, hence the subtle change of "medical care" into "health care", as a way of wig-wagging new allegiances. Finding a hospital-centered model increasingly worrisome, leaders of business had been briefly intrigued by the concept of shifting the control center to HMOs, which seemed to act more like businesses, and thus might be a better buffer with the feds. One of the main problems with dragging out major reforms over decades is that old alliances grow stale, old promises become invalid when new combatants join the battle. Gradually a number of disillusioned businesses quietly withdrew their support from the original Clinton proposal as they learned more of its new realities. In the view of the business and insurance world, national politics of some sort would soon cripple a complex HMO idea that needs good management, most of all. If the rest of the "health" world didn't feel it retained any debts to the pioneers of pre-paid health insurance, well, big business had other things to do.
Congressmen understood the general direction of this mixed message and, at least as defined by "HMO", the floor leaders of the Clinton Plan found they no longer had the votes to pass the health bill. The Clinton Administration yielded and let Big Business go it's a way. Businesses then undertook the HMO project themselves, only to get burnt fingers when they discovered the HMO concept, without a physician or patient enthusiasm, was doomed to failure no matter who co-sponsored it. The public, even their own employees, resented the regimentation of HMO systems, except perhaps for union political machines on the Atlantic and Pacific coasts. To the interior of the country, the enduring California image of HMOs was not an asset.
Unfortunately, Democrats also escaped learning from Clinton cares flaws by failing to pass it. Most importantly, liberal leaders never quite grasped the message the public was sending back to them: The public's healthcare and its governance belong to us -- not to our employers, nor to our elected politicians. If some group wants to pay our bills for us, Americans would pocket the money. But ownership, transferring real ownership of healthcare to the public sector, had never been considered a serious option by a very large segment of the population. Local control was the main reason healthcare had lagged behind the rest of the economy in the shift from state to federal regulation. The debate was still about healthcare, but it might easily switch to a debate about the Constitution, which the Constitution was not likely to lose.
 Powers not granted to the federal government...., are reserved to the States or the people. 
|
| Tenth Amendment: What Part Don't You Understand? |
The Tenth Amendment could suddenly be recited by people more characteristically excited by professional football. If there was to be the talk of amending the Constitution, perhaps it was the part about Congress making its own rules, which needed changing. State governments, ordinarily regarded as the weakest part of our political system, became a White Hope. Congress itself had become more polarized than at any time in the preceding fifty years. Not to mention the fragile condition of foreign affairs or the bewildering tangles of international monetary policy, it looked to be high time to ditch this health thing of Obama's.
Accordingly, this book roused itself into print. Because, no matter what the final fate of Obamacare, it isn't really healthcare reform, it isn't even serious health insurance reform. One main reason it deserves to raise so much concern is the way polarization is spreading into other basic institutions. A real danger is we may spend so much money, and devote so much of our limited attention span to Obamacare, that we never will get around to some basic reform of health care. No matter how else it may be described, this book is about real reform of health care, including absolutely indisputable reform of the insurance part. But because of the political timetable, I came to feel that there was only half the time I needed to be complete. I cut off the bibliography, had to be satisfied with a mechanical index, and then with great regret, cut out at least half of the "inside baseball" describing the details of healthcare reforms -- as distinguished from Health Reform. Unless this book provokes less controversy than I anticipate, there won't be time to do much but answer it.
George Ross Fisher, MD
PhiladelphiaPicking Out the Raisins From the Pudding
There appears no better blueprint for the 1993 healthcare reform legislation (commonly called "Clintoncare") than Jacob Hacker's 1999 book The Road to Nowhere. If President Obama did not use this same roadmap for the "Obamacare" health program, it still remains quite a good description of what he did do. His following this earlier playbook would plausibly explain much that is otherwise mysterious.
The Hacker book was originally an academic thesis written several years after the (Hillary) Clinton Health Plan experienced ignominious disappearance in the halls of Congress. By then, the Clinton episode of 1993-94 was quiet and forgotten, so participants probably felt it was safe to describe big-shot politics to a college kid writing a thesis. The resulting book was easy to follow, had a ring of authenticity, and advanced the author's career. Advanced it so much the same Jacob Hacker later became visible near Democratic policy circles, even seemingly advising political deals, even though strangely quiet, lately. The similarities between the Obama initiative and Clinton's earlier strategy in Hacker's book, are striking. However, a judgment must be suspended whether to frame it as a cautionary tale, or a guidebook. In fact, the possibility that Mrs. Clinton plans to use the blueprint a third time produces a strange fascination among even her enemies.
 1. Pad anything into Senate and House bills. 2. Send the padded bills to a conference committee. 3. Delete all but your own ideas. 4. Ram it through. 
|
| The Clinton Strategy |
Boiling it down, the (Bill) Clinton strategy was to confront a House-Senate conference committee with a vast pile of often conflicting proposals, sent to a conference committee for a proposal to reconcile inconsistencies. In fact, a coherent proposal could not emerge from a Clinton bill, until the President sent his list of proposed deletions to that conference committee. After trimming to its essentials, the conference committee reconciliation would then return for House and Senate approval, probably against some holiday deadline to quash objections. The process would resemble picking out the raisins from a pudding, combined with the nuisance of buying off a few soreheads, except for one thing. The Executive Branch deftly acquires more power over legislation than the Founding Fathers ever contemplated. Michelangelo's remark, that carving statues is just a matter of throwing away what you don't want, is bitterly appropriate here, especially from the viewpoint of those who thought they were elected to write laws, not follow orders. On the other hand, this approach favors a party with safe seats from concentrated urban districts, tending to be more compliant to party bosses .
In a technical sense, this process is more equivalent to a line-item veto. (A line-item veto, by the way, is something Congress repeatedly refuses to grant). It's hard to oppose an omnibus bill until its outline appears, and this Michelangelo process tends to obscure the tone and central theme of legislation until the last possible moment. From the point of Conference Committee forward, passing it back for ratification becomes a matter of rushing it ahead of criticism, and indirectly lessens the power of public opinion. Nor would be the first time a few little extra zingers, never discussed by either the House or the Senate, got slipped into a conference bill, which is typically several hundred pages in length. And the timing for the release of the omnibus legislation could be selected, quite likely the day before Thanksgiving or Christmas when newsmedia was away from work. Or else after a long series of preparatory news events, building public expectations before a spectacular revelation day. But it is a mistake to focus on the press as being hoodwinked. It is the other Congressmen, the ones who ultimately don't get what they were promised.
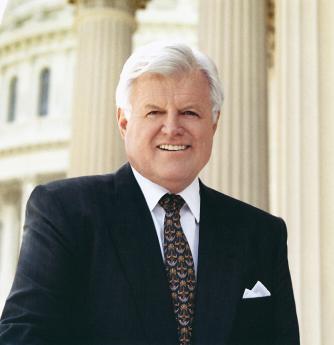
And finally, unexpected events can intervene, as Scott Brown's Senatorial election did in this Obamacare instance. A clever scheme got suspended in mid-air by the death of Senator Edward Kennedy. The bill had been passed by the Senate, but not the House. The House bill was so different it would require reconciliation with what by then would be a different composition of the Senate, and therefore could not pass the Senate a second time. So, a bill identical to the Senate version was jammed through the Democrat-dominated House, no amendments permitted, no conference committee needed to reconcile two differing bills. Unfortunately, the original plan was to include some provisions purely for the purpose of obtaining a Senate vote or two. The original plan was to be that "deficiencies" would be remedied by some raisins tucked in the House bill, which of course never came up for a vote. Thus the resulting legislation is the pure Senate version (with all its undesirable features remaining) and we may never know what was in the unpassed House bill that might have repaired unspecified Senate flaws. After all, this trickiness, does anyone wonder why so many Congressmen are dissatisfied with the result?
Looking back, it is hard to prove how much of the Clintons' original strategy was adopted by Obama, or how much influence Hacker and Hacker's book had, until someone on the inside writes another book and tells us about it. But the congressional strategy of the Obama Health Plan proposals does sound very similar to what we should probably give the name of "The Arkansas Strategy". That strategy would certainly explain a great deal of what happened; it scarcely matters how much the similarities were accidental and how much they were following the same playbook. Except, of course, if some of the participants decide to run for office in the near future, and try to do it all, a third time.

|
| Senator Edward Kennedy |
Senator Edward Kennedy's impending death, Senator Byrd's incapacity, and the contentiousness of the health reform topic always made it uncertain a 59-vote Democratic Senate leadership could assemble 60 filibuster-proof votes in favor of any healthcare proposal; one betrayal and you've lost. The Democratic Massachusetts legislature took away the right for Republican Governor Romney to fill a vacant Senate seat and restored it for a subsequent Democrat governor. In circumstances like this, every single Democratic senator can hold a proposal for ransom, while every single Republican senator will unite in opposition. When the majority shifts Republican, which could be rather soon, the roles will be reversed in an almost certain effort to repeal whatever passed. The public was left wondering whether healthcare legislation was worth hampering our interests in Iraq, Iran, Afghanistan, Syria, immigration reform and the national debt. The Democratic Congress had to worry it was not worth the political damage from hammering it through. They might also worry that the Supreme Court might be drawn in, expressing some unwelcome Constitutional viewpoints. It's really hard to know what to wish for.
|
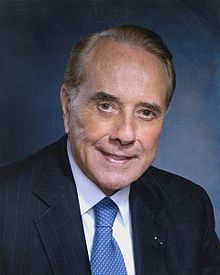
| Bob Dole |
Along the way, former Senate Majority Leader Bob Dole appeared on television and revealed a different insight about Senate behavior. Senator Baucus told the press that something called a Public Option could not pass the Senate, so he was not including it in his proposal. Extreme left-wing members of the Democratic party said they would "take a walk" if the Public Option was dropped. But although it was dropped, it was included in the House version and might thus have been restored in the conference committee. This "Montana" maneuver removed Public Option from Senate debate, still hoping to preserve those 60 votes. Under the circumstances, it isn't even necessary to remember what the Public Option was, but essentially, Public Option was a proposal for the Government to go into the health insurance business itself, in order to put overwhelming pressure on the insurance industry. In 1965 this was impossible, in 1992 it was unprepared for, in 2009 it was merely chaotic.
It is widely rumored the Public Option was a punishment for the reluctance of the health insurance industry to cooperate more fully with the President, or at least a threat of what could happen if they didn't soon cooperate. Indeed, you have to question what the attitude of the Insurance Industry really was, in a proposal which would greatly diminish their control of insurance. Karin Ingaglio, the chief lobbyist for private health insurance companies, admitted to the National Journal that her group had contributed millions of dollars to the Tea Party, leaving it unclear whether she was playing both sides of the street, or else hoping to defeat the Republicans with a third-party, Tea Party, distraction. Bob Dole was a gracious, gentle old man, musing about what might be going on. You don't suppose, he mused, the Public Option might be nothing more than a red flag in front of a bull, to be surrendered with a great show of disappointment. But actually, just a feint creating an uproar, to divert attention from the real zingers in the rest of the bill, which can then pass through unnoticed. But, no, Bob Dole didn't really imagine such a thing. It was just a wild thought he happened to have.
Political observers agree that presently rancorous Congressional partisanship is the worst in a century, and it is not shared by the public. Just about everyone in the political class sees gerrymandering as the main cause. Changes in the ways voter redistricting is conducted, some say the use of computers, has made gerrymandering much more effective. When numerous safe seats arise in this way, it is only a matter of time before the Legislative seats are filled with heedless, reckless partisans, beholden to no one. But it is just as bad, if the seats are filled with party hacks, forever obedient to the unelected rulers of urban political machines (leaders of party machines seldom run for office.) The seniority system takes over, and safe-seat partisans get control over Congressional committees and party discipline. This happens to both parties because incumbents from both sides unite to achieve it. But urban districts are harder to split into party lines, so states containing large cities tend to present a permanent disadvantage in numbers for Democrats, although uniform composition makes for much greater partisanship. Contestants for the dwindling number of uncertain districts are thus forced to act more cautiously, thus tending to seem more competent by the press and the public. But even if elected, they are powerless in the face of the more unrestrained partisans who control internal power plays, and who also tend to be long-term incumbents from safe seats. As a consequence, moderates are more likely to be singled out for sacrifice in the following election.
Scientific gerrymandering has certainly coarsened and hardened the political atmosphere, considerably reducing public control of its representatives. It should also be noted that Senate seats cannot be gerrymandered, but state legislative seats definitely can be, leading to a coalition between state legislators who are almost always party hacks, and U.S. Representatives, who are increasingly so. It is said that in New Jersey and Florida, it is possible to predict the next ten years of politics with precision if you only know how the gerrymandering was arranged. The Senate could probably devise a Constitutional amendment to fix this problem, with no chance of passing the House or getting ratified by the States. Therefore, the present main hope for representative government lies in the national party leadership of some party, intervening into the party nominations for safe seats. Even that, would take extraordinary luck and agility. It remains to be pointed out that 2020 is the upcoming year for a census, 2022 for redistricting.
Welcome to Welfare
 Percent of Their Hospital Cost Reimbursed: Medicaid 70%, Medicare 106%, Private Insurance 150%, Uninsured 400% (?) 
|
| Hospital Cost Shifting |
There's lots more; in politics there always is. The Pew Foundation, which now includes public opinion polling in its tasks, has pointed out 80% of the public does not share the polarization now so blatantly agitating the political class. Hence, some commentators have questioned the prevailing opinion of gerrymandering as the main source of it. These observers point to a worldwide decline in party affiliation; "independence" of party affiliation is claimed by nearly half of American voters when asked. Perhaps we have things backward, and gerrymandering is merely one effort, along with growing dependence on financial contributions by wealthy donors, to rescue party power. Television (and especially the Internet) prompts the voter to hang back before making decisions, hoping to decide something without pressure from party leaders. The growing tendency to vote straight party ballots is not taken by a few commentators as evidence of true voter wishes, but rather as evidence of the futility of resisting a two-party system. Some sophisticated observers feel straight ballots result from plurality ("first past the post") counting of votes, but this (unfortunate) trend seems more likely to be stimulated by (too) early voting by mail.
Since a two-party system favors moderate candidates over extremist ones, it may not be a bad system, but rather a good system adjusting to circumstances. A hidden cause of the present crisis in health care financing comes from the Medicaid programs, run by the states, but mostly (and inadequately) financed by federal taxes. A two-party system disciplines the nominating process by raising doubts about the ability of extremists to win the general election. Consequently, the final two candidates are often so similar the chance of a loser bolting the process, becomes small. In a proportional voting process, splinter parties cannot be silenced in the primaries, because political deals take place after the election when the public has become irrelevant to the voting outcome. Threats of public disaffection are therefore disregarded. This hidden feature went unrecognized at the Constitutional Convention, as indeed was the whole party apparatus. But it has to be counted as one of our greatest strengths, placing a much higher value on unity than dogma. If you follow this reasoning, you would have to conclude the present level of divisiveness will not persist. Because each generation has to learn its own lessons, it may recur, but it will not persist.
Nursing homes were not originally included in the 1965 legislation, but most states receive strong pressure to pay for elderly indigents in nursing homes, stranded by running out of savings. Perhaps it would be a good thing to include nursing home coverage in a reform bill, but nursing homes bear too much resemblance to work-houses to generate much demand to be in one. In variable degree, the circumvention has grown up of paying for nursing homes with money intended for hospitals but necessarily underpaying the hospitals. The hospitals make up the deficit by overcharging for outpatient services, as everybody will recognize who has been charged for the same service, both as an inpatient and an outpatient. By prevailing estimates, the Medicaid programs only pay hospitals about 70% of their actual costs. Hospitals escape insolvency to a minor degree by raising reimbursement demands on Medicare (to about 106% of costs) and more appreciably through private insurance (to something approaching 150% of costs). Teaching hospitals have some opportunity to raid funds intended for indirect research overhead, for resident stipends, and for disproportionate shares of an indigent, "self-pay" patients. Various accounting tricks account for the rest. For example, the transfer of schools of nursing from hospitals to universities has emboldened universities to seek the equivalent of traditional hospital reimbursement schemes, merely and mostly triggering new arenas for dispute, because the hospitals had hoped to profit from the transfer. Since Medicare somewhat overpays hospitals for its own patients, in recognition of the underpayment by states for indigents, current jargon blames the "government programs" for underfunding hospitals. A better summary of the situation is: Medicaid under-reimbursement is the largest source of hospital financing problems, but other problems are less resistant to change. That's pretty significant, in view of the Obamacare plan to put millions of uninsured into Medicaid, some of whom never asked to be insured at all, and most of whom have no previous experience with "welfare", so they need to start reading some books by Charles Dickens.

|
| Governor Christie of New Jersey |
The outcome of all this is nursing homes are in effect supported by Blue Cross and other private insurers of younger people, raising premiums to employer groups and individuals by something estimated like $900-1500 a year per subscriber. That's because Medicare is busy subsidizing Medicaid's hospital patients, the main source of hospital deficits. Because this juggling lacks straight-forwardness, results are inefficient; only about 42% of hospitals actually break even. As might be expected, knowledgeable employer Human Resources departments and hospital administrations know about and object to this system. They are cooperating with Obamacare more than might be otherwise expected, probably in the hope this cost-shifting can be adjusted more in their favor when it is less in the public eye. Mandating all employers to participate would, of course, increase the base of people sharing this exaction, but would ultimately link corporation treasuries to government deficits. The dream of the service unions would be to use this excuse to mandate the unionization of hospital employees. Governor Christie of New Jersey quickly saw a way to split the Union movement into public and private compartments through this. "Every time they get a raise, you get a tax increase," he told the unions of the private sector.
The participation of physicians in the Obamacare effort is riven by their own politics. For surgeons, the premiums for Malpractice insurance can sometimes run to $200,000 a year. An appalling proportion of obstetricians have been sued by their patients, to the point where women have no doctor to deliver their babies in certain parts of the country. For doctors in this high-risk category, relief from the plaintiff lawyers is the most pressing of all problems. On the other hand, many physician specialties have almost no malpractice risk and are much more exercised about the SGR reimbursement freeze, which has been in effect since the administration of Lyndon Johnson and has been severely undermined by inflation ever since then. With physician ranks divided by two different priorities, the way is open to promise both and reward neither.
 The powers not delegated to the United States by the Constitution, nor prohibited by it to the States, are reserved to the States respectively, or to the people. 
|
| Tenth Amendment |
Urban-rural differences remain important in health care. Senators Baucus, Grassley and Snowe come from sparsely settled states. Former Senator Daschle is from South Dakota; there are perhaps twenty states potentially in this category. With a sparse population, it is difficult to develop sufficient insurance business for the law of large numbers to establish actuarial safety; these states need to combine into regional areas to reduce the competitive size of their loss reserves. On the other hand, populous states like New York, California, etc. are often adamantly opposed to regional groupings, for opposite reasons. These population disparities create differing attitudes about modifying the 1945 McCarran Ferguson Act, which limits federal insurance regulation and enables state regulation, thereby making it difficult for small states to agree to interstate health insurance sales and portability. The fact that large employers have already achieved this freedom through ERISA also makes them unwilling to see the problem or waste political capital achieving it for others. And thereby diminishes the power of low-population states to resist national healthcare insurance, which is their natural position.
And finally, Obamacare raises some questions about judicial remedies. Certain Op-Ed commentators have raised a question of the constitutionality of federal mandates or pre-emptions of state laws, depending on how they are phrased. The U.S. Constitution was only narrowly ratified in 1789, in large part because the states were fearful of the federal government getting bigger and more powerful than necessary. In response to this strong feeling, the Tenth Amendment reinforces in no ambiguous words, that anything not specifically assigned to the national government is to be in the province of the state or local governments. If ever there was original intent, it was that one.
REFERENCES
| Never Enough: America's Limitless Welfare State | amazon |
Reforming Health Reform, New Jersey Style
 |
| Congressman Robert Andrews |
A single e-mail to constituents, and no other communication visible to the general public, announced a town hall meeting with our Congressman, Bob Andrews, on the campus of Rowan University, from 6 to 8 PM, August 24, 2009. The subject was to be Health Care Reform Legislation. On arrival, it was hard to find the auditorium in the square mile of new college campus, and only a small sign entitled "Event" indicated the place to park. Lots of cars.
By counting seats in a row and multiplying by the number of rows, the University Auditorium held 3000 people, but at 6 PM it was difficult to find a vacant seat. The doors were almost blocked by two lines of people standing to speak at microphones in the center of the hall, snaking all the way out past the television cameras and then out the door. These people were strangely silent, preoccupied but not rude, apparently rehearsing their speeches. In the lobby outside the doors, several workers were distributing posters showing "Thank You!", checking people off on lists of some sort. Many of those who got posters were wearing red T-shirts emblazoned with something or other.
 |
| Rowan University |
When I finally got a seat inside, it was behind a whole row of such T-shirted poster-holders, mostly but not entirely of the black race. The Congressman was giving a little speech to the effect that he was one of the committee members who wrote the bill, so of course, he had to support it. Strange, that as a member of Commerce and Labor he was working on a bill which traditionally is the province of the Subcommittee on Health, of the Ways and Means Committee. In any event, that gave him the ability to explain some of the languages which were a little too hard to understand. Several in the audience shouted out something unintelligible at that point, but mostly the audience sat in silence, waiting for the questions. He soon opened it up for questions, because he wanted to know what his constituents were thinking.
Although a few inevitably wandered off the point, questioners were confident, moderately deferential, remarkably effective. No matter how it was stated, and no matter how it began ("I have always voted for you, Congressman"), they were at the microphone to run a sword into him. To some extent, posting the entire bill on the Internet had changed politics. One old man, reading from his papers, said that page 343 says, etc; to which the harassed Congressmen blurted out, "That isn't true!" But the old man held his ground, "Oh, yes, and what else isn't true, that's written in the bill?"
Our congressman represents a working-class district, as clearly illustrated by his previously running for Congress without opposition. In searching for the reason this solidly Democrat audience was so antagonized, one gathers they generally have Unionized health benefits and feel threatened that ensuring the "illegals" will be paid for by impairing their own insurance. Somehow they feel that anyone who denies it is lying to them. ("It isn't what's in the bill, it's what will be in the bill ten years from now.") Except for college professors, Union members have the most luxurious health insurance coverage in America and are accustomed to boasting of it. Somehow, this privileged position drowns out their envy of rich people. When told that only the top x% of the country would have its taxes raised, one man bore right in on the Congressman. "You never heard anyone asking a poor man to give him a job". (Yeah, right, right on, Yeah.)
Although the people in red shirts holding posters put up a fight for fifteen minutes or so, they soon subsided out of recognition of who "owned" the room, and the remaining three hours of "questions" were almost uniformly negative. After an hour, the television cameras left the room, and at that signal, the people in front of me wearing red shirts also left. After a succession of speakers praised physicians somewhat excessively, a couple of physicians got up and made a poor showing at the microphone. One of them, a fat woman, had the poor judgment to tell these folks that many diseases like diabetes were self-inflicted, but was to hear back that it would help if our President would himself stop smoking and leave the rest of us to mind our own business. Two women who proclaimed themselves single mothers were no better treated..
At 9:30, a meeting scheduled to end at 8 PM still had a thousand people in the audience, and fifty at the microphones. But I had enough. They made their point. All that remains is to see how fairly the television editors extract significant clips and to find out how the rest of the nation feels.
LATER FOOTNOTE: As matters turned out a few months later, this national legislation had more of a local New Jersey effect than the audience could have guessed. Mandating health insurance for 30 million uninsureds, Obamacare accomplished it for 15 million of them by forcing them into the state Medicaid program, which is widely acknowledged to be the worst program in American medicine, because it usually is the most under-funded. New Jersey residents are firmly opposed to anything which raised their already high local taxes and will focus intently on the attempt in the coming lame-duck session of Congress (November 2010) which intends to transfer federal money to states to pay for Medicaid, and which is given only the narrowest chance of success. Republican Governor Christie deftly split the industrial unions from the public sector unions with the remark, "Every time they get a raise, you get a tax increase." It was hard to answer.
Children, Playing With Matches

|
And now, after the President has signed a bill into law to be effective January 1, 2014, we have mandatory health insurance. Really? The word 'mandatory' is not easily found in a search engine search of the 450 sections of the Affordable Care Act, except for mandatory coding and reporting requirements, and perhaps some oblique references to what might possibly be required of newly mandated insurance enrollees, in case anyone is mandated. The operative term used in the statute to imply universal coverage is "Required minimum coverage", mostly deferred employer group plans for at least a year, particularly for those with more than 100 (formerly 50) full-time employees.
It is unclear what the Supreme Court decision limiting penalties to a small tax will do to this group, who temporarily (?) make up the largest proportion of people affected. They are also affected by more severe penalties for noncompliance, a dubious application of equal justice. What is mandated right now is that everyone who does not belong to a group plan, and who is not specifically excluded, must pay a tax if not insured. Shortly after the law was enacted, the U.S. Supreme Court specified the tax must be small, otherwise, it would be coercive. Two opposite suppositions are possible: by the time the large-employer deferment expires, either the burdensome penalties will be reduced, or else the present uproar will seem trivial by comparison with what will come next year. Seen from a distance, this law looks as though it was written with large employer groups in mind, and everything else was patchwork. If we discover later the patchwork is the whole system, the Affordable Care Act then assumes quite a different character from universal coverage, and probably should be remanded.
Let us accept the premise that this law was mostly intended to provide for those who have unusual difficulty obtaining or paying for health insurance. There were thought to be 30 million of them, probably more during an economic recession. What is the most cost-effective way to pay for ensuring this group? For practical purposes, most of the uninsured fall into three groups: criminals, mentally disordered, and illegal immigrants. Instead of disrupting the entire medical payment system, let us design three new programs, specifically aimed at the special problems of these three groups. They might not cover quite so many affected people, but tailor-made programs would probably do so more appropriately, get the job done more quickly (remember how long this process has already dragged on), and plausibly less expensively. By using block grants to the states, we might in time have the advantage of finding the best of several variations emerge.
Block grants may not be feasible in some of these areas, mostly because of politics, but for other reasons, too. In some ways, the prison population might prove to be the most difficult to make uniform, and while uniformity is not the highest priority, it has some value. Some regions tend to regard criminals as sick people who need treatment, while other regions regard criminals as outlaws who need punishment. Either way, costs may vary considerably, and frugal states do not enjoy subsidizing extravagant ones. In all states, criminal costs are unwelcome, so some states treat incarceration as a profit center, and first-class health care for convicted criminals is definitely not a goal. A wise Congressman avoids issues like this one, and block grants are probably the best solution. Obamacare excludes these people, entirely, even though there are 7 million of them.
A better case can be made for a health program for the 11 million illegal immigrants, but it comes down to much the same issue of local social attitudes affecting the politics, plus the fear that generous treatment will attract more immigration. A much better case can, therefore, be made for uniformity of federal subsidy, and by paying the subsidy directly to the healthcare provider, avoiding much of the political problems. Policing the borders is a national problem, and therefore the illegal immigrant health costs are a problem the federal government should absorb.
Mentally disordered people fall into several subgroups, but here the Federal Government is more fairly accused of making the problem worse, through closing the mental inpatient hospitals faster than drug therapy made it really feasible. Experience has shown that local treatment of mental disorder tends to be more generous and humane than remotely controlled reimbursement systems. When Congress became incensed at what seemed like exploitation of the DRG system, an overreaction was too harsh and business-like for a population that is by definition not completely responsible. The situation seems to call for a block grant program with a few incentives for state compliance with a limited set of standards.
In summary, if we look at the three main sources of clients among the uninsured, none of them seems suited for a national revision of care for the rest of the population. In fact, the generalization seems appropriate that they are highly unsuitable for a uniform national insurance program, pointing to higher costs and worse care if you approach them that way.
In fact, the political downside is worse. If you set about to do things without explaining why they aren't bizarre, people will assume you have some other motive than the one you offer.
Some regions of the country People in jail (there are about 7 million of them) are specifically excluded, and illegal aliens (at least 11 million) are indirectly excluded. Added to these two groups are those who will never be self-supporting because of developmental or acquired mental disorders. These three groups alone almost total of the forty million uninsured persons who were originally slated to be the main problem to be solved. It seems likely the specific and unique health financing problems of these three groups could have been better and less expensively addressed by devising three special programs for their specific problems (incarceration, non-citizenship, and mental defectiveness). In addition, 2 million members of (sic) Indian tribes are also excluded, and there are estimated to be 5 million persons potentially eligible for tribal membership. To stretch general health insurance to fit the unique difficulties of these admittedly difficult problem cases is far less likely to be satisfactory than directly aiming at them. And thus the trillion dollars extra cost estimate for the Affordable Care Act could likely have been better spent.
Just to take one of the three hard nuts, let's look at medical care for prisoners in custody. I have physician friends who are involved in prison medicine, and they are proud of the way they have suppressed medical costs to prisoners. Much of the problem revolves around the tendency to locate prisons in remote rural areas, where the quality of medical care is marginal, to begin with. But central to the issue is the determination of states to keep prison medicine inexpensive, no matter how anxious the rest of the nation is to upgrade the care. So state governments are not about to surrender control of the system to agencies which want to spend money. This isn't rocket science; the solution to this problem is more money, and not the kind of money that resembles Lucy holding the football until the last moment, then pulling it away. Prisons are tough places, with tough people in charge, and lots and lots of drug smuggling going on. Please let me know if you think there is anything in the Affordable Care Act which addresses these issues.
In fact, the briefest discussion of the three largest groups alone calls into question the wisdom of devising any program, insurance or otherwise, to apply to 100% of the population. Your author does not hate insurance, for healthcare or any other purpose. But few approaches will solve any problem for three hundred million people, for every day of their lives. We should thank the insurance industry for doing a good job for 90% of the public, and move on to other solutions for the last 10%. But in thanking them, they will pardon us for asking whether many of us would pay someone 10% to pay our bills for us, not counting the additional $10 billion income tax deduction we offer every year, to induce people and their employers to pay their bills. Why would anyone think insurance is cheap?
The most depressing feature of this issue is that it is likely to be repeated. If you believe as I do that the clever parliamentary tactics employed in its hybrid passage must have resulted in omitting some important features from the House Bill, and must have included many unwanted features in the Senate Bill which survived, then much more is to be uncovered, later. Unfortunately, a reading of the 450 surviving sections leaves the reader baffled as to which sections are central to the proposal, and which ones were included merely for window-dressing. At one time, the Administration may have thought this gave them a free hand to trade off superfluous baggage, but with the full text easily accessible to everyone, everyone can read it and continue to be annoyed by how it got there.
To aid in this process, we next print the table of contents, with section numbers. When the section number has been located, the full text of the statute can be displayed on any home computer, by entering the section number into the otherwise overwhelming text of the full Act. When risk corridors and other mysteries come up for discussion, it will generally be found that the matter reduces itself to a few sentences.
Text of AFFORDABLE CARE ACT, PL 111-148, March 23, 2010, Renamed HR 3590
The Real Obamacare, Unveiled

|
| Democratic Speaker Nancy Pelosi |
Even loyal Congressional Democrats demanded more explanation for passing Obamacare than they received. Democratic Speaker Nancy Pelosi implausibly explained, "We have to pass the bill in order to see what's in it." That didn't help very much.
An unexpected bungle of computerized insurance exchanges that didn't work, would soon confront Obamacare supporters with explaining things to a hostile public, instead of to a merely curious one. Instead of providing better insurance to thirty million people, many of whom did not have insurance, the Administration had to cope with the possibility of uselessly depriving several hundred million people of insurance that did satisfy them. And to do so past the deadline for renewal of their old programs, made several million suddenly anxious that newer products must somehow be worse, not better.
It was expedient politics to add new but more expensive mandatory features. But since many people could already choose a more expensive policy if they craved more features, the practical effect was usually to make insurance more expensive without providing anything new. Here, it also had the unwelcome appearance of extra cost paying for somebody else's subsidy. In any event, health insurance was certainly not cheaper.
Employees of big business were evidently particularly dissatisfied, so their arrangement will be announced later, probably after the elections. Two years after passage, the Affordable Care Act was still a work in progress, but it was hard to call it a victory.
|
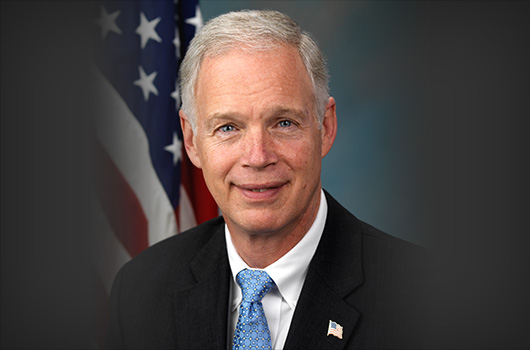
| Senator Ron Johnson |
Worse to come wasn't just an idle possibility. Millions of complacent people then received letters of cancellation (from their old, private insurance companies) in spite of specific provision in the law (section 1251) and repeated assurances from the President that this would never happen. Retired people on Medicare had mostly ignored Obamacare, which didn't apply to them. But any cancellation of existing benefits quickly revived anxiety that the real intention might be to pay for poor people (Obama's "base") with cuts in Medicare, which everyone over 65 had grown accustomed to receiving. A large new group was suddenly asking awkward questions.
Government workers and Congressmen definitely had to accept the new plans, probably to demonstrate shared sacrifice. That led Senator Johnson from Wisconsin to sue for damages because his constituency might think he really wanted to have it, in spite of nominal opposition. Big business received more extensions to its one-year postponement, which increasingly looked like a repeat of the 1994 Clintoncare experience where they had walked out, in a somewhat more obvious way. Small business was immediately refused similar relief, introducing concern about political favoritism, and conspiracies yet to be revealed. One of them surfaced a few months later, when "postponements" for employers with 50-100 employees were announced, effectively adding them to the definition of big business. Once more, there had been no such proposal in the enabling legislation. A majority of state governments refused to establish insurance exchanges, and an appreciable number of governors even refused to expand their Medicaid programs with Federal money. It could be argued that bribes that weren't permanent were essentially no different than direct coercion of states by the Federal Government, but were just a different method of revoking states rights under the Constitution.
Since it might be many years before deaths and retirements made it possible for insider biographies to explain everybody's true motive, the public applied the ancient Roman test of Cui bono? ("Who comes away from it, better off?") Everyone half expected the Obama base to be rewarded, and the Republican base to pay for it; but rewarding five percent at the expense of ninety-five percent, went beyond any election mandate, or even any tradition of the spoils system. Better medical care at cheaper prices always sounded over-optimistic. But worse care at a higher price now began to seem like the real outcome. Who comes away from that, better off?

|
| Republican Senator Scott Brown |
If a copy can be found, it certainly might be tempting to review the final original House bill and compare what was in it with the ultimate product (which was really just the Senate bill). But at that particular moment, there had been a Democratic majority, and that majority declared its preference for the Senate version. That is what the President signed. He then apparently hoped to solve its deficiencies by Executive Branch regulation, which might well lead to Constitutional lawsuit based on the "Vesting Clause" in Article 1 of the Constitution that, All legislative Powers herein granted shall be vested in a Congress of the United States, which shall consist of a Senate and House of Representatives. . When he subsequently did issue several dozen unauthorized regulations, the Speaker of the House of Representatives, John Boehner, announced his intention of filing a Constitutional suit in the Supreme Court. In a sense, that took matters back to Franklin Roosevelt's "Court Packing" uproar in the 1930s, with more or less the same issue of a President illegally delegating legislative power to an executive agency. This once proved to be a convulsive national issue. So this book deals with it in a later chapter, because the state legislatures got to the Supreme Court first in a related Constitutional matter.
|
| Democratic U.S. Sen. Edward Kennedy |
This uncertainty must be quickly resolved. The final law has over 450 sections, so some can be suppressed for a long time before an absence is noticed. The President's public restatement of section 1251 after the policies had already been canceled, remains particularly baffling. There are times when it almost seems the President was daring the Legislative branch to sue him. Although it is possible this maneuvering is more aimed at the Tea Party than the Democrats, it would certainly be the most dramatic Constitutional crisis since the Court-packing attempt in the 1930s. It deserves consideration in detail, but first, we must review the other Supreme Court action in the early days after passage of the Act, which may or may not have been the start of an elaborate collision of historic proportions. Preliminary conclusions must be reserved. Speaker Boehner may call off his suit after the outcomes of the 2014 Senate elections are known. International events may take a sudden turn. And the financial markets may still contain some surprises. More directly, there may be actions by the central actors in what Senators refer to as "this train wreck". In view of its potential destructiveness, the only consolation is it might at least inhibit Congress and the President from this particular maneuver a third time in the future.
Soon combined with a disastrously failed computer program for Insurance Exchanges making it impossible for the program even to get started, 2014 appears to be a bad year for tranquil discussion. It dramatized that trying to bully through was a bad choice. Millions of letters notified clients their old insurance was terminated as "inadequate" while the President continued to appear on television programs assuring such a thing would never happen, -- all of this projected a pretty poor image.Text of Section 1501, renamed Section 5000A: MINIMUM COVERAGE
SEC. 1501. REQUIREMENT TO MAINTAIN MINIMUM ESSENTIAL COVERAGE. (a) Findings- Congress makes the following findings: (1) IN GENERAL- The individual responsibility requirement provided for in this section (in this subsection referred to as the `requirement') is commercial and economic in nature, and substantially affects interstate commerce, as a result of the effects described in paragraph (2). (2) EFFECTS ON THE NATIONAL ECONOMY AND INTERSTATE COMMERCE- The effects described in this paragraph are the following: (A) The requirement regulates activity that is commercial and economic in nature: economic and financial decisions about how and when health care is paid for, and when health insurance is purchased. (B) Health insurance and health care services are a significant part of the national economy. National health spending is projected to increase from $2,500,000,000,000, or 17.6 percent of the economy, in 2009 to $4,700,000,000,000 in 2019. Private health insurance spending is projected to be $854,000,000,000 in 2009 and pays for medical supplies, drugs, and equipment that are shipped in interstate commerce. Since most health insurance is sold by national or regional health insurance companies, health insurance is sold in interstate commerce and claims payments flow through interstate commerce. (C) The requirement, together with the other provisions of this Act, will add millions of new consumers to the health insurance market, increasing the supply of, and demand for, health care services. According to the Congressional Budget Office, the requirement will increase the number and share of Americans who are insured. (D) The requirement achieves near-universal coverage by building upon and strengthening the private employer-based health insurance system, which covers 176,000,000 Americans nationwide. In Massachusetts, a similar requirement has strengthened private employer-based coverage: despite the economic downturn, the number of workers offered employer-based coverage has actually increased. (E) Half of all personal bankruptcies are caused in part by medical expenses. By significantly increasing health insurance coverage, the requirement, together with the other provisions of this Act, will improve financial security for families. (F) Under the Employee Retirement Income Security Act of 1974 (29 U.S.C. 1001 et seq.), the Public Health Service Act (42 U.S.C. 201 et seq.), and this Act, the Federal Government has a significant role in regulating health insurance which is in interstate commerce. (G) Under sections 2704 and 2705 of the Public Health Service Act (as added by section 1201 of this Act), if there were no requirement, many individuals would wait to purchase health insurance until they needed care. By significantly increasing health insurance coverage, the requirement, together with the other provisions of this Act, will minimize this adverse selection and broaden the health insurance risk pool to include healthy individuals, which will lower health insurance premiums. The requirement is essential to creating effective health insurance markets in which improved health insurance products that are guaranteed issue and do not exclude coverage of pre-existing conditions can be sold. (H) Administrative costs for private health insurance, which were $90,000,000,000 in 2006, are 26 to 30 percent of premiums in the current individual and small group markets. By significantly increasing health insurance coverage and the size of purchasing pools, which will increase economies of scale, the requirement, together with the other provisions of this Act, will significantly reduce administrative costs and lower health insurance premiums. The requirement is essential to creating effective health insurance markets that do not require underwriting and eliminate its associated administrative costs. (3) SUPREME COURT RULING- In United States v. South-Eastern Underwriters Association (322 U.S. 533 (1944)), the Supreme Court of the United States ruled that insurance is interstate commerce subject to Federal regulation. (b) In General- Subtitle D of the Internal Revenue Code of 1986 is amended by adding at the end the following new chapter: `CHAPTER 48--MAINTENANCE OF MINIMUM ESSENTIAL COVERAGE `Sec. 5000A. Requirement to maintain minimum essential coverage. `SEC. 5000A. REQUIREMENT TO MAINTAIN MINIMUM ESSENTIAL COVERAGE. `(a) Requirement To Maintain Minimum Essential Coverage- An applicable individual shall for each month beginning after 2013 ensure that the individual, and any dependent of the individual who is an applicable individual, is covered under minimum essential coverage for such month. `(b) Shared Responsibility Payment- `(1) IN GENERAL- If an applicable individual fails to meet the requirement of subsection (a) for 1 or more months during any calendar year beginning after 2013, then, except as provided in subsection (d), there is hereby imposed a penalty with respect to the individual in the amount determined under subsection (c). `(2) INCLUSION WITH RETURN- Any penalty imposed by this section with respect to any month shall be included with a taxpayer's return under chapter 1 for the taxable year which includes such month. `(3) PAYMENT OF PENALTY- If an individual with respect to whom a penalty is imposed by this section for any month-- `(A) is a dependent (as defined in section 152) of another taxpayer for the other taxpayer's taxable year including such month, such other taxpayer shall be liable for such penalty, or `(B) files a joint return for the taxable year including such month, such individual and the spouse of such individual shall be jointly liable for such penalty. `(c) Amount of Penalty- `(1) IN GENERAL- The penalty determined under this subsection for any month with respect to any individual is an amount equal to 1/12 of the applicable dollar amount for the calendar year. `(2) DOLLAR LIMITATION- The amount of the penalty imposed by this section on any taxpayer for any taxable year with respect to all individuals for whom the taxpayer is liable under subsection (b)(3) shall not exceed an amount equal to 300 percent the applicable dollar amount (determined without regard to paragraph (3)(C)) for the calendar year with or within which the taxable year ends. `(3) APPLICABLE DOLLAR AMOUNT- For purposes of paragraph (1)-- `(A) IN GENERAL- Except as provided in subparagraphs (B) and (C), the applicable dollar amount is $750. `(B) PHASE IN- The applicable dollar amount is $95 for 2014 and $350 for 2015. `(C) SPECIAL RULE FOR INDIVIDUALS UNDER AGE 18- If an applicable individual has not attained the age of 18 as of the beginning of a month, the applicable dollar amount with respect to such individual for the month shall be equal to one-half of the applicable dollar amount for the calendar year in which the month occurs. `(D) INDEXING OF AMOUNT- In the case of any calendar year beginning after 2016, the applicable dollar amount shall be equal to $750, increased by an amount equal to-- `(i) $750, multiplied by `(ii) the cost-of-living adjustment determined under section 1(f)(3) for the calendar year, determined by substituting `the calendar year 2015' for `the calendar year 1992' in subparagraph (B) thereof. If the amount of any increase under clause (i) is not a multiple of $50, such increase shall be rounded to the next lowest multiple of $50. `(4) TERMS RELATING TO INCOME AND FAMILIES- For purposes of this section-- `(A) FAMILY SIZE- The family size involved with respect to any taxpayer shall be equal to the number of individuals for whom the taxpayer is allowed a deduction under section 151 (relating to allowance of a deduction for personal exemptions) for the taxable year. `(B) HOUSEHOLD INCOME- The term `household income' means, with respect to any taxpayer for any taxable year, an amount equal to the sum of-- `(i) the modified gross income of the taxpayer, plus `(ii) the aggregate modified gross incomes of all other individuals who-- `(I) were taken into account in determining the taxpayer's family size under paragraph (1), and `(II) were required to file a return of tax imposed by section 1 for the taxable year. `(C) MODIFIED GROSS INCOME- The term `modified gross income' means gross income-- `(i) decreased by the amount of any deduction allowable under paragraph (1), (3), (4), or (10) of section 62(a), `(ii) increased by the amount of interest received or accrued during the taxable year which is exempt from the tax imposed by this chapter, and `(iii) determined without regard to sections 911, 931, and 933. `(D) POVERTY LINE- `(i) IN GENERAL- The term `poverty line' has the meaning given that term in section 2110(c)(5) of the Social Security Act (42 U.S.C. 1397jj(c)(5)). `(ii) POVERTY LINE USED- In the case of any taxable year ending with or within a calendar year, the poverty line used shall be the most recently published poverty line as of the 1st day of such calendar year. `(d) Applicable Individual- For purposes of this section-- `(1) IN GENERAL- The term `applicable individual' means, with respect to any month, an individual other than an individual described in paragraph (2), (3), or (4). `(2) RELIGIOUS EXEMPTIONS- `(A) RELIGIOUS CONSCIENCE EXEMPTION- Such term shall not include any individual for any month if such individual has in effect an exemption under section 1311(d)(4)(H) of the Patient Protection and Affordable Care Act which certifies that such individual is a member of a recognized religious sect or division thereof described in section 1402(g)(1) and an adherent of established tenets or teachings of such sect or division as described in such section. `(B) HEALTH CARE SHARING MINISTRY- `(i) IN GENERAL- Such term shall not include any individual for any month if such individual is a member of a health care sharing ministry for the month. `(ii) HEALTH CARE SHARING MINISTRY- The term `health care sharing ministry' means an organization-- `(I) which is described in section 501(c)(3) and is exempt from taxation under section 501(a), `(II) members of which share a common set of ethical or religious beliefs and share medical expenses among members in accordance with those beliefs and without regard to the State in which a member resides or is employed, `(III) members of which retain membership even after they develop a medical condition, `(IV) which (or a predecessor of which) has been in existence at all times since December 31, 1999, and medical expenses of its members have been shared continuously and without interruption since at least December 31, 1999, and `(V) which conducts an annual audit which is performed by an independent certified public accounting firm in accordance with generally accepted accounting principles and which is made available to the public upon request. `(3) INDIVIDUALS NOT LAWFULLY PRESENT- Such term shall not include an individual for any month if for the month the individual is not a citizen or national of the United States or an alien lawfully present in the United States. `(4) INCARCERATED INDIVIDUALS- Such term shall not include an individual for any month if for the month the individual is incarcerated, other than incarceration pending the disposition of charges. `(e) Exemptions- No penalty shall be imposed under subsection (a) with respect to-- `(1) INDIVIDUALS WHO CANNOT AFFORD COVERAGE- `(A) IN GENERAL- Any applicable individual for any month if the applicable individual's required contribution (determined on an annual basis) for coverage for the month exceeds 8 percent of such individual's household income for the taxable year described in section 1412(b)(1)(B) of the Patient Protection and Affordable Care Act. For purposes of applying this subparagraph, the taxpayer's household income shall be increased by any exclusion from gross income for any portion of the required contribution made through a salary reduction arrangement. `(B) REQUIRED CONTRIBUTION- For purposes of this paragraph, the term `required contribution' means-- `(i) in the case of an individual eligible to purchase minimum essential coverage consisting of coverage through an eligible employer-sponsored plan, the portion of the annual premium which would be paid by the individual (without regard to whether paid through salary reduction or otherwise) for self-only coverage, or `(ii) in the case of an individual eligible only to purchase minimum essential coverage described in subsection (f)(1)(C), the annual premium for the lowest cost bronze plan available in the individual market through the Exchange in the State in the rating area in which the individual resides (without regard to whether the individual purchased a qualified health plan through the Exchange), reduced by the amount of the credit allowable under section 36B for the taxable year (determined as if the individual was covered by a qualified health plan offered through the Exchange for the entire taxable year). `(C) SPECIAL RULES FOR INDIVIDUALS RELATED TO EMPLOYEES- For purposes of subparagraph (B)(i), if an applicable individual is eligible for minimum essential coverage through an employer by reason of a relationship to an employee, the determination shall be made by reference to the affordability of the coverage to the employee. `(D) INDEXING- In the case of plan years beginning in any calendar year after 2014, subparagraph (A) shall be applied by substituting for `8 percent' the percentage the Secretary of Health and Human Services determines reflects the excess of the rate of premium growth between the preceding calendar year and 2013 over the rate of income growth for such period. `(2) TAXPAYERS WITH INCOME UNDER 100 PERCENT OF POVERTY LINE- Any applicable individual for any month during a calendar year if the individual's household income for the taxable year described in section 1412(b)(1)(B) of the Patient Protection and Affordable Care Act is less than 100 percent of the poverty line for the size of the family involved (determined in the same manner as under subsection (b)(4)). `(3) MEMBERS OF INDIAN TRIBES- Any applicable individual for any month during which the individual is a member of an Indian tribe (as defined in section 45A(c)(6)). `(4) MONTHS DURING SHORT COVERAGE GAPS- `(A) IN GENERAL- Any month the last day of which occurred during a period in which the applicable individual was not covered by minimum essential coverage for a continuous period of fewer than 3 months. `(B) SPECIAL RULES- For purposes of applying this paragraph-- `(i) the length of a continuous period shall be determined without regard to the calendar years in which months in such period occur, `(ii) if a continuous period is greater than the period allowed under subparagraph (A), no exception shall be provided under this paragraph for any month in the period, and `(iii) if there is more than 1 continuous period described in subparagraph (A) covering months in a calendar year, the exception provided by this paragraph shall only apply to months in the first of such periods. The Secretary shall prescribe rules for the collection of the penalty imposed by this section in cases where continuous periods include months in more than 1 taxable year. `(5) HARDSHIPS- Any applicable individual who for any month is determined by the Secretary of Health and Human Services under section 1311(d)(4)(H) to have suffered a hardship with respect to the capability to obtain coverage under a qualified health plan. `(f) Minimum Essential Coverage- For purposes of this section-- `(1) IN GENERAL- The term `minimum essential coverage' means any of the following: `(A) GOVERNMENT SPONSORED PROGRAMS- Coverage under-- `(i) the Medicare program under part A of title XVIII of the Social Security Act, `(ii) the Medicaid program under title XIX of the Social Security Act, `(iii) the CHIP program under title XXI of the Social Security Act, `(iv) the TRICARE for Life program, `(v) the veteran's health care program under chapter 17 of title 38, United States Code, or `(vi) a health plan under section 2504(e) of title 22, United States Code (relating to Peace Corps volunteers). `(B) EMPLOYER-SPONSORED PLAN- Coverage under an eligible employer-sponsored plan. `(C) PLANS IN THE INDIVIDUAL MARKET- Coverage under a health plan offered in the individual market within a State. `(D) GRANDFATHERED HEALTH PLAN- Coverage under a grandfathered health plan. `(E) OTHER COVERAGE- Such other health benefits coverage, such as a State health benefits risk pool, as the Secretary of Health and Human Services, in coordination with the Secretary, recognizes for purposes of this subsection. `(2) ELIGIBLE EMPLOYER-SPONSORED PLAN- The term `eligible employer-sponsored plan' means, with respect to any employee, a group health plan or group health insurance coverage offered by an employer to the employee which is-- `(A) a governmental plan (within the meaning of section 2791(d)(8) of the Public Health Service Act), or `(B) any other plan or coverage offered in the small or large group market within a State. Such term shall include a grandfathered health plan described in paragraph (1)(D) offered in a group market. `(3) EXCEPTED BENEFITS NOT TREATED AS MINIMUM ESSENTIAL COVERAGE- The term `minimum essential coverage' shall not include health insurance coverage which consists of coverage of excepted benefits-- `(A) described in paragraph (1) of subsection (c) of section 2791 of the Public Health Service Act; or `(B) described in paragraph (2), (3), or (4) of such subsection if the benefits are provided under a separate policy, certificate, or contract of insurance. `(4) INDIVIDUALS RESIDING OUTSIDE UNITED STATES OR RESIDENTS OF TERRITORIES- Any applicable individual shall be treated as having minimum essential coverage for any month-- `(A) if such month occurs during any period described in subparagraph (A) or (B) of section 911(d)(1) which is applicable to the individual, or `(B) if such individual is a bona fide resident of any possession of the United States (as determined under section 937(a)) for such month. `(5) INSURANCE-RELATED TERMS- Any term used in this section which is also used in title I of the Patient Protection and Affordable Care Act shall have the same meaning as when used in such title. `(g) Administration and Procedure- `(1) IN GENERAL- The penalty provided by this section shall be paid upon notice and demand by the Secretary, and except as provided in paragraph (2), shall be assessed and collected in the same manner as an assessable penalty under subchapter B of chapter 68. `(2) SPECIAL RULES- Notwithstanding any other provision of law-- `(A) WAIVER OF CRIMINAL PENALTIES- In the case of any failure by a taxpayer to timely pay any penalty imposed by this section, such taxpayer shall not be subject to any criminal prosecution or penalty with respect to such failure. `(B) LIMITATIONS ON LIENS AND LEVIES- The Secretary shall not-- `(i) file notice of lien with respect to any property of a taxpayer by reason of any failure to pay the penalty imposed by this section, or `(ii) levy on any such property with respect to such failure.'. (c) Clerical Amendment- The table of chapters for subtitle D of the Internal Revenue Code of 1986 is amended by inserting after the item relating to chapter 47 the following new item: `Chapter 48--Maintenance of Minimum Essential Coverage.'. (d) Effective Date- The amendments made by this section shall apply to taxable years ending after December 31, 2013. SEC. 1502. REPORTING OF HEALTH INSURANCE COVERAGE. (a) In General- Part III of subchapter A of chapter 61 of the Internal Revenue Code of 1986 is amended by inserting after subpart C the following new subpart: `Subpart D--Information Regarding Health Insurance Coverage `Sec. 6055. Reporting of health insurance coverage. `SEC. 6055. REPORTING OF HEALTH INSURANCE COVERAGE. `(a) In General- Every person who provides minimum essential coverage to an individual during a calendar year shall, at such time as the Secretary may prescribe, make a return described in subsection (b). `(b) Form and Manner of Return- `(1) IN GENERAL- A return is described in this subsection if such return-- `(A) is in such form as the Secretary may prescribe, and `(B) contains-- `(i) the name, address, and TIN of the primary insured and the name and TIN of each other individual obtaining coverage under the policy, `(ii) the dates during which such individual was covered under minimum essential coverage during the calendar year, `(iii) in the case of minimum essential coverage which consists of health insurance coverage, information concerning-- `(I) whether or not the coverage is a qualified health plan offered through an Exchange established under section 1311 of the Patient Protection and Affordable Care Act, and `(II) in the case of a qualified health plan, the amount (if any) of any advance payment under section 1412 of the Patient Protection and Affordable Care Act of any cost-sharing reduction under section 1402 of such Act or of any premium tax credit under section 36B with respect to such coverage, and `(iv) such other information as the Secretary may require. `(2) INFORMATION RELATING TO EMPLOYER-PROVIDED COVERAGE- If minimum essential coverage provided to an individual under subsection (a) consists of health insurance coverage of a health insurance issuer provided through a group health plan of an employer, a return described in this subsection shall include-- `(A) the name, address, and employer identification number of the employer maintaining the plan, `(B) the portion of the premium (if any) required to be paid by the employer, and `(C) if the health insurance coverage is a qualified health plan in the small group market offered through an Exchange, such other information as the Secretary may require for the administration of the credit under section 45R (relating to credit for employee health insurance expenses of small employers). `(c) Statements To Be Furnished to Individuals With Respect to Whom Information Is Reported- `(1) IN GENERAL- Every person required to make a return under subsection (a) shall furnish to each individual whose name is required to be set forth in such return a written statement showing-- `(A) the name and address of the person required to make such return and the phone number of the information contact for such person, and `(B) the information required to be shown on the return with respect to such individual. `(2) TIME FOR FURNISHING STATEMENTS- The written statement required under paragraph (1) shall be furnished on or before January 31 of the year following the calendar year for which the return under subsection (a) was required to be made. `(d) Coverage Provided by Governmental Units- In the case of coverage provided by any governmental unit or any agency or instrumentality thereof, the officer or employee who enters into the agreement to provide such coverage (or the person appropriately designated for purposes of this section) shall make the returns and statements required by this section. `(e) Minimum Essential Coverage- For purposes of this section, the term `minimum essential coverage' has the meaning given such term by section 5000A(f).'. (b) Assessable Penalties- (1) Subparagraph (B) of section 6724(d)(1) of the Internal Revenue Code of 1986 (relating to definitions) is amended by striking `or' at the end of clause (xxii), by striking `and' at the end of clause (xxiii) and inserting `or', and by inserting after clause (xxiii) the following new clause: `(xxiv) section 6055 (relating to returns relating to information regarding health insurance coverage), and'. (2) Paragraph (2) of section 6724(d) of such Code is amended by striking `or' at the end of subparagraph (EE), by striking the period at the end of subparagraph (FF) and inserting `, or' and by inserting after subparagraph (FF) the following new subparagraph: `(GG) section 6055(c) (relating to statements relating to information regarding health insurance coverage).'. (c) Notification of Nonenrollment- Not later than June 30 of each year, the Secretary of the Treasury, acting through the Internal Revenue Service and in consultation with the Secretary of Health and Human Services, shall send a notification to each individual who files an individual income tax return and who is not enrolled in minimum essential coverage (as defined in section 5000A of the Internal Revenue Code of 1986). Such notification shall contain information on the services available through the Exchange operating in the State in which such individual resides. (d) Conforming Amendment- The table of subparts for part III of subchapter A of chapter 61 of such Code is amended by inserting after the item relating to subpart C the following new item: `subpart d--information regarding health insurance coverage'. (e) Effective Date- The amendments made by this section shall apply to calendar years beginning after 2013.Text of Section 1251 (H.R. 3590):PRESERVATION OF RIGHT
TO MAINTAIN EXISTING COVERAGE
SEC. 1251. PRESERVATION OF RIGHT TO MAINTAIN EXISTING COVERAGE.
(a) No Changes to Existing Coverage-
(1) IN GENERAL- Nothing in this Act (or an amendment made by this Act) shall be construed to require that an individual terminate coverage under a group health plan or health insurance coverage in which such individual was enrolled on the date of enactment of this Act.
(2) CONTINUATION OF COVERAGE- With respect to a group health plan or health insurance coverage in which an individual was enrolled on the date of enactment of this Act, this subtitle and subtitle A (and the amendments made by such subtitles) shall not apply to such plan or coverage, regardless of whether the individual renews such coverage after such date of enactment.
(b) Allowance for Family Members To Join Current Coverage- With respect to a group health plan or health insurance coverage in which an individual was enrolled on the date of enactment of this Act and which is renewed after such date, family members of such individual shall be permitted to enroll in such plan or coverage if such enrollment is permitted under the terms of the plan in effect as of such date of enactment.
(c) Allowance for New Employees To Join Current Plan- A group health plan that provides coverage on the date of enactment of this Act may provide for the enrolling of new employees (and their families) in such plan, and this subtitle and subtitle A (and the amendments made by such subtitles) shall not apply with respect to such plan and such new employees (and their families).
(d) Effect on Collective Bargaining Agreements- In the case of health insurance coverage maintained pursuant to one or more collective bargaining agreements between employee representatives and one or more employers that was ratified before the date of enactment of this Act, the provisions of this subtitle and subtitle A (and the amendments made by such subtitles) shall not apply until the date on which the last of the collective bargaining agreements relating to the coverage terminates. Any coverage amendment made pursuant to a collective bargaining agreement relating to the coverage which amends the coverage solely to conform to any requirement added by this subtitle or subtitle A (or amendments) shall not be treated as a termination of such collective bargaining agreement.
(e) Definition- In this title, the term 'grandfathered health plan' means any group health plan or health insurance coverage to which this section applies.
Proposal: Coordinate Sections 1501 and 1251
After adventures in Congress and the Supreme Court, the Affordable Care Act no longer says it creates mandatory health insurance. It has transformed into addition of Chapter 48 within Subtitle D of the Internal Revenue Code of 1986. As such, it creates a default minimum coverage requirement in Section 1501 (now renamed Section 5000A), recognizing three main exceptions. They are Religious Objectors, Illegal Residents, Incarcerated Persons, (plus a catch-all group of "Hardship Cases".) The total it comprises is about the same thirty million uninsured persons we started with, although they may be different people. This expedient patches over the difficulties created by the Supreme Court decision in XXXX v. Sibelius, but the implication seems to be that since everyone is required to pay taxes, everyone must have health insurance, but that really cannot be so. The largest exception would be those enrolled in Medicare, taxed, but not covered by the Affordable Care Act. Native Americans pose a different problem. The potential for other loopholes to appear is considerable, and further legislative modification is certainly more awkward. Congress will certainly be vexed to find that modification of the immigration laws implies a change in Obamacare eligibility, as well.
In Section 1251 there is an independent exception, which declares everyone who is satisfied with existing coverage is allowed to keep it. Many are surprised to read it there, and no doubt some would wish it would go away. It appears politically impossible to change it. But, when someone gets standing to sue, the Supreme Court will have to choose, and both political parties are fearful of what the Court might then decide. Section 1251 can easily be defended as a necessary step toward gradual transition into a massive new program. It can also be attacked as a Booby Trap, deliberately sabotaging a political victory. And it can be suspected of being one of those raisins deliberately placed in the Senate pudding, with plans that went astray when the death of Senator Kennedy made it impossible to remove it at the House-Senate Conference Committee. When the Supreme Court gets it, it will make little difference who included the provision, or why. With such a gun at its head, the Legislative Branch would be foolish not to seek a quiet resolution.
Let's begin by noticing that exempting some people from the law is exactly the same as allowing them to choose something else. Section 1251 defines a category of exceptions, but it does not affect the number of uninsured. People who do not wish to transfer might as well be added to incarcerated persons, illegal immigrants, and religious objectors, for all the difference it would make in the number of people covered. Since the largest insurance category of all, encompassing employees of large businesses, has been indefinitely postponed independently, it might actually be true that the size of the program could be reduced to more manageable proportions, but it is certainly no larger. For those looking for a workable face-saving way out of the present train wreck, consolidating the exemptions might create a basis for one. While the new coverage might be more comprehensive, it is only that difference in comprehensiveness which changes. As time gets closer to the elections, political damage from administering a failing program certainly gets worse, and "playing for the breaks" has less time to work. The dynamics from the other side of the table are harder to discern, but it is always good politics to rescue the nation from a looming threat.
Although there would certainly be many objections to consolidating the two sections of the APA, it is difficult to imagine other alternatives for this particular issue. Even ending the Cold War took a long time, when the two negotiators agreed on the goal. Perhaps surrendering to Justice Sutherland's historic doctrine that the whole law is "void for vagueness" is best seen as a nuclear option. The practical consequence of totally voiding Obamacare would be a return of health care to regulation by the States but without the benefits of conciliating the change. Beyond that, questions of interstate transfers of health insurance coverage might start with copying useful features from ERISA. To use an old phrase, this isn't rocket science; there aren't many significant differences between states, right now. But it may not be necessary to smash the Affordable Care Act to achieve more than smashing would achieve. We lived with state regulation of healthcare for centuries; we could do it again.
Accordingly, to get the ball rolling, it seems reasonable to Propose: That one or more Houses of Congress should reopen the ACA law for limited technical amendments, chiefly to add Section 1251 as an additional feature of Section 1501, thus making that entire section just one additional category of recognized exemption, from the minimum coverages in the new tax code.
Health Care and Education Reconciliation Act of 2010
Obamacare is actually the product of two laws, which is an interesting commentary on Congressional procedure, but merely a distraction from a comprehension of the health care reform. For completeness it is briefly summarized here.
Over the years, the ability of the Senate to filibuster important issues was hampered by potentially applying the filibuster to every vote taken. In particular, the Budget Act contained a vast number of changes to individual dollar authorizations, many of them surfacing at the last moment, after the final compromises had been made and everyone wanted to go home. So it was decided to make an exception for budget changes, but it called on Senator Byrd of West Virginia to devise language which would prevent tricky things for sliding through in the rush toward adjournment.
The result was the Byrd Rule, which defined permissible material for such special allowance. It did two things: it defined a permissible item for inclusion in budget reconciliation as one which was financial but did not change the total budget. The second thing it did was hedge this exception around with controls by the majority leader, right up to the ability of the majority leader to replace the Speaker and anyone else he felt was getting around the rule. The rules surrounding this matter were incorporated into the Congressional Budget Act of 1974, including a provision that there would only be one Budget Reconciliation Act per year. The volume of such technical amendments grew to be so great that there were multiple Reconciliation Acts, automatically incorporated into one big one by a special automatic amendment from the Rules Committee. That explains why the technical amendments to the Affordable Care Act are only part of the Health Care and Education Reconciliation Act of 2010, which was never intended to become law.
Many parts of the Affordable Care Act were thought to be suitable for this exclusion, particularly since the complete ACA did not fit completely within the requirements for filibuster protection. Pages of these technical amendments were added to a Reconciliation Bill mostly designed for the student loan program. Most readers will not find these numerous provisions contribute much to an understanding of what the Act actually does, or what it means. But you never know, for sure.
The President signed the Affordable Care Act on March 23, 2010. He signed the Health Care and Education Reconciliation Act a week later. When the Supreme Court handed down the NFIB v. Sibelius decision, further rearrangement of the indexing and wording became necessary to make the whole thing coherently unified as Chapter 48 of Subchapter D of the Internal Revenue Code of 1986. The whole episode is reminiscent of the epitaph of Leonidas, at Thermopylae.
Go tell the Spartans, passerby,
That here, obedient to their laws, we lie.
State and Federal Powers: Historical Review

|
| John Dickinson of Delaware |
It was expedient to leave certain phrases in the Constitution intentionally vague, but the overall design is clear enough. Just as twenty-eight sovereign European nations now struggle to form a European Union, thirteen formerly sovereign American colonies once struggled to unify for the stronger defense at a reduced cost. Intentionally or not, that created a new and unique culture, reliant on the constant shifting of power among friendly rivals. Everybody was a recent frontiersman, trusting, but suspicious. It still takes newcomers a while to get used to it.
So the primary reason for uniting thirteen colonies was for a stronger defense. As even the three Quaker colonies of New Jersey, Pennsylvania and Delaware could see, if you are strong, others will leave you alone. In time, the unification of many inconsequential behaviors created a common culture of important ones; and in time that common culture strengthened defense. At first, it seemingly made little practical difference locally whether construction standards, legal standards, language and education standards and the like were unified or not. Except, that in the aggregate, it forged a common culture.Returning to the Constitutional Convention, an additional feature was added to the tentative 1787 document to respond to protests from small component states. They objected that whatever the big-state motives might be, small states would always be dominated by populous ones with more congressmen if a unicameral Legislature is made up of congressmen elected by the population. Pennsylvania had recently had a bad experience with a unicameral legislature. So a compromise bicameral legislature (with differing electoral composition in the two houses) was added to protect small-state freedoms from big domineering neighbors. Even after the Constitution was agreed to and signed, the states in ratifying it still insisted on a Bill of Rights, especially the Tenth Amendment, elevating certain citizen prerogatives above any form of political infringement, by any kind of a majority. These particular points were "rights"; individuals were even to be insulated from their own local state government. The larger the power of government, the less they trusted it. John Dickinson of Delaware, the smallest state, soon made the essential point abundantly clear to a startled James Madison, when he pulled him aside in a corridor of Independence Hall, and uttered words to the effect of, "Do you want a Union, or don't you?", speaking on behalf of a coalition of small states. It was probably galling to Dickinson that Madison had never really considered the matter, and went about the Constitutional Convention airing the opinion that, of course, the big states would run things. Dickinson, who had been Governor of two states at once, had observed the effect of this attitude and wasn't going to have more of it.The practice of Medicine was certainly one of those occupations where it mattered very little whether we were a unified nation. Unification of medical care offered a few benefits, but mostly it didn't matter much, right up to 1920 or so. Even then I would offer the opinion, that unification of the several states (with consequent Free Trade) only made a big difference to health insurance, and still made little difference to the rest of medical care. In fact, there are still about fifteen states with too little population density to provide comfortable actuarial soundness for health insurance, as can readily be observed in the political behavior of their U.S. Senators. Although the number of low-population states gets smaller as the population grows, there are even so perhaps only ten big states where multiple health insurance companies can effectively compete within a single state border. Quite naturally the big-state insurers expect one day to eat up the small ones. By contrast, the nation as a whole, the gigantic population entity which Obamacare seeks to address, has far too many people spread out over far too large an area, to be confident we could unify them into one single program. Dividing the country into six or seven regions would be a much safer bet. That's the real message of the failure of the Computerized Insurance Exchanges -- far too much volume. And the coming failure of the Computerized Medical Record -- with too much complexity. With unlimited money, it can be done, because diseases are disappearing and computers are improving. But why struggle so hard?
It is at least fifteen years too early, and mostly serves the interest of insurance companies, if they can survive the experience. At the same time, we are at least fifteen years away from growing the smallest states to the point where we could decentralize. It's really a situation very similar to the one John Dickinson identified, James Madison briefly acknowledged, and where Benjamin Franklin improvised a solution. In their case, it was a bicameral legislature. In the case of medical care, it could be an administrative division of revenue from the expenditure. It could be the cure of a half-dozen chronic diseases. It could be six regional Obamacare. But creating one big national insurance company during a severe financial recession is something we will be lucky to survive.

|
| Delegates |
Benjamin Franklin, who for over 40 years had been working on a plan for a union of thirteen colonies (since 1745, long ago producing the first American political cartoon for the Albany Conference), devised the compromise. It was essentially a bicameral legislature -- with undiminished relative power in the Senate for small states. In this backroom negotiation, it was pretty clear Franklin held the support of two powerful but mostly silent big-state delegates, Robert Morris and George Washington. These were the three men of whom it could be said, the Revolution would never have been won without each of them. In 1787 they were still the dominant figures in diplomacy, finance, and the military. All three were deeply committed to a workable Union, each for somewhat different reasons. Now that a workable Union was finally within sight, parochial squabbles about states rights were not going to be allowed to destroy their dream of unity.
And so it comes about, they gave us a Federal government with a few enumerated powers, ruling a collection of state governments with regional power over everything else. And since big-state/small-state squabbles are unending, almost any other solution to some problem repeatedly, seemed preferable to disturbing what holds it all together. On the other hand, the Industrial Revolution was beginning at about the same time, and people who recognized the power of larger markets almost immediately set about attacking state-dominated arrangements, systematically weakening them for a century, and redoubling the attack during the Progressive era at the end of the 19th Century. Attacks on what seemed like an abuse of state power, the power to retain slavery, and later the power to perpetuate white racism, were claimed to justify this attrition of states rights. The ghost of the Civil War hung over all these arguments, restraining those who pushed them too far.
However, the driving force was industrialization, with enlarged businesses pushing back against the confinement of single-state regulation within a market that was larger than that. This restlessness with confining boundaries was in turn driven by railroads and the telegraph, improving communication and enlarging markets, which offered new opportunities to dominate state governments, and when necessary the political power weakens them. One by one, industries found ways to escape state regulation, although the insurance industry was the most resistant, whereas local tradesmen like physicians found it more congenial to side with state and local governments. The 1929 crash and the Franklin Roosevelt New Deal greatly accelerated this dichotomy, as did the two World Wars and the Progressive movement from Teddy Roosevelt to Woodrow Wilson. The Founding Fathers were said to have got what they wanted, which was a continuous tension between two forces, supporting both large and small governments; with neither of them completely winning the battle.

|
| Insurance Monopoly |
The medical profession further evolved from a small town trade into a prosperous profession during the 20th century, but the practice of medicine remained comfortably local. Even junior faculty members who move between medical schools quickly come to realize their national attitudes are somewhat out of touch with local realities. For doctors, state licensure and state regulation remained quite adequate, and state-regulated health insurance companies paid generously. State-limited health insurance companies had a somewhat less comfortable time of it, but the ferocity of state-limited insurance lobbying, as exemplified by the McCarran Ferguson Act, perpetuated it. The medical profession watched uneasily as the growth of employer-paid insurance extended the power of large employers over health insurance companies beyond state boundaries, and thus in turn over what had been medical profession's kingdom, the hospitals. And the medical profession also had to watch increasing congeniality with big government extend through businesses, unions and universities, fueled by overhead allowances of federal research grants and finally in 1965, federal health insurance programs. Nobody likes his regulator, but national organizations inevitably prefer a single regulator to fifty different ones. Furthermore, everybody could see that health care suddenly had lots of money, and naturally, everybody wanted some.
 There is nothing naturally inter-state about medical care -- except health insurance. 
|
To be fair about it, there was not a strong case for state regulation, either. It could have been argued that uniformity and reduced administrative costs favored central regulation over-dispersed control, because of improved efficiency; and few would have argued about it. Until the ACA insurance exchanges crashed of their own weight around the ears of hapless creators, that is, unable to do what Amazon seems to do every day, and raising quite a few embarrassing recollections. Recollections of the mess the Sherman Antitrust Act inflicted on local medical charity in Maricopa County, Arizona. Recollections of the "Spruce Goose" airplane that Howard Hughes made so big it couldn't fly. Recollections of the gigantic traffic jam strangling the District of Columbia every weekend. And, reminders that 2500 pages of legislation remain to be converted into 20,000 pages of regulations which it would take a lifetime to understand. Suddenly, let's face it, retaining state regulation of health care, or not rocking the boat, gets a lot better press. It might even work better than the national kind, especially in an environment where no one expected a perfect solution, and just about everyone had heard of the Curse of Bigness. When we first discovered that use of health insurance added 10% to the cost of health care, it had seemed like an easy place to extract 2% of the Gross Domestic Product for better things, just by streamlining administration. But after the health exchange fiasco, some people begin to wonder if 10% is just what it costs to use insurance to pay for healthcare. If that is the case, perhaps we should look at other ways of paying our bills, not just a different regulator. Nobody would pay 10% just to have his bills paid, if he understood what he was doing.
Obamacare's Constitutionality

|
| President Barack Obama |
Any idea of a smoothly orchestrated introduction of the new law was jarringly interrupted by the U. S. Supreme Court, which granted a hearing to a complaint by 26 State Attorney Generals, that the ACA Act was unconstitutional. It was big news that the whole Affordable Care Act might be set aside without selling a single policy of insurance. The timing (before the Act had actually been implemented) served to guarantee that the constitutional issue, and only that issue, would be discussed at this Supreme Court hearing. By implication, there might be more than one episode to these hearings.
While many could have declaimed for an hour without notes, about difficult issues perceived in the Obama health plan, questioning its constitutionality had scarcely entered most minds. Then of a sudden, near the end of March 2012, a case testing the constitutionality of mandatory health insurance was granted certiorari and very promptly argued for three full days before the U.S. Supreme Court. Twenty-six state attorneys general brought that case, so it was not trivial. In jest, one Justice quipped he would rather throw out the whole case than being forced to spend a year just reading 2500 pages of it. But Justices are practiced in the art of quickly getting to the heart of a matter; it soon boiled down to one issue: was it constitutional for Congress to force the whole nation to purchase health insurance? Is there no limit in the Constitution about what the federal government can force all citizens to do, even though the federal government itself is severely limited in scope? Even though the Tenth Amendment states that anything not specifically granted to the federal becomes the province of the states? Would a people who fought an armed revolution for eight years over a 2-cent tax on tea, now consent to a much larger requirement which it was not constitutionally authorized to impose? Most people finally wrapped their heads around some formulation of this non-medical concept to a point where they vaguely understood what the Judges were arguing about. This was beginning to look like a topic where We The People made a covenant with our elected leaders, and reserve the sole right to change it.
 The powers not delegated to the United States by the Constitution, nor prohibited by it to the States, are reserved to the States respectively, or to the people. 
|
| Tenth Amendment |
The Constitution describes a Federal system in which, a few enumerated powers are granted to the national government but every other power is reserved to the state legislatures. The Constitution had to be ratified by the states to go into effect, and the states had such strong reservations about the surrender of more than a handful of powers that they would not ratify the document unless the concept of enumeration was restated by the Tenth Amendment. If states could not be persuaded of the need for a particular power to be national, they might refuse to ratify a document which enabled permanent quarrels about the issue. That wariness explains why The Bill of Rights goes to the extra trouble of declaring certain powers are forbidden to any level of government.
Separation of powers further explains why Mr. Romney's mandatory health insurance plan might be legal for the Massachusetts legislature but prohibited to Congress. After Chief Justice Roberts got through with it, whether that truly remains the case will now depend on whether it is described as a tax, a penalty, a cost, or whatever, and only if the U.S. Supreme Court later agrees that was a proper definition. Because -- to be considered a tax it must be too small to be considered coercion. The law itself apparently does not underline this distinction in a way the Justices felt they could approve. Indeed, while Mr. Obama in his speeches firmly declared it was not a tax, later White House "officials" declared it might be. There was agreement the Federal government could tax, but no acknowledgment that taxes might have any purpose other than revenue.
Under circumstances widely visible on television, however, it was clear that the House of Representatives had been offered no opportunity to comment on this and many other points in this legislation. To a layman, that fact itself seems as clear a violation of constitutional intent as almost any other issue, since the Constitution indicates no idea was ever contemplated that any President might construct laws, nor like the courts, interpret their meaning. The first three Presidents repeatedly raised the question of whether they had the authority to do certain things we now take for granted. And Thomas Jefferson was similarly boxed in by a clever Chief Justice, who said, in effect, Agree to This Decision, or be Prepared to Get a Worse One. The Constitution says it is the function of the Executive branch to enforce the law, "faithfully". Presumably, all of the thousands of regulations issued by the Executive Branch under this law must meet the same test.
Given that the Justices now hold it constitutional for the federal Congress to mandate universal health insurance, based on some authority within taxation, the immediate next issue is paying for it. Millions of citizens, usually young and healthy but sometimes for religious reasons, do not want to buy health insurance and would be forced to do so by this law because the only available alternative is to pay a revenue tax. The purpose of including them is to overcharge people who will predictably under-use community-rated insurance, and thus enable the surplus to reduce costs for those who do want to buy health insurance. (Here, the Court had the pleasure of reducing an unusually opaque law to an unusually succinct summary.) To avoid the charge of a "taking", the Administration must either surrender on the universal mandatory point or else surrender the level premiums of community rating. The lawyers for the complaining attorneys general laid great stress on this particular issue in their arguments, and it occasioned much of the discussion from the bench. However, until the law is in action there is as yet no cause for damages.
Here it will depend on whether you call it a permissible activity for Massachusetts or for the Federal government. The Constitutional point seems to be that it is a legitimate Federal power to tax for the "general welfare", so it now becomes essential to know if the taxes for noncompliance in Obamacare are really a penalty. The Justices seemed to be questioning whether the whole scheme would collapse with the forced subsidy eliminated, and because of that be deemed to have been a "general welfare purpose" adequate to meet the constitutional requirement of a permissible enumerated purpose. Lawyers can generally find such a defined purpose in the words of the Constitution, even if they have to dip into the penumbras and emanations of the words. So the question might just devolve into whether a majority of the Justices wish to declare the penumbra to be within the enumerated powers of Congress. To all of this, the lawyers for the attorneys' general reply that such an enumerated power is impossible because there is no limit to what could be done by this method. Congress would then be allowed to mandate that everyone eat broccoli for dinner, or buy a General Motors car in order to pay for the deficits of rescuing that company from bankruptcy. Almost anything could be mandated by establishing a penalty called a tax; including a mandate that everyone buys a product in order to pay for the deficits of mandating it, illustrates there exists at least one circularity of enumerating something like a power of Congress. According to this reasoning, mandated health insurance cannot, therefore, be an enumerated power of Congress, either now or at any time in the future. The sort of speculative law outlined in this paragraph is exactly the sort of thing the Supreme Court dislikes and shows the utility of denying access to the courts to anyone who cannot claim "standing", defined as a claim of actual injury from a law.
The Justices undoubtedly had to weigh the fact that the American public has a strong distaste for this sort of convoluted reasoning, which sounds like a convention of Jesuit priests having fun. On many other occasions, however, the public has accepted the judgment of people it hired to understand this sort of thing; that's called respect for the law. Eighty years ago in the Roosevelt court-packing case, there was the same sort of collision between the Court and the President, and the Court knuckled under even though the public supported the Court. In both cases, the Court seemed to be yielding to the President, with the unspoken compromise that the President would not pursue his earlier course with quite so much vigor. Since the really central 1937 question of overturning the Interstate Commerce clause ("Commerce among the several states") was left unaddressed, the velvet glove might yet contain an iron fist.
Roberts the Second

President George W. Bush nominated John Roberts to be Chief Justice of the U.S. Supreme Court in 2005. Since then, the Chief's administrative changes to the court and the whole court system have been slow but methodical. To the extent the Chief Justice has control of the matter, Roberts has been taking steps which make the Court into a more thoughtful branch of the Federal Government, ultimately making it more powerful. His first step was to reduce the number of cases considered each year, constraining them to conflicts between lower jurisdictions, unless otherwise mandated. This year, the number of cases heard is about eighty, or only half of the previous numbers. The policy lets unconflicting Appellate judgments stand. A second court must disagree with the first one, for the Supreme Court to enter the case.
The so-called Obamacare case, (NFIB v. Sebelius), meets this conflict-between-jurisdictions standard, but is notable for other innovations. The case was nationally broadcast as a live slide show. It heard arguments lasting three days instead of the usual single hour, and of course, it broke new substantive ground in a case of national interest. The decisions will now get more press attention; but this relatively rapid evolution toward a national debating contest, through modified Court procedure, is more important than it looks. It would be saying too much to claim the whole nation now fully understands its Constitution of enumerated powers, but surely the citizens who have only recently learned something about it must number in the millions. Before this case, many law school graduates might have had difficulty describing the design of the federalized system in a plausible dinner-table conversation. It's not yet clear where John Roberts is going, but he is surely trying to bring the public along with him.
During the semi-televised arguments, I was at first impressed with the rapid-fire exchanges between Justices and litigators about the operation of health insurance. Some people are born with high-speed brains and high-speed speech apparatus; no doubt, such people are sought after to represent others in court. But after practicing Medicine for sixty years and writing books about health insurance, I recognized that several rapid-fire responses by the attorneys were confident but off-target. Frankly, if you only have a few minutes but many points to make, and have to say them before someone interrupts, you would almost have to be a circus freak to manage. This is quite unnecessary, no matter how entertaining it may be to other lawyers. There seems no reason why the questions cannot be submitted in writing, sometimes employing experts on the specific points, and allowing enough time without interruption to devise a thoughtful answer. At present, it seems to matter more what the litigating attorney will agree to, than what is the fact. The outcome of cutting a litigant off after he says, "Yes, your honor, but.." is now only to establish whether both sides agree on a point; just why they agree or disagree is not even sought, let alone disregarded. It would seem useful to know Justice Thomas' reasons for abstaining from questions during oral arguments, for a different sort of example. So, it is easy to imagine that John Roberts has some thoughtful goals in modifying Supreme Court traditions, and equally understandable if jurists of this distinction become irritated by suggestions from the peanut gallery. It is thus fitting that we all hold back and first watch where the varsity means to take us. But allowing the public to express an opinion, is not the same as lobbying for it.
The Obamacare Act was about 2600 pages long, and two years after the President signed the bill, more than half of the necessary regulations remain to be written. The Law is "not severable", which is to say individual pieces of it cannot be attacked in court, without potentially upsetting decisions made on other portions. As a consequence, both the good and bad parts could endure for a long time to come. Or, the whole thing could suddenly sink from sight, relatively quickly. If the Justices can tolerate it, this legislation with many "moving parts" could be in the courts for a long time to come. So, Justices will then find the rule Roberts has made, of only accepting conflicts between the jurisdictions, protects their time and patience. But in doing so it will shift most final judgments into the hands of the lower, appellate courts. The legal profession will like this quite a lot. It will be like the gratifying situation said to prevail when a commanding General decides to retire -- everybody down the line could get promoted one notch.
By artfully selecting cases to argue, there were here four points open to the decision. Only two of them eventually had bearing on the final outcome of this case, but the whole issue is not necessarily concluded. The first decision got the most attention, deciding that the penalty for not having health insurance could be read as just a tax, and therefore was legal for Congress to use as a Constitutional basis for making health insurance mandatory, as Roberts declared the "Commerce clause" was not. The distinguishing feature of a Congressional exaction which is "just a tax" appears to be whether it exceeds the expenditure intended; if it exceeds the expenditure it would presumably be punitive. Nothing had seemed more important to the Founding Fathers than to expand the ability of the national government to impose taxes to service war debts. To truncate this wish of George Washington and Robert Morris into a short-cut, "Congress has the right to tax", or conversely to expand its confining language into "Congress has the right to tax in order to make private health insurance compulsory" just points up that the only real purpose of taxes in Washington's day was to wage war, and that the purpose of allowable taxes probably would have been defined if other purposes had been foreseen. Someone could usefully point out that what the Constitution really means is that Congress has the right to tax for "defense and the general welfare", and challenge anyone to argue otherwise. One sees the clever hand of Gouverneur Morris fuzzing up that argument; are we to ignore the fungibility of money and ask whether Congress may spend money on the general welfare only if it is general? How about earmarks, for example, are they all for the general welfare?
However, to turn a blind eye toward interesting issues is apparently a price that must be paid for obtaining the right for the Chief Justice to write the majority opinion, which eventually slips in some language (in legal language, an obiter dictum) to the effect that , of course, you couldn't use the Commerce Clause to do that. Getting Justice Ruth Ginsburg to sign that will eventually sound like the box John Marshall constructed in Marbury v. Madison. If that obiter dictum is as heat-resistant as the opinions of the first Justice Roberts in Franklin Roosevelt's court-packing effort, then the Commerce Clause is likely to be off-limits for a long time. Of course, if Chief Justice Roberts had joined the other four conservatives he would still have been able to write the majority opinion, but in the opposite direction. Except of course for that inevitable political accusation: There you go again, you 5-4 conservatives.
The second decision, in this case, is the sleeper. Congressional managers in charge of writing the bill had finally decided they had no way to cover 40 million uninsured people, except by diverting fifteen million of them into what is acknowledged to be the absolutely worst part of the American medical system, the state Medicaid programs. And because many States Rights advocates were in charge of state Governor's offices, the Congressional bill-writers added what is now a fairly familiar prod to cooperation. That is, if a state refuses to take the extra Medicaid patients, it will lose all federal funds for existing clients of state Medicaid. This sort of coercive provision has become so standard in highway bills and other federal programs operating at the state level, that it was largely unnoticed in the 48 hours the Congress was given to examine 2600 pages of legislative provisions. This, however, is blackmail, said John Roberts, quite unallowable under the defined separation of powers of the Constitution, between the state and federal levels of government. Furthermore, if some state decides to accept the penalty, it could close the existing program for the poor and accept the subsidy for the middle class, thus enhancing their revenues and reducing their obligations to the poor. Congress must now devise new strategies for suggesting federal programs to the states, and probably will do so. But the financial blackmail strategy now has a permanent black eye, with a skeptical public eye on the alert for it. The ironic conclusion of all this comes from the Congressional Budget Office, which predicts we will end up with 30 million uninsured persons, anyway.
What's awkward about this was immediately pointed out by attorney Richard Epstein: it ignores the century-old precedent set by Chief Justice Taft. Writing about a Child Labor law, Taft created a Supreme Court precedent that the Constitutional taxing power of the national government may not be used to implement what cannot be implemented directly. We can now see an example within the borders of a single case, where the Constitutional taxing power provision is used to indicate an otherwise impermissible Obamacare, and a few pages later its use is forbidden in the case of Medicaid in order to accomplish a forbidden coercion. Locating the two issues in the same case decision helps make the distinction between using the taxing power for revenue, and using it to coerce obedience; the distinction grows as the magnitude of the tax grows, particularly after it exceeds the intended government expenditure. What is not emphasized is the basis for Chief Justice Roberts reversing the precedent set by Chief Justice Taft on the same topic a century earlier. He did it with the Obiter dictum, and yet he didn't exactly do it. The four liberal Justices who co-signed the decision are not in a position to dispute it, while the four conservative Justices may not wish to. In either direction, however, the vote of the current Chief Justice appears to be both decisive and subtle.
It remains to be seen whether the 'tax, not commerce' strategy was clever. If the tax approach proves to be durable, it presumably extends to a wide range of legislation since Roosevelt's New Deal. Already, its awkward features have emerged in renaming portions of Obamacare into Chapter 48 of Subtitle D of the Internal Revenue Code of 1986 (!). Any law student who tries to look that up is going to have a frustrating time. But on the other hand, sometimes you win by losing. If it should somehow not be a tax, it has already been excluded from the Commerce Clause, so it has no hook left in the Constitution on which to hang it. There's something in this whole wrangle which resembles the position of Germany and Japan after the Second World War. In spite of losing that war, those two nations seem to have prospered better than England and Russia, who lost their empires but are said to have won the war .
More Work for the U.S. Supreme Court: Revisit Maricopa
<The Judicial Branch took much of its present form from Chief Justice John Marshall, several decades after the Constitutional Convention of 1787. Somehow, the fact of being the last branch to set its boundaries gives the Judicial branch the last word in certain circumstances, including the possibility that its last word may need some reconsideration. Sometimes not, of course, since if the other two branches make a mistake, the Court can overturn them; but the other two branches can regain control by seeking to change the law. That's the sort of balanced power which the founding fathers envisioned. But if the Supreme Court itself makes a mistake, it remains pretty much a mistake in residence, until the Court itself re-examines the matter. It would be indelicate for anyone else to cite a list of examples of this observation, so they are usually taken up, one at a time. The example with the greatest application to Healthcare is the 1982 decision in State of Arizona v. Maricopa County Medical Society.
Maricopa County is where Phoenix is located, and its County Medical Society was one of the pioneers in what was then called Foundations for Medical Care. These were organizations in which local physicians took the lead in organizing and managing health insurance for the local community. There is no doubt the rules and policies of the Foundations were conceived and implemented by physicians, who felt empowered by the defects of health financing which they saw in daily practice. It is also true these physicians were impatient with both the government and the health insurance companies, who seemed to resist helping the sick poor by implying it violated a per se technicality intended for business corporations. And furthermore, on the topic of business corporations, they are not exactly an enumerated Constitutional power of the federal government. At the same time, "Foundation" physicians could easily see opportunities for reducing waste in the local hospitals which would only be exploited if physicians were in charge because physicians could usually judge the cost/benefit more readily. Having recently returned from World War II, these doctors knew that medical care could be excellent even without such a thing as health insurance, and indeed even when hospitals were only a collection of tents. Perhaps a few of them were overly influenced by the TV serial, "MASH", whose central theme is that if doctors take the lead and do the right thing, much can be forgiven. That's a sort of Hollywood restatement of the latitude of ancient Courts of Equity, intended to cover a situation where obvious harm exists, but no law exactly addresses it.

|
| The Maricopa Medical Society |
Accordingly, the "better sort" of a doctor in Arizona perceived that the respectable ones would readily consent to care for the poor at lower rates, whereas the shirkers in their midst would ruin things for everybody by refusing to do their fair share of pro bono work. Like labor unions, the doctors resented the free rider phenomenon. The idea of a two-class system of medical care was also abhorrent to them, however; if there wasn't enough money to spread around, a "good" doctor would just agree to lower his fees unilaterally. This moral quarrel often conflicts American business, which characteristically takes the view that it doesn't really matter what costs or taxes or burdens are imposed by the government. What matters is that competitors mostly agree to abide by the same handicaps. When handicaps are roughly equal, the difference between success and failure is -- talent. To a considerable degree, talent rising to the top summarizes the aspirations of the anti-trust statutes, where it is both a simultaneous source of cost escalation and price suppression. Physicians are ultimately expected to find their highest duty is fiducial to the patients' best interest, particularly when the main conflict is only a financial one. In the antitrust arena, particularly the per se violations, the difference between a business corporation and medical society is sufficiently wide to justify considerable professional latitude. As it is not, in the case of insurers, and as it only partly remains, in the case of hospitals. The Maricopa Medical Society responded with perhaps excessive enthusiasm to the challenge of making local sense out of the price-fixing dilemma, but it was never given the opportunity to make its case.
At one time, local healthcare costs were held down by imposing competition on the hospitals, treating insurance administration in particular as clerks to pay the bills, rather than as big business's cup-bearer of fairness in a naughty world. Needless to say, the hospitals and health insurers had long chafed at the ability of physicians to change hospitals, and the patients to change insurers when their Attorney General seemed to suspect a return to Robin Hood notions of a special right to defy the law. What disappeared was an ancient concept of professional latitude. In certain parts of the country, big business was already reconsidering its control of hospitals and insurers as their agents in both assuring low-cost medical care, and suppressing its cost. With the defeat of physicians by the Maricopa decision, plus the approaching withdrawal of big business, the way was opened for hospitals and insurance companies to go to war for monopoly control of their own finances. Thirty years later, hospitals and insurers are now universally merging, and applying monopoly controls to admit favored physicians as their employees. The Affordable Care Act is the mechanism by which the government means to control the victors, thus making government itself into the hidden battlefield. It's a far cry from leaving medical decisions in the hands of physicians and their patients, to chose the treatments, and to agree on the price.

|
| Sen. John Sherman |
The Attorney General of Arizona, himself a colorful character, soon brought suit for an anti-trust violation, since price-fixing had been declared a per se violation, or confession of the absence of competition. These were additions made to the Sherman Anti Trust Act by earlier Supreme Courts, who found that an Act first written on the back of an envelope was difficult to administer. Further strictures were imposed by the Clayton Anti-Trust Act, but these might be remedied by subsequent Congresses. The important consequence was that the District Court of Arizona found it quite unnecessary to hold a trial or hear the evidence. The Court found against the doctors entirely on the basis of a motion for summary judgment. The matter passed through the Court of Appeals to the Supreme Court, which on the theory that price fixing is price fixing, by a vote of 4 to 3, upheld the Arizona suit. All the way from a writ of summary judgment in a district court, to the United States Supreme Court, without formal examination of the facts.
Perhaps, strictly on lawyerisms, that was safely correct. But in terms of the effect on medical care, it won the war for control of hospitals and the insurance companies. Somehow it was interpreted to mean that a hospital or an insurance company might do a great number of things which were forbidden to organizations run by physicians. The consequence is that Foundations run by physicians were under constant threat of what might happen to them if they did what HMOs were seen to be doing every day. The whole Clinton health fracas revolved around this particular case and its implications. From the physician point of view, if you had medical training, you were disqualified from running an HMO, because a change of leadership shifted the antitrust issue to a different level for two identical organizations. And that was true even if the physician had been trained for the role, while the administrator had not. What was particularly galling was to be tarred with the same brush of antitrust whereas others would describe their identical behavior as self-disciplined in the public interest. Self-imposed financial restraint was taunted and abused by aspirants for the same job with the same temptations, with multi-million dollar incomes but without adherence to the same code of ethics. The joke is that after all the Clinton Healthcare Plan's uproar, the public decided they disliked HMO's intensely, mainly because they couldn't choose their own doctor, and the doctor was being hampered in doing what seemed professionally best for the patient. None of these legal issues had arisen for physician-run HMOs. While of course, that might happen, such disputes would be settled by physicians, using medical arguments, followed by a change in management if the medical community widely disagreed with the decision. The only substantial difference was that doctors were running one, but subservient in the other, and the Courts had found that when doctors were in charge it amounted to price-fixing between competitors.
It now remains for some case to be found and carried to the Supreme Court which would allow an examination of the facts of this matter, perhaps remanding the case back to the District Court to hold a trial. That would seem a bare minimum after thirty years, and it now no longer get precisely to the issue. Somehow, another way must be found to examine which of two rather extreme theories of the Wild Wild West needs to be laughed off. Either we must re-examine whether, always and everywhere, price-fixing is such an undiluted evil that it never even needs a trial. Or whether we should continue to lynch price-fixers, and declare that medical care is too important to be left to people trained in its complexities, even when disciplined by self-interest in the exercise of its power.

|
| Henry J. Kaiser |
While on the subject of mixing business practices with professional standards, we might as well direct judicial attention to the unfair and probably unconstitutional (equal justice) tax preference for employers who purchase health insurance for their employees. An unnecessary grievance is created for millions of self-employed and unemployed people. Now seventy years old, this grievance has dubious evasions at its historical origin, has resisted multiple efforts for repeal, and benefits only one large group: big business. Henry Kaiser claimed he had difficulty attracting employees to his war industries because of wartime wage and price controls. Persuading the War Production Board to look the other way, he cloaked inducements to employees as something other than employee compensation. The fringe-benefits circumvention has since grown entirely out of control but is fiercely defended by business and union interests. As it grows, however, the inequity for the self-employed and unemployed to remain excluded from it also grows. Instead of addressing this problem directly, it might well be conjectured that recent regulatory attempts at forcing individual policies into group policy eligibility might be a way of exacting a price for cooperation, and for lobbying silence.
Summary of the Maricopa Case
From a legal standpoint, the uncomfortable feature of the case of the Maricopa Medical Society is that it went all the way to the Supreme Court without any trial of the facts or real opportunity for the defendants to present their case. That is, the whole HMO movement was effectively removed from the hands of physicians by a motion for summary judgment, on a Supreme Court decision, 4 to 3.
To hold a trial of the facts by remanding the case for trial, would seem to be the only way to introduce the defense that the doctors would have made. It is improper to suggest to their lawyers what the defense should be, but certain facts are now public knowledge. The Medicaid Act was passed in 1965, requiring state consent for a joint program. By 1972, Arizona was the only remaining state not to have agreed to Medicaid, which by then was widely recognized as the worst medical program in America. In 1982, Arizona adopted a small portion of Medicaid, and it was only in 1988 that it fully adopted the program. In 2001, Arizona's governor was offered 7.9 billion dollars over four years, as matching money for the insurance exchange feature of the Affordable Care Act. The governor recommended to the Legislature that they accept the offer because at least it was "better than Medicaid". There can be little doubt the Legislature of Arizona was adamant on the issue.
What were the doctors expected to do with the sick poor people? No doubt, there was a wide divergence of opinion, but it seemed likely only a handful of saintly volunteers would come forward, and none of them would be able to afford to pay hospitals what it cost. They felt that only by bullying a substantial majority to take the cases would it work, and the only weapon they had was to make it a condition for membership in the medical society.
Under these contentious circumstances, surely the Supreme Court could find some words to create a better outcome. Price fixing is a per se violation of the act, and there is little doubt that all HMOs fix prices. But only a physician-run HMO could be accused of fixing prices for competitive reasons, although it is arguably how strongly they would compete for indigent patients. The Supreme Court may be reluctant to overrule the price-fixing part, and the Arizona politics of this case are surely thorny. But at least the Court could find some clarifying language about physician-run HMOs. The opportunistic response of the non-physician-run HMOs was to exploit the opportunity to eliminate the competition of physician-run groups. In the meantime, HMOs run by non-physicians have become contentious in the extreme, whereas the earlier physician-run ones were tolerated by most physicians, and embraced by quite a few. The matter is one of the important threads in the Obamacare controversy, so the Supreme Court has an opportunity to improve quite a few situations by writing a clarifying paragraph or two.
What Can Supreme Court(s) Do About Tort Reform?
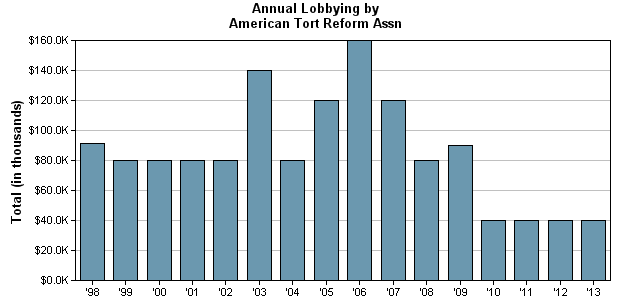
|
| Tort Reform |
For the better part of twenty-five years, I was a member of several physician study groups assigned to find some solution to the malpractice crisis. During that time, all manner of solutions were suggested or even tried out, and it would be my observation that only one of them seemed to work. That exception was a restraint on "pain and suffering" awards. In the past, we had tried arbitration panels, blue ribbon courts, and a wide range of proposals from the defense bar, designed to help them win cases. Nothing seemed to help the situation, which was always the number one complaint from surgeons, until California imposed a $250,000 cap on damages for pain and suffering and both awards and damage suits dropped significantly. That's legal jargon for a top limit to the amount of an award for pain and suffering, imposed on top of 'economic' damages, which are the awards for medical treatments actually incurred by the plaintiff. In the course of these discussions, I learned that it was customary to make these awards for non-economic damages based on medical costs. "Seven times the medicals" would be a typical offer in a negotiated settlement.
The history of this curious approach seems to have been the appeal to the judge, that if only economic costs were considered, the patient still would not be made whole, because the award would not cover his legal costs, which were usually 25-50% of the total, on a contingency basis. That is, the lawyer offered to work free of charge if he lost, but got 25-50% of the award if he won. From other investigations, I had discovered how hotly the trial lawyers would defend the contingency system, passionately proclaiming it allowed a poor man to have his day in court, so I tried to avoid that argument. My focus was, and is, that seven times the medicals are a somewhat overgenerous response to legal costs of a quarter to a half of the medicals. And it would be my surmise that the drop in California lawsuits following a limitation to awards for pain and suffering, reflected the fact that suits had been attractive at the overgenerous seven times level, but became unattractive when they declined to a more reasonable level. Stimulated by such surmises, it took very little investigation to discover that almost all high-figure awards were fairly exclusively for pain and suffering, while only a negligible amount of awards are for economic damages. Nuisance suits are in a different category, based on the insurance company estimate that a flurry of motions can usually run the defense costs up to the point where it is cheaper to settle than to defend a meritorious case. But even nuisance cases serve the purpose of paying to investigate a case, where it can be judged that ten nuisance cases may uncover one which has enough emotional appeal to a jury, to take a chance on trying the case. Therefore, a negotiated settlement of this issue between the two professions might justify a cap on pain and suffering, plus investigative costs of contingency cases equal to the economic damages.

|
| Malpractice |
That's the solution that appeals to me, but it does not propose a way to accomplish it. To argue this compromise with representatives of the trial bar is a waste of time unless they are threatened with some other solution which seems worse to them. As long as physicians are protected by insurance, they will not fight hard enough for any solution to be able to win it. The surgeons will seek ways to pass the costs through the reimbursement mechanism to the public, and the non-surgeons are not sufficiently threatened to cooperate. Ultimately, the public will have to recognize they are bearing almost all the costs of this conflict between professions, and direct public officials to do something about it. Whatever jurisdiction seems most appropriate begins to lose traction, here. Yes, the Legislative Branch is probably somewhat more appropriate, but from the beginning of our Republic, the legislature has been dominated by lawyers. Representation by physicians has in fact dropped considerably since the 18th Century, reflecting the vast increase in scientific progress, leaving them little free time for public service of the sort useful in a battle like this.

|
| John G. Roberts, Jr |
The person who comes to my mind is the Chief Justice. It is not commonly recognized that the Chief Justice, both of the United States and of individual states, has administrative control of the court system. Since most jurisdictions do not have monitoring and reporting systems useful for malpractice reform, these should be established. There is no great amount of judicial literature useful to a balanced analysis of this problem. There are no public forums for debating the matter which is not heavily sympathetic to one viewpoint or another, at least in the public view of it. And there are no fifty-one persons better positioned to appointing such review bodies, debating forums, and proposal-making -- than these fifty state Supreme Court Chief Justices, led by the Chief Justice of the United States. These Chief Justices already have the power to implement the necessary changes, but they lack public support for doing so. So the Chief Justice is the one person who can act, if he first orchestrates some mandate to do so.
It happens that the Chief Justice is already the head of the Judicial Conference, which includes the presiding officers of both state and federal courts. This might be an appropriate place to discuss Tort Reform, or for some reason, it might be better to appoint a special Task Force. One suggested approach might be to examine the usefulness of transferring hallmark cases to a special Federal Court of Appeal for Malpractice, or transferring particularly egregious awards to such a court, or constitute it as a special court of appeals for hallmark cases. That is, it is uncertain whether such a specially skilled court should be regarded as a way to untangle contentious issues, or whether it should be constituted as a punishment for outlandish judicial behavior. In one case, the policing power would be in the certiorari process, in the other, it would be by mandate from the Judicial Conference.
This is just a suggestion for adopting an approach which does not seem to have been used much. It was prompted by watching one particular State Chief Justice transform the malpractice environment of his state in a matter of a few months; I'm not sure how he did it, or whether I would approve of what he did. And after a year or two, things went back to the way they used to be. But the Chief Justices seem to have a role in this matter that needs to be explored.
ERISA Is Thrust Into the Battle

|
| ERISA |
In 1963 the Studebaker automobile company went bankrupt, leaving half its employees without anyone to pay the promised pension benefits. Congress soon resolved such things should never occur again and convened a Congressional task force to devise a law which would make employee benefits survive, even after the parent company went under. Negotiations took almost ten years and were said to craft a law that could not be amended, thus assuring employees their pensions would be independent of the fortunes of the company itself. Somewhere near the end of this long process, someone asked why it could not extend from pensions to health insurance as well. Almost as an afterthought, health insurance acquired some new features which had never really been considered in the past. ERISA (Employee Retirement Income Security Act) was enacted, signed by President Ford in 1974 and almost immediately began to change the whole discussion of health insurance. The suggestion I would make is that this legislation takes care of interstate health insurance, and seems to have created very little dissension. It might, therefore, contain some features which peacefully solve the same problem of reconciling a mobile and itinerant population with the Tenth Amendment.

|
| Interstate Commerce Commission Seal |
Because the Constitution provided for only a limited set of powers for the Federal Government, and the Tenth Amendment repeated the point for strong emphasis, every power not expressly given to the Federal, and not expressly forbidden to the States, was to be a power of the States. And that included health insurance. The Court-packing uproar of 1937 considerably strengthened the power of the Federal Government to extend its ability to regulate commerce. Indeed, advocates of this movement have been at pains to describe the Interstate Commerce Clause as merely "the Commerce Clause", as if to pretend it had never said anything else. However, the authors of ERISA (the Employee Retirement Insurance Security Act) expressly included pre-emption clauses which rather unnecessarily provide that Federal Law and Regulation should supersede state powers in that area.
There was a conflict here, in which ERISA apparently had to behave as though the Tenth Amendment did not exist. The conflict was never resolved by the Supreme Court, probably because it was so evident that business was delighted to have a thousand mandated benefits in state laws undermined by Federal pre-emptions. Concerted efforts by labor lobbyists had succeeded in putting everything they could imagine into health benefits packages, which were then exempted from income tax. Health insurance became "first dollar coverage", greatly increasing its scope. Because it included many low-cost items, its insurance administrative costs were unduly high; and because it included birth control, it was even a welcome respite for the Court system from the excited lobbyists on both sides of that inflammable issue.
Unfortunately, much of the behavior in the health insurance world is political rather than economic. Consequently, big businesses were mainly interested in is having one fifty-state insurance umbrella rather than in winning arguments in public. The use of federal regulation allowed them to have nation-wide insurance with uniform benefits, and it probably allowed them a wider set of insurance choices at lower prices. Moreover, it helped the Human Resources departments of the major corporations to have their way unhampered, and get rid of such nuisances as obstetrics for male employees. In the original negotiations, labor unions were bought off by allowing them to run their own "independent" health plans, but eventually, they went back to searching law books for loopholes. And the conflict between the "supremacy clause" and the Tenth Amendment was certainly a logical one to pursue because one mandated Federal regulation, and the other precluded it. Twenty-six states place taxes on provider institutions and most of them use the tax money to draw down federal matching money at anywhere from 1:1 to 1:4 levels, which is then returned to hospitals as "disproportionate share hospital" reimbursement. Other states use tax incentives to force third-party administrators to restructure benefits in a way that mirrors regulation.
By far the commonest set of dodges take advantage of judicial opinions that the states could regulate what was insurance, whereas the Federal regulation mostly applied to "self-insurance". The feeble distinction was whether lump sums were paid to an insurance company to distribute, or whether the parent employer distributed the money directly. By extension of this principle, reinsurance was taxed, payments to hospitals were federally regulated. The principle of risk-sharing was dragged into discussions which relegate state regulation of stop-loss arrangements, especially those with low attachment points, as indistinguishable from pure insurance; while self-insurance and experience rating are state regulated. What to do about "pure" insurance with a high deductible is less clear. (This may be one subtle reason why first-dollar coverage, in some ways the least desirable insurance form, is treated as a default, while Catastrophic coverage, which ought to be the basic protection, is relegated to a status bordering on outlandish. By treating huge costs as the responsibility of local charity, this arrangement tends to make them remain so.) That is, by inserting a fictitious intermediary, the regulation supposedly changes from federal to state. The model for this would seem to be one-bank holding companies. Consequently, trial lawyers have taken to suing the fiduciaries of trustees, leading to the comment that "You would have to be a lunatic to agree to be a fiduciary." The longer all of this goes on, the more tangled it will probably become, so the Supreme Court is probably under heavy pressure to pick a suitable case, and decide it.

|
| Affordable Care Act |
Shortly after the Affordable Care Act was passed, big business employers were given a one-year deferral of mandated coverage. The tangle with insurance exchanges for small employers (fewer than 50 employees) does somewhat justify getting that part straightened out, before taking on the much larger issue of employees in the large groups. But there is probably much more to it than that since large employers have the ability to hire assistance in the technicalities, and could probably quickly do many things small employers could not contemplate. Since it was elected to do the more difficult job first, this explanation is unconvincing. We are left uncertain: whether a big business has walked out, is bluffing its intention to walk out later, or has some other use for the extra delay. A secret Republican promise to offer more favorable terms, in exchange for help in the 2014 elections, would probably not be difficult to obtain. Meanwhile, uncertainty whether state mandates for low-cost medical items apply or not hangs over the surprisingly high deductibles being placed on insurance plans in the exchanges. For Catholic voters, it is critical whether they will be compelled to include birth control pills; for Health Savings Accounts, eliminating low-cost state-mandated benefits is important for high-deductibles to work. And for Obamacare, if state-mandated low-cost issues must be covered, it is hard to see how high deductible policies could work, how alternative co-payments can be avoided, and therefore how lowered costs can be imagined.

|
| Henry Kaiser |
Pre-empting state-mandated benefits is not the only issue that could be used for trade. Everybody has been curiously silent about the egregious unfairness of the Henry Kaiser tax exemption for employee benefits, with no deduction at all for the self-employed. The solution seems quite simple: preserve tax neutrality by lowering the tax exemption for employees by about a quarter, but extend the result to everyone. There are so many more employees than self-employed, that the exemption for self-employed could be paid for with quite a small downward adjustment of the exemption for employees. For this tax inequity to persist for seventy years, somebody is being pretty stubborn.
Note: Later in this book we discuss investment returns, and ERISA regulates huge dollar amounts of employee pensions, many of which are in trouble because they are underfunded. Most of the investment is subject to 1-2% fees of one sort or another, which would disappear if the investment switched to index fund investment without fees of more than 0.25%. Rather than let the City of Detroit, or the States of New Jersey and Rhode Island, go bankrupt because of unfunded pensions, it would seem worth-while for some politician to sweep out the investment advisors and purchase index funds. If it seems like a lot of trouble, just imagine what might happen if your political opponent in the next election, suggested it first.
Money Bags
This little morality tale was told to me by two unrelated sources, one of whom was a staff aide to Wilbur Cohen, the author of the Medicare law. And the other was a high official of Pennsylvania Blue Shield, the appointed administrative agent for Medicare in Pennsylvania. Its relevance to the more recent SNAFU with Insurance Exchanges introducing the world to Obamacare should be fairly obvious.
After Lyndon Johnson rammed the Medicare amendment to the Social Security Act through Congress in 1965, he wasn't shy about drawing attention to it. The press was present in great numbers, with staff officials who had a role in crafting the document, members of Congress, and anyone else who was standing around. The legislation was laid before him and signed with twenty different pens to be presented as mementos to the in-group. Each pen was only used to inscribe about half of one letter of his name, so it was a slow but joyful process. As intended, it got lots and lots of publicity.
 > >
|
| H. Ross Perot |
So, thousands of thankful old folks saw the ceremony on television, though they heard that the law was in effect immediately, and proceeded to dump their medical bills into a shoe box, sending them to Medicare to be paid. Unfortunately, Medicare didn't have an office, a staff, or even a telephone number. These things take time. As fast as they could, the Medicare staff constructed a system of carriers and intermediaries, carriers for part A, and intermediaries for part B. And almost without exception, appointed the local Blue Cross and Blue Shield organizations to be the carriers and intermediaries. Consequently, the organization of Medicare was patterned closely after the organization of the two administrative corporations. Meanwhile, the bills from old folks just kept pouring in through the postal service. It was about all the staff in Washington could do, just to direct the mail out to the local intermediaries and at least get it out of their hair.
Less than a year later, that's how the claims manage to Camp Hill, PA, a little suburban town near Harrisburg. In desperation, Blue Shield had rented a local vacant supermarket and piled the mailbags ten feet high. There were quite a few telephone calls of inquiry, and the old folks were politely told the matter was being looked into. It was beginning to look as though one supermarket wasn't big enough.
Computers were, of course, rented from IBM, who had a policy of renting, not selling, its valuable equipment. Keypunch operators, computer operators were hired, air conditioning was installed, and one team after another of computer programmers was hired -- and fired. Consultants were called, scratched their heads, sent big consultation bills, and turned sadly away. Sorry, but somehow it just doesn't work.
So that's how it happened that one Friday afternoon, a vice-president of Texas Blue Cross named H. Ross Perot came in, accompanied by a fellow with glasses so thick they looked like the bottom of Coca Cola bottles. So far as anyone can remember, the guy with coke-bottle glasses never said one word. The desperate, hopeless mess was explained to Perot, whose salary at that time was rumored to be twenty-five thousand dollars a year, about right for a Blue Cross executive. His background as a kindred Blue Cross person inspired confidence, and the conversation rambled on for an hour or so. Meanwhile, the guy with coke bottles went over to the Penn-Harris Hotel across the street and got to work. By the end of the weekend, he had come back a couple of times, but eventually, would you believe, it really, well it really worked. Contracts were quickly signed, the wheels began to turn, the mailbags in the supermarket began to march through the processing cycle. Blue Shield, the Medicare program, the finances of the nation's elderly, and Lyndon Johnson's reputation -- were all rescued.
As everyone now knows, the Medicare processing contracts made Ross Perot into a billionaire, living on Bermuda in the lap of luxury, eventually upsetting the re-election hopes of George Bush, senior by running for President himself on a third party ticket that had something or other to do with giant sucking sounds. A Congressional investigating committee looked into the outrageous profits Perot had extracted from his homeland's elderly, volleyed and thundered. Whether Perot actually thumbed his nose at them is doubtful, but he certainly was in a position to do so.
Meanwhile, whatever happened to that guy with the coke bottle glasses, no one seems to know.
Electronic Insurance Exchanges
Forty-some months after Obamacare passage, its initial computer program was a huge and public flop. Since Obamacare contains four hundred fifty other sections, the future seemed ominous for what follows. At its worst, it even seemed possible the whole nation might be without a way to pay its medical bills for an indefinite time. It was impossible to say how long it would take to fix things. Things looked dim, not just for Insurance Exchanges, but for any other hugely complicated proposal giving politics the highest priority over technology. It was muttered that the fault was the government procurement process, whatever those mysterious words mean.
Up until October 2013, it had been axiomatic that other requirements must be sacrificed to preserve the priorities of the Federal Government. Of a sudden, the possibility had to be faced that the computer age -- or worse still, the nerds and long-hairs -- might impose a revision in Big Government's notions of sovereignty. These electronic systems are expensive, in the multi-billion dollar range. It is simply not tolerable to keep throwing them out until you find one that works. So what's left to conjecture is the awful possibility that government must change. There may turn out to be multiple ways to address the situation, but at the moment there is only one. It's called privatization, and it's not something a liberal political party welcomes.
But let's not go on about that; it is what it is. To some of us in the policy world, the great pity was that the Electronic Health Insurance Exchange was one feature of the Affordable Care Act which seemed like a good idea. Its sudden collapse might well force the Administration to continue its dependence on the existing insurance industry, along with its antiquated approaches. It might endorse caution about changing anything which seems to be working, or making reforms which are even mildly difficult. For example, direct marketing.
Direct marketing implies sales of insurance directly from the insurance company to the customer, without a broker or other intermediary. The insurance industry has been burdened since the 19th Century with heavy marketing costs and middle-men, reflecting the difficulty of convincing consumers of the safety of paying premiums without immediate contact with what it actually buys. Putting marketing in the hands of employers may once have been a necessary feature, but "job lock" and reduced international competitiveness for employer sponsors, have now grown to be fairly serious problems. The resulting incentive is to prefer to hire well people who are cheaper employees, thus hampering national efforts to hire the handicapped and extend the age of retirement. Employer sponsorship still retains one advantage: control of a large block of customers positions the employer to muscle down healthcare prices in the community through board seats at the local hospitals, health insurers, or newsmedia. But employer involvement creates an unexpected feature, that of union domination of the employer's seat at the table. These are all delicate balances, and a switch to direct marketing must be slow and incremental. Doing it all by the first of October may have advantages for politicians with their eye on the first week in November, but political deadlines can, and sometimes have, brought the system to its knees. It is definitely not liberating to have a goal of mandatory universal coverage, right now, immediately. Nevertheless, direct marketing does force insurance products to be more uniform and price-sensitive. And voluntary, not mandated.
Electronic insurance exchanges also address the Constitutional awkwardness. Both healthcare and insurance directly respond to the Tenth Amendment, that everything not Constitutionally mandated to be federal, must be state-regulated. And it's a good thing that is so, from the point of view of the small and sparsely settled states, who do not have enough actuarial power to support more than one monopolistic health insurer. By original intent, no Constitutional amendment could pass, over small-state opposition. But cheer up, the Tenth Amendment also applies to every major corporation in the country, and nevertheless, the little state of Delaware has no trouble harboring hundreds of corporations. These corporations operate as "aliens" in their home states, and for the most part, exist in Delaware as a brass plaque on the wall of a lawyers' office tower. Their corporate stock is listed in New York, on the stock exchange. Their products are sent to all corners of the nation, by Amazon, located in Seattle. These dispersed arrangements sound tortured and complex, but nevertheless, they are driving down transactional costs to the despair of their competitors. If we depend on competition to discipline prices, we must make competition possible.
Finally, computers make it easy to break health insurance into a hundred pieces, and allow the individual subscriber to tailor the pieces as an itemized package, or ultimately, a personalized list. If someone forces me to have obstetrical insurance, I feel sure some distant insurer would sell it to me for a dollar a year, knowing that the claims from an elderly widower would still allow them to make a profit on my nonexistent obstetrical care. Or if I have had my appendix removed, the risk of paying for a second time is pretty small. It works the other way around, as well. If some hospital wishes to charge "Medicare plus seventy percent", let them do so. I'm interested in buying health insurance that pays "Medicare plus five percent", and whether the hospital agrees in advance to accept it as payment in full. To capsulize this point: buying health insurance interstate and at a great distance, forces the products to be uniform, clearly defined, and cheap. And while any political entity may subsidize whom they please, the subsidies will be forced into the open.
So those are the reasons the electronic insurance exchanges seemed to have the kernel of a good idea, ruined by being in too big a hurry to do something which takes time getting used to. Like making it mandatory, universal, non-voluntary, and inflexible. But worst of all, demanding that it work by the first of January, next year. We're not selling snake oil, here. We're planting an oak tree.
Furthermore, name the CEO of almost any successful computerized business. You probably do know his name, whether it is Andy Grove, or Bill Gates, or Steve Jobs, or Tom Watson. But the name of the person in charge of electronic Obamacare is unknown to almost anybody. That he is a billionaire seems unlikely, even in a field full of billionaires; just about all of them are in the top 1%. Now that the Electronic Insurance Exchanges are such a notorious flop, it is going to be harder to find an outstanding person willing to accept the job--at anything approaching the laughable top salary level considered appropriate in a political environment. George Washington refused to take a salary, but that was then. The current situation is much like the one described by Mark Twain, of the man who wouldn't mind being hanged for his mistakes, except for the honor of the thing.
Privatization puts people out of work, and has other political liabilities, particularly for a President who has made such a point of denouncing the top 1%. But privatization is one quick way to find a genius to run a company, promising to make him and his close associates into billionaires as a reward for success, threatening disgrace if he fails. Awarding the whole program to a corporation after demonstrated success, not before then, concentrates the rewards on the politician who makes the correct choice. If his company is too small to handle it all, he can merge with others if he pleases, and fight with them about unpleasant succession issues. Privatization is not guaranteed to be successful, but privatization has been shown to work, more often than not.
Establishing an eventual goal of direct marketing will also force the insurance product to conform to what is useful for direct marketing, but such pressures do not seem to be injurious, as will be discussed in subsequent chapters. But one thing is pretty sure: mandatory universal coverage would be the last step in implementation, not the first.
Redesigning Electronic Insurance Exchanges
Having sniggered at Obamacare's Electronic Insurance Exchange mess like everyone else, it has been admitted here there were some good ideas buried in it. Indeed, a politician of the highest rank ought to be able to fish out these good ideas, call them something else, and reconstitute them. The good ideas would seem to be:
Interstate Health Insurance The U.S. Constitution's Tenth Amendment makes it clear the Federal Government should confine itself to a short list of necessary activities; E everything else is to be regulated by the various state governments. At the other extreme, actuaries have determined that a health insurance company cannot possibly survive an occasional catastrophic illness unless it has two thousand subscribers. Five thousand would be better. And the size of the groups is conditioned on being able to limit the insurance coverage to one year, with other limitations like pre-existing illness and non-renewable clauses, which protect the small new company from attracting too many people who are sick. These are limitations since if you admit ten or twenty subscribers with very expensive conditions, you must then admit several hundred perfectly well people to cover the costs of the entire group. Looking at it in reverse, most insurance executives would say they are uncomfortable with any group smaller than ten or twenty thousand subscribers, particularly if politics are going to force the acceptance of expensive sick people. Even then, they are thinking in terms of annual, or term, insurance. To ensure a lifetime of health costs as a unit, as we are about to contemplate here, requires a subscriber group which is possibly larger than the present population of many small states. Somewhere along the line, the required customer base will block implementation of the concept of lifetime health insurance for individuals, by provoking the excluded states to demand a level playing field. On the other hand, if interstate sales could somehow be permitted, the small states would become its greatest supporters. Summing it all up, interstate sales of health insurance are the key to exploiting the potential for lifetime health insurance, whose attractions will be discussed later.
Add to this the biggest hazard of them all, the tendency of large groups to demand discounts. The Blue Cross plans started this in the 1930s, and competitive health insurers were loud and bitter about the "Blue Cross Discount", which they quickly matched by seeking to negotiate special discounts for large employer groups, themselves. Eventually, we got to the present uproar about uninsured people, because the whole process had concentrated expensive sickness into about 5% of the American public. Governments and business enterprises complained about burying the costs of uninsured people into the premiums of large groups; ultimately, they showed their real feelings by demanding that individual (that is, non-group) policies be eliminated entirely from the insurance pool. The very largest groups sought to eliminate themselves from pooling with small businesses, by retreating to ERISA plans or other routes to group self-insurance. This is a mess largely hidden from the public, waiting for the Electronic Exchange uproar to die down. The point here is merely to emphasize the almost irresistible forces pulling in the opposite direction. To summarize: the requirement for single-state regulation, added to the need for comparatively large groups to be viable, has eventually led to fifty monopolies plus a great deal of dissatisfaction. How in the world can we transform this environment into twenty or thirty, or even fifty, interstate insurance companies? The uneven geographical distribution of the population might allow an expansion of the marketplace to more than a hundred viable companies. Increasing the available market for small insurance companies, easing the entry problems for new companies and allowing the marketplace, not the Tenth Amendment, to determine the best size for viability, might all be regarded by everyone as a good thing -- because small companies reduce the cost of failure, hence encourage innovation, mergers and all those other good things into a somewhat fossilized industry.
Direct Marketing Replaces the Employer Middlemen. Dismissing the possibility of repealing the Tenth Amendment, the stock markets provide the easiest model. The central element is to confine the exchange to trading a single essential component, encouraging that market to reduce its transactional costs to commodity levels, serving everyone at costs so low that competitive prices are not much of a worry. Health insurance companies have grown comfortable with playing footsie with state legislatures and Insurance Commissioners, so there is ample room to reduce transaction costs to the point where the total price of health insurance is not seriously affected by them. At that point the real competition is between states, attempting to devise good laws and good regulation. The stock exchange model suggests that any insurance company would be happy to pick its own home state (currently Delaware is the corporation favorite). Meanwhile, direct consumer marketing of the exchange's product can be national in scope, satisfying the Constitution although probably not the McCarran Ferguson Act. If you please, we substitute the model of Amazon for interstate marketing of many products directly to the subscriber. And by the way, invite Amazon and similar to bid on running the privatized system.
Niche Marketing Blue Cross owes its initial success to supplanting "Polio Insurance" and "Cancer Insurance" with broader-base "Hospital insurance", in the 1920s. Its resistance to niche insurance in the Medicare Advantage plans may, therefore, be merely a knee-jerk reaction, or an effort to be consistent over the decades. Or The Blues may have more substantive issues with niche marketing, which amounts to choosing the particular disease you fear most, rather than the annual cost of the hospitals you choose. As soon as you lose confidence in the fairness of hospital prices, you become willing to re-examine whether something else might be more difficult to manipulate. In any event, the most major flaw in Obamacare is to try to stretch what is satisfactory for 95% of the population, into covering the last 5%. In this, it seems to have encountered serious difficulties. Starting with roughly 40 million uninsured as a goal, after major upheavals it still has been estimated by the CBO to leave 30 million uninsureds, and cost a trillion dollars over ten years. It is possible to account for most of thirty million as belonging to one of three groups: 8 million prison inmates, 8 million mentally impaired, and 11 to 20 million (estimates vary) illegal immigrants. These people have considerable group similarity but differ so much from the rest of the population that it seems more appropriate to design three special programs, rather than tinker with existing populations which lack their special needs, probably making more people dissatisfied in the process. On a national basis, there are enough in each group to satisfy actuarial requirements for insurability. If one or more of these niche products is a failure, however, it can be modified or even dropped without disrupting the rest of a functioning system. Niche products are niche products. For example, mentally defective people often have epilepsy, which leads to a legitimate need for football helmets; who else could claim helmets as a medical expense?. Illegal aliens need translators, prison inmates need detoxification centers. Any social worker could quickly list the "special needs" of these three patient categories. If this is what we need, let's provide it rather than disrupt the rest of the population.
Special Discounts. In an environment which is accustomed to cross-subsidy treated like a virtue, scarcely any recognition is made for people who cannot possibly have a particular risk. Males and post-menopausal women are occasionally mentioned as unable to have children, but here the problem is complicated by the issue of child support. But if you have had your appendix, and/or gall bladder removed, it can't be removed a second time. Doesn't it seem fair to reduce the premium for those who cannot have the risk? How about someone who has had two cataracts removed? If we have the concept of reducing auto insurance premiums for a certain number of years of "safe driving", why can't we use our computer capability to reduce the costs for those who can be shown to have less risk? At least, we ought to be able to put this data to some use, rather than treating it as a social blunder even to mention such a thing. Ultimately, we can consider lifetime health insurance with a level premium. That is, you subsidize yourself at one age by taxing yourself at another age.
Who would be hurt by all these changes? Quite obviously, the subscriber would benefit from choosing his own policy rather than letting the local insurance monopoly and the Human Resources departments choose the insurance on behalf of all employees collectively. The employers would benefit from eliminating middle-man costs. The benefits for Union Health plans are not so clear-cut, so they might resist until they actually came into competition with minimal exchange prices. And the government would benefit from opening the exchange operation to competitive bidding, thereby privatizing the system. By doing so, they might even make a profit, rather than sustain continuing costs, including political costs, trying to do it themselves.
Creative Destruction for Health Insurance Companies

|
| New York Stock Exchange |
Of the stocks now listed as members of the Dow Jones Industrial Average -- the largest and most successful corporations on the New York Stock Exchange-- only one of them made the list in 1900. That was General Electric, and although GE is still a successful business, it' s definitely not the wizard it used to be. Every investor, indeed anyone with a pension fund, should recognize that corporations have a natural life expectancy of about seventy-five years. No matter how successful a company is, when it reaches seventy years of age, three scores and ten, it is time for portfolio rebalances to consider replacing it with something younger. This curious life cycle of institutions usually regarded as immortal is unexplained, but it may match the life cycle of the man who initially formed the company or the decline of the founding family; or perhaps the original business plan becomes obsolete, unable to keep up with changing times. One alternative principle needs to be explored further, however: it always costs more to repair and reconstruct, than to start all over from scratch. A nation which prospered within a constantly expanding frontier may someday need to revisit this basic idea underlying "creative destruction". Automobile insurance companies, for example, often startle their claimants with the news that it is cheaper to "total" a dented car than to repair it. Building a new car involves engineering to compete for low-priced quality, but repairing an almost-new car after an accident will always involve tailoring a hand-made restoration. In the meantime, the whole healthcare insurance industry of America needs to be more reconciled to the possibility that it would just be cheaper to start all over with basic premises. And state regulation might be one of them.
Along these lines, there is an old joke in Philadelphia about the father who advised his teen-aged daughter, "If necessary, you may sell your body. But never, never sell your Pennsylvania Railroad stock."

|
| Joseph Schumpeter |
Consequently, it is not a sign of disloyalty or thirsting for vengeance to observe that what we now call health insurance companies were created in the 1920s, and therefore unsurprising if we saw them decline or go out of business relatively soon. Joseph Schumpeter seemed to proceed from the same observation, regarding it as one of the democracies' strengths that major corporations regularly undergo "creative destruction". Whether a good thing or a bad thing, it seemingly is a fact of life. Therefore, nostalgia for the good old names an investor recognizes from his childhood doesn't necessarily make the best investment strategy. But face it. Buying "cats and dogs" isn't so smart, either, so it's usually better for most folks to stick with companies that have some seasoning. The conflict between brand names and entropy is thus a continuous process of adding and subtracting. And because it is easier to have something automatic doing unpleasant things, this one probably needs an external threat to move the needle.
Streamline Health Insurance?
Let's review the logic. Mandatory health insurance was considered to be necessary because we wanted Universal health insurance. And we wanted universal insurance in order to extend health insurance to those who had pre-existing conditions. In a sense, we don't have a mandatory insurance problem, we have a pre-existing condition problem. Is there no other way to solve this?
Perhaps, and perhaps not; but let's take up this critical point at the end of the discussion. Right now, it is pretty clear that 10% is a pretty big price for someone else to pay your bills. Most of us would not pay so much to have someone buy our groceries, pay our utility bills, or put quarters into a parking meter for us. We very definitely would not pay such a fee to someone who proposed to do it with a system of three insurance policies (one for 80%, one for 20% copayment, and the third one for Major Medical policies for gaps in our policy coverage). Nor would we compensate a payment agent to pay for coverage which is riddled with cash demands for escalating deductibles and copayments, every time we go to the drugstore, to the accident room, to the doctor's office. Something surely is wrong when we surrender the convenience of third-party payment, pay heavily for this service anyway, and they are hounded and confused by a myriad of partial payment demands, or bewildered by undecipherable itemized bills with an astonishing total at the bottom -- but nevertheless marked "patient responsibility, zero". Something is very definitely wrong when hardly anyone can explain the payment system to us, and no one is willing to quote a price in advance of service. So, let's start by considering what would happen if we eliminated co-payments entirely, and confined deductibles to out-patient services.
In the past, it might have been theorized that prices would go up because patient participation puts a brake on prices. But now we would have to contend with the question, "How would you be able to tell the difference?" The patient in a hospital bed is incapable of haggling about prices, while the hospital is mostly reimbursed in an approximated lump sum, called the DRG (diagnosis-related group). Even those insurances which are reimbursed by items are subject to secret discount systems, which vary from 40% discounts for state Medicaid to overpayments of 30% of costs for private insurance, and up to 400% for payments by list price. This system led one very famous Philadelphia surgeon to growl, "The main purpose of having health insurance is to keep the hospital from fleecing you." The bad public relations of asking the public to endorse this summary would make the problems of changing the system seem minor. For public relations alone, the system must be made more transparent. Most hospital administrators would make the irrelevant response that, after it all shakes out, hospital inpatient care only generates about a 2% profit margin.
That may be true but fails to emphasize that emergency room services generate a 10-15% profit margin, and hospital out-patient and satellite clinics approach 30%. If you drive past a nearby hospital, you are very likely to see a construction crane in operation. But just take a guess in advance at what type of building is being built.
Since hospitals are obviously responding to prevailing profit margins, they would be wise to agree on negotiations with insurers based on audited profit margins, assigning the margin to individual departments to divide up after internal negotiation. For inpatients, a refined object of negotiation with insurers should be an agreement on the variation of reimbursement to be tolerated between insurers for substantially similar inpatients, essentially some variation of Diagnosis Related Groups. A later chapter discusses improvements needed for DRG determination. The central point is: no attempt should be made to bargain prices with a patient who is sick enough to require inpatient hospitalization.
For emergency room services , it is possible to imagine a sort of DRG, and if the patient subsequently requires hospitalization, that should be the ideal approach. However, most emergency patients are not admitted, and there are usually nearby competitors for them. Therefore, some sort of hybrid should be constructed, partly an Emergency DRG, but also modulated by comparison with neighborhood facilities.
For outpatients, competition should rule, and any insurance accommodation should reflect that fact. Ideally, small outpatient services should be cash transactions, but the trend lately is for increasingly expensive procedures to be performed in the outpatient area. The most suitable outpatient payment would be the option of using a Health Savings Account. Optional, because it is desirable to encourage those who are able to protect their HSAs for other uses, to be described in later chapters.
The ambulatory patient is fully capable of loud and insistent bargaining over prices, ultimately threatening to go elsewhere or just to refuse the pay the bill. In the last extremity of disagreement, the provider will be very glad to accept an HSA, so it serves as sort of a distorted re-insurance, and it is useful to have a central reporting mechanism to determine how the market is faring. Since everyone is now entitled to have an HSA, everyone should sign up for one. The uproar over the Electronic Exchanges has demonstrated that almost everyone is coming to the conclusion that high deductibles are desirable. The reasoning is not so self-apparent, but it is nevertheless also true, co/pay is something to be discouraged.
Electronic Medical Record

|
| TRS-80 Model I |
When the first home computers became available in 1980, I bought a TRS-80 from Radio Shack and tried to automate the paperwork in my office. It was fun, and the idea was exciting, but after a few years I gave it up. I was willing to accept a partial electronic record, which was limited to data input that was already automatic, in order to get something useful, without making extra work for myself. Over thirty years later, an embroidered version of it was working satisfactorily in my office, but it was far from complete, and I had not been able to persuade a single colleague of mine to use it for more than a trial. To finish the story, when I retired I was advised I had to retain my records for seven years. During those seven years, I had exactly two requests for any of the thousands of records.
The reader is entitled to suppose my particular electronic record was a poor attempt, but now that it's a requirement, I hear nothing but the same old complaints which made me conclude the electronic record was not ready for prime time, as they say. First of all, it takes too much of the doctor's time for data entry. In effect, the bulk of the record was typed in by me. An ophthalmologist friend, concerned with a much more limited data set, would use the computer (he had a MacIntosh) to jot down notes, and then turn it over to his secretary to expand into something readable and useful. He had three secretaries, by the way, so he was the fourth secretary in the system. Some other ophthalmologists expressed interest in his approach, but so far as I know, no one else adopted it. More recently, my physician daughter used the Kaiser-Permanente system which is considerably more sophisticated, and found the data entry imposed on her was burdensome. In fact, she devised a sort of measure of the extra work. She was staying at the office an extra two hours a day, falling further and further behind. So, she requested a 10% reduction in her patient load (and salary), but still fell behind. So, she dropped her workload to 60%, and found she then enjoyed the experience, although not the 40% reduction in income. From this I derive the estimate that the electronic medical record reduces physician efficiency by 40%. She says most of her colleagues just fake it to maintain their income. It's hard to translate a 40% impairment of physician efficiency into a reduction in quality, but one can make one's surmises.
I'm pretty proud that my daughter was unwilling to compromise her principles for money, but that really isn't the end of it. Both my system and the one she uses would record the patient's laboratory work instantly in our offices, which was very gratifying, except all of the eleven hospitals where I was on the staff refused or were unable to send the hospital laboratory work to my office for the inpatients. That was summarized on the typed discharge summary they mailed me, often several weeks after discharge, and added to the office record, that was also true of x-ray, pathology and electrocardiograph reports, so the office record was fairly complete, but hardly automated. But even if automated in some way, it was pretty unreadable. Quite a few records ran to a couple hundred pages, which is not something a doctor is likely to read before each visit. It provided me with a useful record, but I certainly was not going to spend the time to organize it. What the computer needed to to was to organize a system of periodic summarization, but to be useful it had to condense the summary to 10% at most of the raw data. When some company produces a program that will take the input load off the doctor's back, and also automatically produce concise and accurate summaries, well, let me know. My present position is that EMR is not ready for everyday use, it's going to cost an enormous bundle of money to force that conclusion to be changed, although here and there, for some specialties, it produces a few benefits. Meanwhile, let me tell you a story about how EMR remains a tantalizing dream.
We have half a dozen hospitals which deliver babies in central Philadelphia, all within twenty blocks of each other. We also have an ambulance service which operates on the strict rule of taking every patient to the nearest hospital. Pregnant ladies still go shopping or to the theater when they are at term; it's sort of a form of bravado. And so, it is inevitable that quite a few of them get caught in labor, call an ambulance which obediently takes them to the nearest hospital. But their doctor is waiting at another hospital, and has their records, which the receiving hospital does not. I can tell you with the best will in the world, it takes at least an hour, often more, for a hospital to get a call, find the record, and fax a hundred pages to the hospital that needs it. By the time all this confusion gets sorted out, the baby has been born without any use of records. No doubt all the confusion could be straightened out by an efficiency expert, either by periodic fire drills at the hospitals, or raising Cain with the ambulance people, depending on who is most likely to prove helpful. Meanwhile, we dream of an electronic record to solve a problem that is pretty low on the priority list of all concerned. It's a good idea; it's just not ready.
It's worth a little time to ask why the hospital computer departments have proven to be so resistant to merging with physician office systems. The answer offered by some observers is that hospital IT departments report to the accounting department, who don't want to negotiate with a new set of bosses. There's something to that, or rather there was something to that, thirty years ago. Furthermore, the Nursing Profession has long maintained a resistance to being left alone with sick patients, taking orders from doctors who are miles away in their offices. Therefore, this attitude surfaces in an adamant resistance to verbal orders, demanding an order be signed by a doctor on the spot. No doubt all these anecdotes have variable application in different institutions, but they give a hint that resistance to the electronic record is not entirely based on technology, but it is no less real.
Computerizing Medical Care
Note: This article was written in 1999, long before Computerized Medical Insurance Exchanges were such a disaster:
|
| First Computer |
My first encounter with a computer was in 1958, and I have loved them ever since. As president of what called itself the Delaware Valley Hospital Computing Society, I remember giving a dinner speech concluding as follows: "If you want to be happy for a day, get drunk. If you want to be happy for a week, get married. But if you want to be happy for a lifetime, get a computer!" After fifty years, my affection continues. But to be candid, billions of dollars about to be spent on computers in medical care will mostly be wasted. Even worse, like malpractice suits computers will induce behavioral changes in the system costing far more than the directly visible costs.
That's unpopular news at present since the National Business Coalition for Health has launched a major lobbying campaign to persuade Congress to spend an initial billion dollars inducing physicians to maintain an electronic medical record. Various health insurance companies already provide financial incentives to doctors to file electronic claims forms, eventually threatening to reject any claim submitted on paper. The American College of Physicians has established a rather large department to develop programs for physicians to use in their practices; twenty years ago the University of Indiana started much the same thing. The College of Physicians of Philadelphia has spent close to a million dollars on such a project. It is reported that Microsoft Corp. has a massive project underway to supply electronic medical records. It sounds fairly easy to obtain large research grants from the government to devise something, anything, useful in this area. In my own case, training funds really weren't necessary, since I eagerly got into the field when everybody was a beginner. I was just as good a beginner as any other beginner. But let me repeat: the electronic medical record has been in the past and will be for decades, an expensive digression. In health care, creating more administrative work isn't the solution, it is the problem.
For fifty years the problem with an electronic medical record was that it took too much of the doctor's time to complete his part of the input, and then cost him too much to pay employees to do the rest. Presumably, automatic voice recognition and dictation will soon make it possible to record doctor's notes without handwriting or typing. Since, however, the elimination of current paper forms and check-off boxes will create a major problem in organizing the dictation verbiage, it could add five or ten additional years before programmers manage to rearrange dictation material and effectively integrate it into organized form, complete with laboratory results, dictated x-ray and EKG reports, even small images of the original material. Temperature, blood pressure, weight, photographs and the like can all be readily integrated into the stored electronic record, but to do so usefully is an expensive programming project. Doctors are quite right to be anxious they will lose control of the usefulness of their records in order to ease the task of programmers, speed up the sluggish pace of development, and reduce what will surely be an unexpected cost overrun. Storage and retrieval of such records is known to be an achievable but expensive task, which however also risks sacrificing the speed and ease requirements of the medical task it is supposed to serve -- in the name of cost-effectiveness.
Computers are no longer an unfamiliar tool; physicians have altogether too much experience with "vaporware", unrealized promises of convenience, and the damaging effect on the medical quality of the philosophy of Quick and Dirty. To respond to their resistance to design blunders with an accusation of undue conservatism is to provoke an icy stare and gritted teeth. Inevitably, the effective use of automation will require a redesign of workflow with major disintermediation of "gopher" staff; after all, that is how cost savings are to be achieved. That will provoke outcry that physician time is the most expensive component in the process, but unfortunately, physicians will discover Information Specialists with a business background will brush that argument aside. The most overpaid people on the face of the earth are investment bankers, but information consultants have persuaded business executives that inefficiency of the investment process is more expensive than even an investment banker's time. Having been through this themselves, insurance executives are unlikely to pay the slightest attention to physicians dancing to a familiar old tune.
For all that, data input is not the real problem; it's just the first problem. It's in a class with data storage and retrieval, which is expensive and cumbersome when you add a need for instant access and total privacy. But costs will come down steadily, and eventually, we can expect automated fingerprints or other biological identification, and cheap instant retrieval. Doctors will be able to make rounds in the hospital with a computer in their pocket, record telephone calls in their entirety, dial automatically and whatnot. There are problems with wireless transmission inside buildings with steel girders, and legal requirements for signatures on narcotic orders, but if we are determined, these problems can be overcome as easily as they were with electronic check writing and stock brokerage. Cost may top twenty billion dollars in twenty years, but it all can be done if we insist.
But then you encounter the real problem. Information will accumulate in these records in staggering amounts. Even if you resolutely resist demands to have the nurses record every groan, and the orderlies file every laundry slip, the legitimately important medical information will be exposed as the massive heap of transients that they really are. Plaintiff lawyers will insist no scrap of data may be deleted, hospital administrators will insist on compliance, when in fact most of a doctor's concentrated effort is devoted to brushing aside momentarily distracting data in order to see what's going on and react to it instantly. When a quick look doesn't solve the problem, the doctor goes back for additional data. If you disrupt these skills and traditions of coping with information overload, evolved over centuries, you will at best impose frustrating delays on a complex system under pressure, and ultimately inspire elaborate systems of short-cuts. The Armed Forces are famous for paperwork, but even they know better than to ask a pilot for his Social Security number as he starts a bombing run. The hospital nursing profession has already just about collapsed under paperwork pressure. If you see five nurses in a hospital, three of them will be sitting down writing something. The terrible truth is that no one reads it, no one checks it, and ultimately it sits in the record room waiting for a plaintiff lawyer with unlimited time to sieve out some misrecorded misconception or uninformed conclusion. My faith in the computer is such that I feel sure that methods can be devised to produce periodic summaries, automatic alarm signals, and mostly effective prioritization of data elements. Unfortunately, medical care is changing at such a rapid rate that ad hoc automation of physician thought processes cannot keep up with the current pace of change in medical progress. You would think some things would be unthinkable, but since I can remember the organized campaign to suppress the CAT scan as an unnecessary expense, I confidently predict that programmer inability to keep up with some advance in medical care will at times lead to organized outcry that we should slow down the pace of improving medical care, so that computer clerks can keep up with it. But that is only a small part of the issue, which at its center is that physician time will be dissipated and his attention distracted by presenting him with unwieldy amounts of neatly printed, spell-checked, encrypted and de-encrypted, biometrically secure, hierarchically prioritized -- avalanches of data which are irrelevant to the issues of the moment. The goal is not, after all, an electronic record. The local goal is to decrease the cost of medical care by increasing the productivity of the physician, and the overarching goal is high-quality patient care at a reasonable price. Behind all that, since the impetus comes from NBCOH -- the ones paying the insurance premiums -- suggests that the local goal is not so much the improvement of care as oversight reassurance that cares provided has been as good and as cheap as possible. The goal is legitimate, but this cybernation approach looks to be self-defeating by being overly specific.
If the reader has the patience for it, let me now cite a historical example of the third-party tail wagging the medical dog. In this case, third-party health insurance similarly overextended its reach by imposing internal health system changes, trying to facilitate the role of monitoring it externally. Specifically, the system of diagnostic code numbers was changed from one devised by the medical profession for its purposes, into a different coding system devised outside medial profession sponsorship, which seemed to suit the needs of payment agencies better even though it suited medical purposes less. After twenty-five years, it is now clear that third-party payers have shot themselves in the foot on this matter, and everyone is worse off. The topic, please pardon the obscurity, is the diagnostic coding system.
To go back to beginnings, the American Medical Association perceived a need for a diagnostic coding system in the 1920s. Organizing or even merely indexing vast amounts of information about a disease required more specificity than freestyle verbal nomenclature could provide. Quite a distinguished panel of specialists and consultants then produced the Standard Nomenclature of Diseases (SNODO) which in time became the Standard Nomenclature of Diseases and Operations. In order to reduce ambiguity, this system developed a branching-tree code design for anatomy, linked to a branching-tree for causes of disease, ultimately linkable to a branching tree of procedures. These three sets of three-digit codes linked the components together with hyphens (000-000-000). The first digit of each was the most general, as in Digestive, Musculo-skeletal, etc. and subsequent digits were progressively more specific and detailed, as in "Digestive, large intestine, sigmoid colon". The causes of disease would resemble "Infections, bacterial, streptococcal". An example of Procedures would be "Incision, incision, and drainage, drainage and insertion of the drain". In nine digits, it was thus possible to represent " incision, drainage, and insertion of a drain into a streptococcal infection of the sigmoid colon". After a while, the codes grew from three to five and six digits, again repeated three times, so an immensely detailed, unambiguous description might be coded in fifteen digits by a physician who knew the rules but didn't own a codebook. This code was ultimately taken over by the Academy of Pathology, expanded and is called SNAP. The pathologists absolutely refused to give it up.
The rest of the profession gradually yielded to the pressure of hospital administration, who was pressured by the Association of Medical Record Librarians, responding to the views of outside statistical interests, particularly insurance. A simpler, shorter coding system was needed, they felt, concentrating on the thousand most common diseases. The International Classification of Diseases was produced, reducing the millions of SNODO diagnoses to 999 by heavy use of several varieties of "Miscellaneous" or "Not Otherwise Classifiable (NOC)". Since the goal was to count the incidence of common diseases, the coding system was stripped of any logical tree-branching and became a short list of what was most common, starting with 1 and going to 999. In time, of course, the common-ness of conditions changed, and various complaints from various directions forced the ICD to go to 4 digits, then five. Unanticipated conditions or complications eventually required the patchwork of some alpha "modifiers", and the original short hodge-podge became a long and bewildering hodge-podge. Coding accuracy declined markedly, but ho-hum. The health insurance companies paid the bill, no matter what the code said. At another place, we will discuss the entertaining way that Ross Perot became a billionaire out of the computer chaos of Blue Cross and Medicare at this time, but right now the central theme to follow is DRG, Diagnosis Related Groups. Try to follow, please.
By 1980, Medicare was fifteen years old. It was clear that certain things just had to be changed because the excuse that the system was new and untried was beginning to wear thin. The early designers of the system based their payments on auditing a hospital's yearly costs, auditing the proportion of patients who were Medicare beneficiaries, and paying a proportionate share. That was easy and reasonably accurate, but it had a rather significant flaw that it took no account of whether the patients needed to be in the hospital in the first place. Or whether they needed to stay so long. The response they adopted (in the Budget Reconciliation Act of 1983) is a measure of just how desperate they must have felt. Knowing full well how inaccurate the ICD coding system was in practice, it was all there was. Consultants, particularly at Yale, ran computer simulations of various subsets of ICD codes to find a formula that would produce approximately the same hospital payments as the system of cost reimbursement. If memory serves, the original formula was to divide the thousand ICD codes into 27 diagnosis-related groups (DRG). Eventually, the process was tweaked to seventy or eighty groups. Walter McNerny, then Past President of the American Hospital Association told Congress hospitals could live with this system, and promptly we had a system for paying out hundreds of millions of dollars. It was touted as a highly sophisticated advance in the arcane science of hospital reimbursement, so it must have included a lot of deliberate overpayment. I can remember trying to remonstrate with McNerny, who felt he didn't have time for the discussion. Physicians had very little to do with the DRG portion of the 1983 Medicare Amendments because the AMA had long insisted that physicians and hospitals go their separate ways on reimbursement. Russell Roth, who was president of the AMA at the time, recounted many times the episode in the Oval Office, when it was announced to Lyndon Johnson that Dwight D. Eisenhower"was in the next room waiting for him. LBJ excused himself to leave, and on the way out said to Wilbur Cohen, "Give him anything he wants." Things were destined to change, but at least for a very long time, physician and hospital reimbursements were strictly independent.
Smothered to Death in Greenbacks
Here's my macroeconomic nightmare, brought on by thinking too much about paying for health care costs, and supposing, just supposing, we were successful in doing it. The equivalent nightmare would be to imagine that some multi-billionaire walked into the offices of Vanguard or Fidelity, and said he would like to speak to the manager. After he had a cup of coffee, he would explain that he wanted to make a deposit of $5 trillion dollars in a total-market index fund. After an initial reaction resembling a Grade B comedy movie, the manager would begin to see the idea was pretty disruptive.
In the first place, $5 trillion is more than twice the size of the largest index fund currently in existence. We're getting there, but at the moment no one can be entirely certain what it would do. It might take months or even years to feed that much money into the markets without creating violence. That one buyer alone would dominate the stock markets of the world, bankrupting some, enriching others. In the Grade B movie I envision, dozens of beautiful starlets would be sent around for the sole purpose of learning what our buyer was buying next week. And what would he care, he would tell them. If he decided to make a big sale, markets would tumble, maybe crash.
Now, assuming this money was honest and not "dirty" as they say, the consequence of steady buying in huge amounts would be to flood the markets with liquidity. There might well be spurts of both directions, but in general, the addition of this much money concentrated in the stock market would send the price of stocks up, in response to supply and demand. If the price of a stock is generally raised without underlying business transactions to justify it, earnings per share would go down. In the long run, that could send the value of stocks down, resulting in inflation, because it would be possible to sell more stock without raising prices. In any event, reducing the scarcity of stocks would lessen the value of capital, compared with the value of labor. Reducing the value of capital would itself cause disorders in the economy before the markets regained equilibrium. Prices of labor-intensive goods would rise, prices of things which could be automated by using capital would fall. It would create new winners and losers; new elites.
For these reasons, students of economics generally hate macroeconomics. It's important, but it's hard to make final conclusions. In our Grade B movie, the bald-headed little manager ends the scene by jumping out the window.
Average Lifetime Medicare Balance Sheet
Lifetime Medicare revenues are about $55,000 in premiums from Medicare recipients, about $87,000 from payroll taxes paid by working people, and about $140,000 in general revenue, mostly from income taxes. These are soft numbers, approaching one quarter from the Medicare recipients themselves, one quarter from working people, and one half from income taxpayers. The best we can calculate is our proposal would generate about three-quarters of that. It's not enough, but what do you want for nothing?
The following average revenues of Medicare come from the CMS website, and must exactly balance Medicare expenditures:
Thirty-five years of Medicare Part B and D premiums $55,300. Plus, thirty-five years of 6.2% payroll deductions. $87,000. Plus, a 50% subsidy from income taxpayers, or debt owed to foreigners, as you might please to call it: $142, 360. Total lifetime expenditure (probably an underestimate): $285,000, per person.
A Three-Compartment HSA. At present, we pay for this expenditure year by year, as it comes due, in a process called "pay as you go". We are about to propose that we gradually stop that, and pay off the accumulated debt, thereby reducing the expenditures, and effecting some savings by consolidating programs from birth to death. We propose to pay off the rest of it in yearly installments from birth to death, collecting investment revenue on escrowed payments, and gradually reducing duplicate payments for the same expenses. It will be wise to collect more savings than are calculated to be necessary, just in case expenses or net revenue prove more unfavorable than we hope for. And because of the poor, a certain amount of subsidy for them is required. The government is the payer of last resort, but the program is intended to be self-supporting with interest on loans calculated in the final assessments. An independent agency is probably needed to manage unforeseen developments and make mid-course corrections. To minimize the adjustments, it is envisioned that revenue for lifetime coverage be escrowed , with a reserve fund , so the higher interest rates for long-term can be kept separate from the lower rates for short-term cash needs. Separate from both of these would be a regular Health Savings Account for yearly health costs and the averaging of yearly volatility between the funds. The lifetime escrowed fund would not be permitted to fall below current estimates of lifetime needs at that age, with interest-bearing borrowing used when it is in deficit, but no borrowing to return the debts when it is in surplus. It is envisioned that millions of accounts be reported annually, but invested collectively. It is envisioned that, after startup adjustments, the escrow fund and the reserve fund would be entirely in large-cap, domestic, total market, index funds with a maximum administrative fee no higher than that of the largest such fund on the market. The regular HSA would be entirely in short-term U.S. Treasury certificates, with an age-specific proportion kept in the reserve fund. Formulas should be devised to maintain transfers from regular to reserve, at a level maintaining only necessary liquidity for the pooled universe, but ultimately reaching for maximum achievable returns in the long-term funds. After satisfying itself with the performance of these formulas, the committee should turn its attention to the minimum deposit flow into these funds needed from subscribers to idealize returns, and then recalculate the formulas from experience. To the extent this is possible, permanent formulas for the whole structure with safety corridors should be devised and exposed to public comment, with the goal of public satisfaction that some average income experience would reflect the best possible money management. At that point, the committee should turn its attention to the developing perception of what long-term trends, combined with demographic data, are being projected for the growth of the escrowed fund to a point where the phase-down of Medicare is possible, and at what rates. The opinion of Congress should be sought as to whether these projections need to be changed, disregarding any other suggested use for the funds. Preparatory to any changes, the opinions of the professional advisory groups should be sought and forwarded to Congress. The Secretariats need not follow Congressional advice, but any deviations from it should be addressed in a public white paper and resubmitted to Congress for a white paper response sixty days before the next election.
A working example of our proposal is the average person contributing $250 per year to the escrowed compartment of a Health Savings Account, from age 28 to age 65, which reduces the after-tax, out of pocket, contribution to about $200 a year, or $4 a week. Other non-escrowed contributions to the HSA would pay for current expenses during a transition, but a certainly guaranteed revenue stream through thick and thin is absolutely necessary for the success of this idea. The source of this contribution is less critical, and if Obamacare may subsidize, this plan may also subsidize the poor to the same extent. It is estimated in our example to generate 10% tax-free income, based on the work of Ibbotson, but the expenses of the system have yet to be determined. It is intended that a private fund manager may be chosen if preferred by the subscriber, and performance records are periodically reviewed. Generally speaking, private advisors are reluctant to deal with amounts less than $10,000, so that transfer provisions should expose the fund to competition at that point, and the implications of trends should be taken seriously. The fund would continue to generate income until the end of life expectancy, here stated to be age 90, at which time it is transferred to a regular IRA. If these are close to average numbers, the individual would have at least $35,000 in the account at the time of death, and according to Ibbotson, it might be $120,000, plus another $100,00 if 26 extra years could be recovered by including childhood.
Please adjust these numbers any way you please, using the calculator provided in:
https://www.philadelphia-reflections.com/CompoundInterestCalculation/CompoundInterestCalculation.htm.
(In particular, try out your own numbers.)
Matching $35,000, the result of 3% income return, with $285,000, is about a quarter of it. Tripling the hypothetical interest rate to 9% would mean that investment income could pay well more than half the average lifetime costs of healthcare, and following Ibbotson's charts, 10% is not at all impossible over the span of a century. At the worst, however, you could surely match income and revenue by quadrupling the contributions to the HSA (to $800 yearly), which is still considerably cheaper than present term insurance costs. But finally note this well: we are planning to take actual healthcare expenditures out of the same revenue pool, so all of this calculation assumes $200-$800 in addition to current expenses for checkups and illnesses. Although the transition can muddle up appearances, a good person, or even a prosperous sick one, could set aside this much money by paying health expenses out of after-tax income (in order to preserve the tax-advantaged fund for compounding). And indeed this would happen automatically if the population continues its present pattern of sustaining its heaviest medical expenses when it is older, allowing it to compound among people while they remain young and healthy. This idea underlies Obamacare also, although the assumption that uninsured people are mostly healthy is a little dubious. It seems much safer to place the necessary money in a special-purpose escrow fund, where it could be spent away only in approved emergencies. When approved emergencies do occur, the escrow should remain unspent, and the expenses get paid by borrowing from a special reserve fund set up for this sole purpose, administered by some independent agency. Ultimately the U.S. Treasury remains the payer of last resort, so there must be Government oversight. One would hope that bad experience with Fannie May and Freddie Mac has taught us how to design such oversight.
-------- When all of the kinks and special pleading have been worked out, you only have solved Medicare. There's the healthcare for the rest of your life which has to be figured into the equation, so double it, for the purposes of discussion. It's my guess we could do it with this approach alone, but being Americans, we would try everything else first. And there is one big thing to try. We could try to lower costs. Everyone would agree there are waste and inefficiency in the system, but everyone would also agree there are lots of truly sick people to tend, and lots of important research to do, before we can assess that healthcare costs are as reasonable as we can make them.
--------- In this regard, it would seem reasonable to raise the retirement age in steps to age 70. I retired at the age of 83 and didn't feel it hurt me a bit. Ending life with a thirty-year vacation is about twenty years too much, no matter how badly your back aches.
The experience with Health Savings Accounts surprises even me. The actuaries report that the nine million people who now have HSA are running costs 30% lower than average. Whether it will scale, that is whether it will be true of ninety million subscribers, is unknowable. But moral hazards, the savings from not spending someone else's money, are not a fairy tale, by any means.
The savings to be achieved from getting tort reform are probably equally surprising. But the psychological effect on health care providers from tort reform is worth it, even if we didn't save a penny. The natural leaders of the Law Profession have always really been a decent sort. Just how the unnatural leaders of that profession gained control of the Bar Associations and Trial Lawyers Association, is open to debate. But it is high time the natural leaders of the Law profession reasserted control of it, perhaps led by the Chief Justice, the corporate law firms, the law schools, and the Judicial Conference.
In case that isn't enough, there are some suggestions to be made for healthcare cost reductions, some of which concern features of health finance which date back many decades.
Economics of Chronic Disease and Catastrophic Illness
Until rather recently, most wounded soldiers could expect to die from their wounds. George Washington died of an infected throat, an unlikely outcome today. Infectious diseases are now much less likely to be fatal, while preventive measures are in the process of eliminating fatal heart attacks and strokes. It was mentioned in earlier sections that the two most medically expensive years of anyone's life are likely to become the first and last years of a considerably extended lifetime.
If we could be sure of that, or its timing, it would make modern health insurance design easier. Some people can be expected to outlive a formerly fatal condition, and it should be possible to raise annual premiums a little to account for it. If we were smart, we would try to lower premiums by taking advantage of the extended time for investments, which results. But a new and largely unexpected health cost is the treatment of chronic conditions. That might lead to fewer diseases but more expensive ones. In the past, it was possible to regard chronic illnesses as incompletely cured ones, just a step away from total elimination. However, the cost of diseases in the chronic category has risen so much it undermines attempts to fund it with insurance. People with chronic disease are also living longer. Take atrial fibrillation, from which your author happens to suffer, as an example.
Atrial fibrillation, or AF, is a pretty common disorder whose causes and mechanics do not concern us here. It has occasionally fatal or hospitalizable flare-ups, but for the most part, the patients (before 1990) would make one or two visits to the doctor a year, for checkups and renewal of inexpensive digitalis prescriptions. It was then realized that a small but definite proportion of the patients would have a serious stroke related to forming a clot within the chamber of the heart and throwing it into the brain. That is, although the patients were living a long time with their chronic condition, they were often later actually dying prematurely from preventable strokes. Accordingly, the patients were urged to take anti-clotting pills and monitor progress with weekly blood tests. Although it is true the maintenance costs of this disorder were abruptly raised, these costs would have to be offset by reducing the costs of hospital confinement and wheelchair life at the other end of life. To that would, unfortunately, have to be added the hospitalization and transfusion costs for the rare patient whose anti-clot medication gets out of control and provokes a massive bleeding episode. The net financial cost and gain from this change of treatment have not been completely worked out, but insured patients don't much care about that; they would rather have a weekly blood test than the gruesome experience of paralysis from a stroke. One thing is clear, however. A great many people paid for their blood tests with insurance that covered them when they were 40 or 50 years old and eventually saved money for Medicare because they didn't get a stroke when they were older. The tension between the two coverages held the potential for conflicts of interest to emerge between insurers.
Going forward, further changes occurred in the treatment of atrial fibrillation. By 2012, several medications emerged which did not require the cost and nuisance of weekly blood tests. Switching over to this improved medication, I discovered that the co-payment on my insurance was $68 a month, for the pills alone. By the formula which used to apply, this would imply another 80%, or $270, was paid by Medicare to the drug industry each month. There is no way the patient can be sure of these facts in a cross-subsidy world, but on the face of it, it becomes entirely possible for the drug costs to exceed my share of the cost risk of having a stroke. Since there are several of these drugs, it is possible that competition may drive down the drug cost. In any event, the drug cost will drop substantially when the patents expire, and we will finally be able to estimate the enduring cost/benefit of the new drug compared with its blood-test predecessor. But that's probably not the end of it. Sooner or later, someone will discover a way to prevent or cure atrial fibrillation, generating a new cost cycle, we hope a final and lower one. We go through this history of a single disease entity for the purpose of asking a simple question: How can you predict future health care costs in such a violently changing environment, well enough to construct an insurance design?
You can't. You cannot predict what mixture of diseases will lie in the future, but you can rouse yourself when they start to grow in frequency. You can't predict, so you monitor. And for that you need a professional monitoring organization, preferably acting in conjunction with other monitoring agencies throughout the world while remaining in competition with them for the glory of being right. It might also be well to isolate the monitors from the regulators, just enough to enable them to criticize each other's work because they didn't participate in it.
----------------------------------------------
The line of reasoning we have been following leads to an unexpected conclusion. When the insurance company is big enough and rich enough, it can ride out occasional additions to the chronic disease category, calculate its per-person cost, and run a responsible insurance company. Just how big it has to be, and how much it has to save in reserves, will, unfortunately, vary with the state of medical science. Eventually, we will get to that end-game of first and last years of life, with only accidents, epidemics, and self-inflicted disease during the interval. My first suggestion is we stop paying insurance for the first year after a new drug's introduction, giving the insurance company a chance to know about its new cost center that was unknown when they set the premiums. The patients could get the drug, but they would have to pay cash in full. While we are being fair, we should extend patent protection by a year to compensate. It would reduce premiums somewhat, because at present they have to set aside a reserve fund for such contingencies, and there might be other ripple effects, like giving competitors an extra year to catch up.
In the meantime, we must still make a guess as to the "actuarial sound" size of a viable subscriber group. In the environment which thinks about these things, the minimum actuarial size of the group is about 2000 subscribers, but only if coverage is limited to a single year. More conservative theorists would put the minimum actuarial size at 5000 members for a one-year premium. At either size or in fact at any size, there is a small but diminishing risk that some quirk will bankrupt the insurance. Therefore, we must return to the insurance, or reinsurance, described at the beginning of this section; that is, excess major medical insurance. The difference is that its proper role is to re-insure groups, not individuals. Although the risk becomes vanishingly small by increasing the size of the subscriber group, some risk always remains for reinsurance coverage. Although there are many twists and turns to be considered, it is worth mastering these complexities. Taken all together, they explain why the insurance industry favors large groups over small ones, one-year coverage instead of lifetime coverage, and either employer-based or government-based re-insurance with a deep pocket. These are entirely legitimate attitudes for people placed in charge of insurance solvency, and woe unto anyone who accepts this responsibility without providing for its inherent risks.
However, in recent years society has been acting as if the advice of insurance executives is to be taken without understanding its parochial limits. Yes, the biggest group we can imagine is the whole nation, and the biggest re-insurance carrier would be the Federal Government. But nothing in such stipulation suggests that it would be desirable for the government to run the insurance, or for national participation to be mandatory, or for a single size to fit everyone. To get to specific problem areas, it is much more desirable to design specific programs for the prison inmates, the mentally handicapped, and the non-citizens for a total of about thirty million people -- than to twist around the whole insurance system which is serving non-retarded, non-prisoner, non-illegal citizens moderately well. To say nothing of ending up with forty million who are still excluded, and an extra cost, estimated by the Congressional Budget Office to be a trillion dollars in ten years. Along with with the introduction of all the other curses of bigness, plus a certainty of political meddling. At the very least, don't make things worse.
Secondly, there is nothing in these ancient insurance cautions to preclude the gathering of investment income on the premiums, while at the same time despairing of predicting the costs of the medical care it is assigned to mitigate. There are risks to investing, but they are accepted every day by consenting adults. There is a great deal of bad investment advice in circulation and some outrageous fees. We can expect to hear plenty of it in discussions about sums this large. But surely our political system has the wit to consult with a variety of advisors, and ultimately let the public decide whether letting our elected leaders administer the matter, is cheaper than losing the opportunity entirely.
Third. It should be obvious that there are many important unknowns in the discussion of this subject and a deficit of timely monitoring information. The nation needs a monitoring system of great probity, immediate responses of experts to sudden developments, and the power to invade privacy occasionally to get the data. It is debatable whether a monitoring organization should have regulatory power, but it certainly should have close contact with those who have the power to act. There has to be a defined pathway between the complaint of any citizen, leading to access to those who have the power to do something about it. Both the legal and the medical professions have models to examine which are centuries old, functioning well in spite of having no official power to act. The Federal Reserve, on the other hand, has the power to command and the power to investigate within its field; it is its vaunted independence which might be questioned. It could even be suggested that its independence rests on the public perception that its viewpoints are more likely to be accurate, than are those of whoever seeks influence.
Fourth. Let us have incremental patchwork, by all means. That is the conservative approach to public affairs of great moment. But until the Supreme Court finds a way to remove the anti-trust blockade of Maricopa (1982) and medical malpractice's destruction of practitioner discretion, things are unlikely to make great leaps forward. The path to influencing the Legislative Branch is perhaps more direct, but its seventy-year continuation of income tax preferences for employer-purchased health insurance sends a clear warning. The Sustainable Growth Factor (the "Doc fix") sends a similarly unfortunate signal. Fifth. But who will watch these watchdogs? The careful reader will perceive how many of the proposed reforms in this book have little to do with the Affordable Care Act, except help ACA exploit public perception that something is wrong, and relies too much on special pleading. The electronic medical record is an example, reflecting reliance on advice from group practices. The dismal failure of the electronic insurance exchanges has indelibly stained the Administration's reputation as a computer authority, so this feature is now up for political sale. Nevertheless, it remains a good idea to permit interstate competition between health insurance companies, since that could create competition between fifty actuarily-sized monopolies while encouraging other insurance companies who do not enjoy similar hospital discount prices to seek equal treatment. It is almost a century past time to insist on equal prices for equal services, by imposing a "most favored nation" requirement, or fixed relationships between hospital costs and hospital prices, regardless of whether they apply to inpatients, emergency room, or outpatient satellite clinics. Strict segregation of patient-care revenues from research funding and totally non-medical activities in teaching hospitals within universities -- ought to require no mentioning. Oversight, perhaps regulation, of the whole accounting system of the medical industry definitely ought to be a function of the monitoring system mentioned in point Three.
Indemnity and Payment by Diagnosis: Fair Prices For Healthcare
In America, the closest thing to an oriental bazaar is the auto showroom, where a salesman will spend an hour evading the price question, knowing some customers will eventually buy a car rather than spend unlimited time shopping. Lack of price transparency favors the merchant, so prices are higher. It probably does follow that healthcare prices would be lower if prices were more widely advertised and therefore, more standard.
But healthcare also varies in quality and effectiveness, so prices need to be flexible enough to compensate. Even eminent practitioners, therefore, squirm at the idea of price transparency. Flexible pricing is in fact a useful thing, without it, prices do rise, but not as much as supposed, and not without some justification. The practitioner is tangled in a web of comparisons, with his colleagues, with clinics and institutional salaries, with memories of other prices for nearly the same thing, with all the other alternatives available to a customer who can walk around and shop. Under the circumstances, the patients generally want to have a fond relationship with a doctor they can trust to know what the market is saying, and trust him to make the best guess about what his own services are worth. Therefore, a physician is a fiduciary, expected to put the patient's interest ahead of his own. Insurance is not a fiduciary: Our modern third-party system systematically replaces trust with: standard prices, blind faith in low prices as always better than higher ones, and determination that medical quality had better always be top-notch, or else we will sue.
 Competitive market solutions are never an even match, once someone takes away your clothes. 
|
The best way to handle the situation is to pay, in part, by indemnity. In effect, indemnity makes the promise to pay $800 for a gastrectomy. If the surgeon thinks he is worth more than that, it must be agreed to by the patient in advance and paid out-of-pocket. Not paid in advance, agreed to in advance, with the implicit understanding it can be reduced by sincere dispute, after the fact, and without recourse before the fact. Back at the beginning of the system, this feature was bargained away. I cannot resist telling the story of my father-in-law's advice to me, doctor to doctor, at the time of my wedding. "Never let your wife keep your books," said he. "To you, the patient is a poor old devil down on his luck. To your wife, he just represents a steak dinner, if she can collect the bill." Our third-party payment system has succeeded in projecting the image of protecting the patient against voracious "providers of care", just the reverse of their natural postures, and something my father in law never dreamed of. It's very simple: basic payment by indemnity, extras by a negotiated patient supplement. Since consumer representatives are so intransigent about "give-backs", it might at well include a COLA on the basic, and otherwise put inflation into the patient supplement.
 It's very simple: basic payment by indemnity, extras by negotiated patient supplement 
|
At present, DRG is mainly forcing patients out who was once enticed into the hospital by the previous payment system. Once that backlog is exhausted, the DRG pressure will start to hurt, since all rationing systems lead to shortages. Like the Volstead Act, this government mandate was successful in its original purpose, but the unintended consequences were worse. When DRG starts to hurt, a new coding system had better be ready. Because the resultant growth of hospital outpatient services has been so extreme, it will cause a bigger bubble to burst unless attention is given to service benefits inflating the cost of outpatient care. To repeat, the cure for medical cost inflation is not to apply rationing, it is to improve the payment methodology so that rationing is unnecessary. The current repetitious chorus denouncing fee for service is just a cry of desperation from people too unimaginative to devise any substitute more sophisticated than salaried rationing. The problem here is not fee for service, it is service benefits. And the problem lies, not with the provider, but with the carefree beneficiary -- carefree because he is insured. And furthermore the solution is not salaried practitioners bossed by salaried politicians, it is a hybrid of indemnity with basic pricing. Under Health Savings Accounts, we bring the public into power over its own affairs. The remaining problem is to let the individual control his own monster, by making waste and luxury his affair, not an affair of the public at large. A good beginning would be to forbid the use of collection agencies, forcing the institution to confront its irate customers.
Diagnosis Related Groups (DRG), in Relation to Medical Electronic Records.

|
| The American Medical Association |
For a concept supposedly working moderately well, the Diagnosis Related Groups (DRG) system for inpatient reimbursement has a bizarre history. It has led to some unconfessed, and widely unrecognized, disastrous results, and should be thoroughly reworked as soon as possible. In a scholarly sense, the story begins eighty years ago. The American Medical Association decided all of the diseases, ultimately all of the medical care would be better understood if reduced to a systematized code. Originally, the code was visualized as a six-digit complex, with the first three digits defining an anatomical location, followed by a second set of three digits specifying the cause of the disease affecting that location.
SNODO That 6-digit structure limited code to a thousand diseases in a thousand locations, or a million "disorders" just for a beginning. Roughly half those theoretical combinations have no biologic existence, although even fanciful codes had some value for detecting coding errors. Other regions of the code exceeded the number of conditions actually found to exist, but originating in a digital structure then allowed virtually unlimited expansion, but sacrificed the significance of a particular position within the code. IBM was enlisted as a consultant, who advised the AMA to stop worrying about it; just provide a numerical code for everything, in the finest detail possible. Mathematicians could later easily make it usable for calculating machines, the forerunners of computers; and non-existent conditions created no harm. Some of those consultants had worked with a system which produced great success for the U.S. Census and perceived no advantage to limiting the code numbers while planning for them to be manipulated by machines. The third group of three digits was soon added, making a nine-digit Standard Nomenclature of Diseases and Operations , familiarly known as SNODO, which could identify a million different operations, whether actually performed or not. Actually, groups of three or more digits separated into groups of three digits by hyphens transferred the significance of code-position to the cluster level, which proved adequate.
SNOMED The pathology profession subsequently added still the fourth set of digits, for microscopic features, so the potential was soon up to a hundred million microscopic conditions. The team of physicians who worked on coding the medical universe contains many names now famous, notably including Robert F. Loeb and Dana Atchley of The College of Physicians and Surgeons of Columbia University. For at least thirty years, the Joint Commission on the Accreditation of Hospitals (an AMA and AHA joint affiliate) enforced a rule: every discharge summary from every accredited hospital in America must code and index every discharge diagnosis in SNODO code. It was tedious work, kept alive by the glittering future prospect of developing an Electronic Medical Record by 1940.
|
| Robert F. Loeb |
ICDA After twenty years or so of this enormous task, the Medical Records Librarians rebelled. The labor effort was burdensome, and the librarians were in an occupational position to observe how little use was being made of it. On their demand, an alternative simpler coding system was adopted, called the International Classification of Diseases (ICDA). At first, it was limited to the one thousand commonest discharge diagnoses , therefore limited to the charts which the librarians could confidently observe would be used. In time, it was expanded to ten thousand commonest diagnoses. Limiting medical codes also limited the cost and effort of coding and was considered an important retreat from over-enthusiasm. Meanwhile, expansion of the SNODO code by a handful of true believers continued to fill up the coding gaps, soon using and exceeding the capacity of the 80-column IBM punch card (originally, ten digits plus metadata), one card per diagnosis.
Unfortunately, the code was in danger of collapsing from this unanticipated expansion, since computers had not yet advanced to the point where they could rescue SNODO from the limitations apparent to its users. It was a classic case of a hypothetical system appearing to be better than the one in actual use, but not living up to its promise when both systems encountered actual use. The ICDA coding scheme did suffice for immediate purposes, and the "calculator" system was at least a decade away from evolving into the more flexible "computer" which could skip around the limitations of a punched card input system.
The professional difference was this: the doctors roughly understood the coding logic and could devise an understandable code for most charts through the logic of a structured language. The record librarians had not been trained to encipher (or even dither, as photographers say) the code by logic; a thousand codes was about the limit of what anyone could memorize. The burden of manual coding eventually overran the code design, before practical results could defend its utility in other areas of the hospital or the profession.
All the medical record world promptly abandoned SNODO; except for the pathologists who intuitively recognized ICDA could never approach their own greatly expanded needs. Eventually, pathologists took SDODO over, expanded and redesigned the basic framework, and produced what they are rightly proud of, an elegant codebook called SNOmed which obeyed meaningful internal coding rules. It still came, however, as a large and expensive book, which most practitioners were reluctant either to buy or to use.
|
| Dana Atchley |
DRG Meanwhile, a group at the School of Hospital Administration at Yale under the leadership of John Thompson lurched in the opposite direction of drastically reducing the ICDA code (initially expanded to 10,000 entries, which proved too large for some purposes, while still lacking specificity in many others), back down to only 468 of the commonest "diagnosis clusters". The purpose was to find clusters of diagnoses with common characteristics, which could be used by unskilled employees to identify diagnosis submissions which normally fell within certain bounds, but who in a particular case were sufficiently deviant to warrant investigation as "outsiders". This gross sorting by machine was then examined by the PSRO (Professional Standards Review Organizations), especially in the central feature of the length of stay. They termed their product Diagnosis-Related Groups (DRG) , which made no pretense of being complete but was complete enough to encompass the majority of outrider events. The computer version of their concept was called Autograph, which had some attraction to hospital administrations as a way to predict outriders. To summarize what happened next when Medicare adopted DRG for payment purposes: both DRG and ICDA started to expand, and SNOMED was relegated to the role of the codebook for Neanderthal pathologists.
 Two million diagnoses are compressed into two hundred payment groups. 
|
| Diagnosis "Related" Groups |
Using the standard diagnosis codes, one-size-fits-all did not help the hospital and insurance accountants a bit, since my habit they tend to believe all businesses are about the same, no matter what the business produces. Their complaint was coded with thousands of codes were too big and complicated. Simultaneously the medical professionals were finding them much too small for the job. Meanwhile, ICDA was fast losing its reputation for being compact and inexpensive, while the opposite feeling immediately developed: the DRG was far too small for what physicians could now realize was going to play a very large and important role in everybody's finances. Two vital areas of the hospital had difficulty communicating from the beginning; now, there was no longer even a common language to use. There was no quick fix, either, because both DRG and the underlying ICDA designs were based on the frequency of occurrence, rather than precision and logic. Furthermore, the copyright was owned by professional societies who had little interest in finances, and considerable interest in reducing their burdensome coding workload. In the background, however, computers had made the task of code translation a trivial one. A third profession, the computer department, scarcely knew what the other two were talking about, but they came closer to affinity with the accountants.
Like the three bears of Goldilocks, some codes were too large and some were too small, but at least there were three of them, each crippled in a different way. Comparatively few doctors understood what was going on, and in spite of their vital interest at stake, had trouble getting over their hatred of the boring coding task. Since this whole issue of data coding and summarization has taken on major importance to the success of the Affordable Care Act, in some circles the uproar has become a political war dance. Let Obama do it if he likes coding so much. Basically, the librarians were saying they resented being criticized for making important mistakes in a task they didn't understand very well. In summary, everybody hates coding.
Overview of the Future.One a faction of the small field of those who are interested in such matters has decided to expand both the specificity and the reach of ICDA, which is now up to its tenth edition of revision. Unfortunately, it does not seem to some of the pathologists to be a sensible approach. We have an elegant code in SNOMED, they protested, which is arguably too big to use; expanding ICDA seems destined to reach the same destination, on the rebound from being too small. We now have ample data on what is common. The most efficient approach would at first seem to be condensing the highly specific SNOMED to a useful size, based on the frequency of use. The approach would stand in contrast to making a list of diseases by frequency, and then subdividing their specificities. While such a condensed volume could be printed as a book, we are now at a point where every record room within the hospitals of the nation is equipped with several computers, so the elasticity of the code should no longer be anyone's problem. Let the machines do the drudgery.
This whole process could now rather easily be automated for much more than its original purpose of classifying disease populations, and in a pinch it could even substitute 26-digit letters for 10-digit numerals, imparting some clues in the process. Further condensation of an already condensed version began to be used for payment purposes, adding still greater amounts of practical nuance. You might suppose everyone could see paying the same amount of money for treating the same disease (tuberculosis, let's say) of two different organs (let's say of bone, and of the kidney) was either going to bankrupt someone or enrich someone else. And that's only money. Any scientific or diagnostic decision based on a code of "All other" will make computerized medical records sprint faster toward worthlessness. At the rate it's going, lumps of "all other" will have no relation to each other, except to justify the same reimbursement for treatments of vastly different value. Or difficulty. Or cost. Or contagiousness.
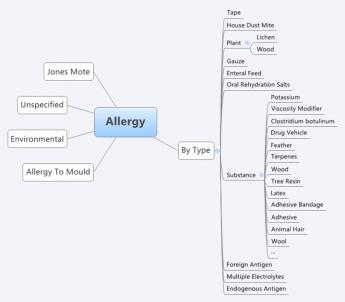
|
| SNOMED |
In automated form, SNOMED is quite ready to be revised still further in other directions for other purposes. It could, for once, integrate the accounting and demographic functions with the rest of medical care. But a great many other useful functions can be imagined, once computers have a stable platform on which to build, and the task of coding can be safely undertaken without much physician input burden. Safe, that is, from the danger, the whole coding framework will get changed, again and again. In a certain sense, this is similar to the brilliant choice by Apple of the Unix skeleton, when Microsoft Windows seized on quicker expedients. A great many sub-professions seem to wish to have their own codes for their own purposes and resist the idea a physician code should be imposed on them. When you encounter such obstructionism, it is easy to suspect motives. But the general rule is: when it comes to a choice between scheming and incompetence, it's incompetence, nine times out of ten.
However, medical care and hospital care are medical functions, and their accounting and demographics will always eventually return to their medical professional core. Meanwhile, notice what happened to DRG, a code so crude it relegates most refinements to the category of "All Other". The fact of the matter is, it is a crude approximation, some cases paying on the high side, some on the low side of true costs. If the hospital loses money on inpatients, well, just build another wing to the outpatient department. Underlying this response was the enduring misconception that outpatient care is inherently cheaper than inpatient. If it's the case, well, we'll just have to fix it.
The surprising lack of chaos from such experience has almost nothing to do with medical content, and almost everything to do with having insufficient case volume to remain in balance. That is, the big hospitals smudge it out, and the small hospitals don't understand it. The highly prized profit margin of 2% or 3% can easily be achieved by admitting slightly more cases of a profitable kind (ie hire a surgeon expert in certain profitable operations), or by the government adjusting just a few DRGs to profitable status (like reducing tariffs on behalf of favored industries in Congress). Meanwhile, the rest of the enterprise becomes progressively more expensive, because there is no fixed relationship between service benefit prices and audited costs, and now an even less regular relation, to cost-to-charge ratios.
It is a precarious thing for institutional solvency, to depend on a financial balancing of a particular caseload within one set of four walls, and then complain hospitals are too small to survive. Between their accountants and their record librarians, this outcome drives the smaller institution into a futile chase after higher patient volume. Of course, we need to change with the times. But some basic truths never change, and one of them is every ship should be able to sail on its own bottom. You don't approach that by giving every ship a new hull.
Let's get specific. In the first place, allowing only a 2% profit margin during a 3% national inflation is to walk on the edge of a dangerous cliff. If some fair profit margin could be agreed to, it is only an average among hospitals. You might as well reduce the DRG to four payment levels, and reimburse hospitals on the basis of which of the four walls the patient faces. With enough tinkering, you might arrive at the desired total hospital reimbursement to match any profit margin you establish, totally disregarding the diagnoses of all patients. Quite obviously, you must code the diagnosis to whatever number of digits it requires to identify the unique condition. You could match up all of the hundred dollar cases and all of the fifty thousand dollar cases, call the two codes, and pay only two prices.
But such an effort is just a delusion. Somebody-- or some machine-- has to go to the trouble of coding every single diagnosis down to the point where the code is no longer meaningful to costs and assign relative values among them. Only at that point would it be legitimate to assign a dollar amount to each relative value. You have to maintain the code as treatments change, which will be quite frequently. You can do it, and you can computerize it. A computerized version of this process would scarcely be any different from copying the English description and, like a Google search, getting back a number to copy; it might even be done by voice transcription. But there is still no guarantee charging itemized bills wouldn't turn out to be cheaper, and at least have a different meaning. DRG in its present form is nothing but a crude rationing system; get rid of it, or spend the money to make it work. I can't guarantee if you put a doctor in charge, it would work. But I can guarantee that if you don't put a doctor in charge, it won't.
Proposal 5: Congress should be asked to commission a computer program to translate English language diagnoses into SNOMED code, preferably by voice translation. Suggested format: a search engine where English variants of discharge diagnoses are entered, and a SNOMED code number returned, along the general lines of entering common phrases into Google and receiving file location numbers in return, except it returns the SNOMED code. If the code is not found, the computer accepts a manual entry by a trained person. verified by an expert over the Internet to become officially entered into a master list which is periodically circulated as an update. The search program and its supplements should be produced on DVD disks to be used on hospital record room computers by other professional users. It should provide "hooks" so the Snomed codes and patient identification can be transferred electronically to related programs, such as payment codes and billing.
So that's how DRG got to be what it is. It's perfectly astounding such a crudity, devised for other purposes, could be so "successfully" employed to pay for billions of dollars of Medicare inpatient care, such that payment by diagnosis-lumps threatens to spread to all medical care. There is even another way to describe it: inpatient hospital care has been lumped into a rationing system which constrains national inpatient care to a 2% overall average profit margin. That's just as surely true as if someone deliberately tried to make it that way.Payment by diagnosis ignores both cost and content, based on the mistaken assumption those features have already been carefully accounted for. It does not matter in the slightest how long the patient stays or how many tests he gets, or how many expensive big hospitals swallow up inexpensive little ones. Meanwhile, emergency rooms and satellite clinics also do not affect the cost inherent in a supposed linkage between the diagnosis and the cost. The failure to link drug prices into this modified market system is particularly noticeable.
The exciting potential has been lost to have the patients who can shop frugally as outpatients, set the price for inpatients who are helpless to act frugally. Their much more generous profit margins support what is essentially a hospital conglomerate. Any corporate conglomerate executive could tell you what happens when one department is subsidized, while another is treated as a cash cow. And the fun part is this: squeezing physician income against an unsustainable "Sustainable" Growth Rate creates the "doc fix", which annually blackmails physicians into acquiescence past the next November elections.
SGR: Sustainable growth rate, earmarks by a different name. SGR is a term borrowed from financial economics, signifying the rate at which a company is able to grow without borrowing more money. It is easily calculated by subtracting dividends from return on investment. Any variation from this definition will produce different results. A sustainable growth rate in Medicare is calculated by a formula, modified every year in special ways which closely resemble "earmarks", but contain special adjustments for changing work hour components, malpractice cost components, etc. It is a large task for the Physician Payment Commission to determine yearly changes in thousands of services, and it must be frustrating for them to see their painstaking calculations tossed aside every year by Congress, in response to howls from the various professions. Whenever this occurs it is a fair guess the calculation has been misused. The discussion has long since transformed from a simple calculation to a simple threat: physician reimbursement will be cut. Each year it is cut, and each year Congress relents on the cut at the last moment. But ultimately its design will prevail: on the pie-chart of healthcare expense, physician reimbursement will shrink, and hospital reimbursement will expand, as physicians migrate to salaried hospital employment, and enjoy an instant 40-hour week amidst a physician shortage. This keeps the AMA in a constant state of agitation, and physicians in a constant posture of supplication. At the end of 2013, the proposed cut in reimbursement had grown to 26%. When almost every physician has an overhead of 50%, a cut of 26% is beyond meaningful. And every year the financial attractiveness of joining a hospital clinic for a dependable salary grows, with consequent improvement in the overall power of the hospital conglomerate, and steadily decreasing relation to market-set pricing readjustments.
Insurance Reimbursement, The Missing Item on the Itemized Bill. The DRG system threatens patients, too. After discharge from a hospital, the patient is sent a multi-page itemized bill, which purports to be what the patient would owe without insurance. Such bills traditionally omit any mention of the insurance reimbursement, which is the only payment the hospital receives if it has contracted to accept "service benefits" as payment in full. Since that is almost always the case, the "total of service benefits" is exactly equal to the "total patient responsibility". Since the patient will pay nothing if patient responsibility is limited to service benefits, and service benefits are exactly equal to whatever the patient received, the explanation goes round and round without ever revealing what has been paid. The illusion that you have been told something worth hearing, is maintained by providing an almost endless list of itemized charges.
Most hospital employees do not have the foggiest idea why the list is even produced, and its accuracy is therefore questionable. A variety of specious explanations, therefore, emerge, usually with a focus on billing a handful of uninsured people, or insured people whose service benefits have expired as "outsiders". There may be a particle of truth to this, easily refuted by showing the supposed items on the bill were often fabricated by employees who know very well they are seldom used for anything. Most likely, the purpose is to conceal the true insurance reimbursement from competitive insurances who might undercut them. As profit margins shrink, it becomes increasingly dangerous to let competitors know what they are. As margins widen, it is even easier for competitors to undercut them. As a matter of common observation, most retailers in any business are less than forthright about their profit margins, so perhaps this concealment can be forgiven as normal commercial behavior. It becomes more questionable when seen as an industry-wide practice, intended to defend a system of double-pricing. In this case, it defends the employer tax discount as the lowest price around, when compared with those rascals, the uninsured or the insured but fully taxed.
The DRG payment to the hospital is not zero, but it is far less than the total on the itemized bill and is seldom revealed. One central message it sends is however pretty clear: "This is how much you would be charged if you didn't have Insurance X." The shortfall in revenue is made up by overcharging the emergency room and the outpatients, who are unsuitable for anything resembling the present DRG. If the hospital does not have enough outpatient work to sustain the inpatient losses, its only recourse at present is to call the architects and build a bigger outpatient department. To fill it, just buy up a neighboring group practice or two of neighborhood doctors. Fix the DRG, and it would be hard to say what would eventuate.
Bottom Line: Who is Injured? For a long time, service benefits insurance was the only thing supporting the hospital industry, and commercial behavior by the hospitals was justified as the only way to support their charitable mission. Now that Health Savings Accounts have reached 12 million clients, with assets reaching $22.8 billion, a viable way to provide indemnity insurance has definitely arrived. Not only are HSAs cheaper for the customer, they very likely provide higher payments to hospitals. This last point will only be clarified when we learn what discounts the catastrophic high-deductible insurance have been able to extract, but hardly anything else will affect the answer. To the extent one competitive method receives major discounts and the others generally do not, this service benefit discount is probably only of benefit to the insurance companies who enjoy it. A personal episode in my family illustrates.My son went to a well-known Boston hospital for outpatient colonoscopy and received a bill for $8000.00. When told that was outrageous, he protested and promptly received a bill reducing the charge to $1000. He was delighted to send a check for that reduced amount, even though I told him a fair price was probably around $300. He reminded me of a comment from a famous surgeon now deceased, whose name is emblazoned on a tall pavilion in another city. The old surgeon growled, "The only reason to carry health insurance is to keep the hospital from fleecing you." In a sense, that growl applied directly to the colonoscopy, which that hospital had converted from markup into a holdup.
Discounts for Health Savings Accounts? HSAs scarcely have to penetrate the market much further before they have the market power to command an equal discount. That may still take a little time, because some states have hardly any penetration, while California has a million subscribers. In the meantime, the patient needs to be careful to ask for prices in advance. Almost every health insurance has started to impose high deductibles, so their proper stance is to insist on equal treatment. The old system of "First-dollar coverage" was responsible for making outpatient care a target for this sort of thing. The next advance, after making all outpatient care match market prices, is to insist a hospital charge the same thing for the same service for inpatients as it does with outpatients. To make that possible, it has to return to fee-for-service billing, and management of Health Savings Accounts should settle for no less. That's the main reason DRG billing offends me, although there are lots of other reasons, and lots of other people are injured in different ways.
An Unending Capacity to Generate New Problems
There is a fair amount of seemingly unrelated detail until we reach the point of this article, where we conclude it really is possible to design and pay for lifetime health costs with the tools we already have, using individually owned lifetime policies. As a part of that, it really should be possible to substitute cost shifting between the youth and the old age of one person, rather than the present kind of cost shifting from one person or group to somebody else. People don't mind taking from one of their pockets and putting into a different one. But fierce possessiveness appears when you shift from my pocket to your pocket, and the health system is riddled with it. "Riddled with cost-shifting" seems to imply underhandedness. In fact, only the simplest businesses could survive without such flexibility. The problem with cost-shifting in medical care is there is so much it, even carried to the extreme of performing carefree, with blithe indifference about how to pay for it. Just review how accustomed we have become to cost shifting as the only possible thing to do.
From the outset, Blue plans announced their business model: patients in the private rooms supporting the care of indigent patients on the wards, up to then entirely supported by the charity. Plus a third, intermediate class of say ministers and school teachers, called semi-private, who were financed on a strict break-even basis. Summary: rich people supported poor people, and the semi-privates broke even. At first, there was just a handful of semiprivate, but after a decade or so, just about everybody was semiprivate, defined as two strangers in a room. Blue Cross had an enormous unintended effect on hospital architecture. When Medicare and Medicaid adopted the same philosophy, the semiprivate room became the standard. If the rooms were small (and cramped) the nurses didn't have to walk so far, but the main driver was the insurance reimbursement formula, which was based on square feet of floor space. A square foot of such space was used as a cost basis for non-patient space in the overhead formula. Eventually, hospital architects were receiving demands for bizarre room sizes, in order to affect the reimbursement formula. The tail was beginning to wag the dog.
t During that era, charities were payers of last resort, unless creditors were stripped by bankruptcy. Furthermore, to provide a full range of services, some services lost money, subsidized by other departments which generated a profit. Any corporate executive could tell you what came next: the profit centers start to boss the losers around. In group practices, surgeons generally still subsidize primary care ("the feeders"); state Medicaid is roughly 50% subsidized by federal Medicare, and after hospitals are paid, underpayment by Medicaid is balanced by the hospital from other sources, once again mainly from Medicare until payment by diagnosis (DRG) came along. It is when one insurance competitor is forced by internal hospital cost-shifting to subsidize its rival, that most of the outcry is heard. Employer-basing leads to different subsidies between insurances, and by a two-step process, one competitive business subsidizes its fiercest competitor. Generally, a business does not care what things cost, so long as competitors must pay the same price. In the eyes of business, trouble comes from unequal cost-shifting. Its mere suspicion is almost as bad. Working-age people subsidize the generations too young or too old to work. That is obviously what must happen indirectly and unofficially, anyway. Cost-shifting is a normal business practice, an absolutely necessary one, but the cost shifting of hospital costs is almost beyond belief. Because now, no one can tell what anything costs, and because patients who are business employees will reflect the attitude that the absolute amount doesn't matter, only that competitors must pay the same. In short, cost rises meet little resistance.
What brings the matter to a crisis is payment by diagnosis, where it doesn't matter how long a patient stays or how many tests he has, the insurance payment to the hospital is the same. Added to a determination by Medicare to cut costs, the result is that the profit margin for inpatients is around 2%. From the payment designers' point of view, it's an excellent rationing system. But it isn't, because hospital architects are directed to shift their lavishness to service areas with greater profit margins, like emergency rooms and satellite outpatient clinics. The next time you see a building crane at your local hospital, just ask them what kind of building they are putting up. Having spent a fortune twisting hospitals into one kind of shape, the reimbursement system is twisting a new shape, and rather oblivious about it. At the same time, two-bedrooms are being converted to one-bedrooms to attract a carriage trade and justify a higher price. Maybe, just maybe, the bed capacity is somewhat smaller at the end of responding to a pitiful profit margin for inpatients. Changing demographics are also a factor. Trends toward unsustainable cross subsidies grow steadily larger because the contribution of working people is certain to get proportionately smaller. Extended longevity increases the proportion of young and old dependents, boosting the costs of working people by the fact that their shrinking proportion must ultimately pay for all of it. Ultimately, all hospital revenue originates with the working segment of the population. Parents pay for their children, and payroll deductions pay for the elderly grandparents. Working people are supporting it all. Let's not overstate: disappearing infectious diseases reduced the mortality and hospitalization of working people, too. The elimination of polio and tuberculosis was a dramatic godsend but made it harder to finance a general hospital, because of the shrinking client base of employed people. The way things are going, health costs should eventually concentrate in the first and last years of life, with hardly any serious illnesses for the people in the middle years of life who ultimately pay for every bit. Hospital cost-shifting can not indefinitely support its own system because working people will have so few medical expenses it becomes impossible to hide very much within them. If you want to know why payment by diagnosis was welcomed, just reread the last three paragraphs. Unfortunately, if payment is based on diagnosis, it doesn't matter how many x-rays you have, or whether all the door handles are polished brass. We badly need a new way to charge inpatients, and just about every system has been tried. Unfortunately, it took a long time to get rid of payment by the square foot, and it will take a long time to get rid of payment by two hundred very approximate diagnosis groups, or DRG. The very least that could be done is to substitute a better diagnosis code, like SNOMed, for the private ICDA, so that payments are seen to be driven by the right diagnosis, which might tell planners something useful.
 How could we have created individual policies that failed to reward customer loyalty with guaranteed renewal? Or monopoly status, to companies without guaranteed issue? 
|
| Lost Opportunity |
 Medicare would pay terminal costs as before, but be reimbursed by the escrow fund. 
|
| Transfer Vehicle |
 Malpractice costs are disproportionately concentrated in Obstetrics. 
|
| Who is doing the suing? |
The second redirection of attention would be to campaign to lower the age at which American women have their first child, greatly reducing neonatal problems, including infertility measures and congenital malformations. Absorbing the cost of having a baby ought to assist this effort, otherwise highly desirable on purely medical grounds. Unfortunately, our system of graduate education and career advancement will incentivize timing conflicts with biologic goals. Society will have to work these conflicts out in its own way, but at least we can adjust health insurance timing to be more in keeping with societal trends.
Finally, it should be said that the Health Savings Accounts are a vastly simpler way of paying for health care than using the service benefits approach, and the payment system greatly needs simplification. Using a high deductible has the potential to preserve market benchmarks for prices which are otherwise going to induce unworkable price controls, permanently. The system of "first dollar coverage" was accelerated by a wish to include as much as possible under the Henry Kaiser income tax evasion, and it will return if we neglect to correct that flaw. Experience with Health Savings Accounts has demonstrated as much as a 30% reduction in claims costs. Linking market-set outpatient costs to the same services when provided to inpatients should be an adequate price control for helpless sick people since an improved system of diagnosis-related groups should accomplish most of it. But the main advantage is to reduce these fund transfers to money without health attachments, to make unification and substitution more plausible. That is, to eliminate "service benefits" and not replace them with "diagnosis benefits" except for helpless bed patients. A return to dollar indemnity is greatly needed, although perhaps not totally.
To a considerable degree, service benefits are in conflict with indemnity benefits, in a manner resembling the conflict between debt and equity in the financial sphere. At some point, there must be a reconciliation between these two ways of paying for things, especially by keeping indemnity consistent with market prices. The best one can hope for is to shift the location of the interface between service benefits and indemnity, bringing the friction out into public view, and equalizing the power of the sponsors. Therefore, the best place to hold the debate is to treat diagnosis groups as inpatient service benefits, and outpatient costs as indemnity. With reasonable exceptions, of course. One of the main mistakes of the DRG system was to extend it to every inpatient. Inpatient psychiatry should be paid for as if it were an outpatient service, and chronic diseases such as Alzheimer's disease should also be excluded from DRG as well. Emergency room visits should be separated into two groups as well (admitted to hospital and discharged home), with reimbursement slanted to reduce the incentives for unnecessary use of the Emergency room, not the other way around as it is at present. The whole trick here is to see the double reimbursement situation as an opportunity for constantly rebalancing the two approaches, rather than allowing it to be pounced upon as a loophole.
We started by saying these issues should be chipped away, during the period when more important issues are being addressed head-on. But the list of small issues is a long one, providing ample opportunity for trade-offs in ambiguous opportunities. More than anything else, the endless capacity to develop new problems demonstrates the need for careful construction of an institution to serve as an informed and trustworthy umpire.
Classical Health Savings Accounts (C-HSA)
Cost Shifting: Indigent Care Out, Outpatient Revenue, In
The CEO of Safeway Stores recently offered his company's preventive approaches as an example of what the nation can do to reduce health costs. He's undoubtedly sincere, but quite wrong; Safeway just shifted costs to Medicare. This is only one of several ways, major ways, cost-shifting is misleading us. Let's explain.
Average life expectancy is increasing at more than two years per decade, but of course, people eventually die. Since health care costs are heaviest in the last year or two of life, extending life will soon push nearly all those heavy terminal costs from employer-based insurance -- into Medicare. To die at age 64 costs Blue Cross a lot; but to die at 65 gets Medicare to pay for it. Either way, the cost is exactly the same, it doesn't save Society as a whole any money at all. Let's put it another way: dying at age 64 costs the employer and the employees, but dying at 65 costs the taxpayers. This means Medicare costs will surely rise, but in this case, it's a reason to rejoice.
Increasing longevity is constantly pushing more costs from employers to Medicare, and not just in Safeway; the prospect is that soon substantially all major sickness costs will shift into Medicare. (To explain the failure of most employer insurance premiums to fall comparably in response to this shift, one must look elsewhere). But just a minute. Medicare is 50% subsidized by the government, and the employer writes off half of the cost as a business expense. That ought to mean it doesn't make much difference to anyone involved, except for one thing. Some employers have two employees and some have two hundred thousand employees. The amount of tax write-off is multiplied by the number of employees, so some employers can only write off a little, while an occasional employer might even make a profit on using health insurance for calisthenics. Economists agree that fringe benefits eventually and proportionately come out of the pay packet, so ultimately the employed patient benefits from the reduced bill, his employer pays less, and the Medicare costs the taxpayers more.
<But instead of going down that trail, let's look at the second form of cost-shifting. Government payers and a few other monopolists are able to pay hospitals less than actual costs and get away with it. The worst offenders are state governors administering Medicaid, where the underpayment is roughly 30%, in spite of federal reimbursement to the states for most of it, at full price. The resulting profit is used for various state purposes, mainly nursing home reimbursement. For the most part, such diverted funds are used for purposes not easily eliminated, so it is unlikely there will be much cost reduction for the government if the scam is acknowledged and merely shifted to a different line in the ledger. To avoid bankruptcy, hospitals raise the rates for other health insurance plans -- and the uninsured. Employers are paying for most of it, so they stand to gain from reform, only to face higher state taxes as matters readjust. We have yet to learn where these costs will shift if the federal government takes over the costs of the uninsured; the current Obamacare plan is to shift 15 million uninsured persons to Medicaid. To a major degree, the federal government and its taxpayers are already paying for a lot of this uninsured cost, through the Medicaid shift. So its present dilemma is whether to continue to pay for it twice.
There's still a third cost-shift. In 1983, Medicare stopped reimbursing hospitals fee-for-service (itemized inpatient bills are still prepared but are meaningless fictions) and for thirty years has paid by the diagnosis, not the service, for inpatients. Consequently, per beneficiary inpatient costs have only risen 18% in five years, while outpatient costs have risen 47%. Costs are not the same as prices, which are even worse distorted. To a large extent, changes in costs are really changes in accounting practices, driving changes in actual practices. Skilled nursing and home care costs are rising even faster. When you hear fee-for-service payments attacked, it is this apparent overpayment of outpatient costs which is the source of the complaint. But to pay out-patient medical costs in any way other than fee-for-service would imply an almost unimaginable restructuring of the medical system, without any proof it would save money. It will be very interesting to learn what contorted proposal is about to emerge.
 Medicare +6% Medicaid -30% Private Insured +32% 
|
| 58% of Hospitals Lose Money |
Not only do these shifts provoke inpatient nursing shortages, but they also start a war for patients between hospitals and office-based physicians. Hospitals are winning this war for business, but are losing money doing so. If the public ever demands a stop to loss-leaders, net insurance premiums will probably rise. The difference between a hospital which makes money and one which loses money is based on whether there is enough extra out-patient revenue to compensate for the hidden tax which the state effectively imposes on hospitals in order to pay for nursing homes. The obscurity of the present payment system is quite expensive, and the present beneficiaries of it are the Medicaid nursing homes. Obamacare essentially provides health insurance to 15 million uninsureds by the process of placing them on Medicaid, so the consequences are going to be an interesting juggling act to watch.
 5-year Change: Inpatient +18% Outpatient +47% 
|
| 5-Year Hospital Costs |
Just notice, for example, that neither Medicare nor private health insurance pays below costs if you look at total national balances. Private insurers are paying hospitals 32% more than actual inpatient costs, while Medicare is paying 6% more than national cost. And yet 58% of hospitals are losing money. The magic in this formula lies in the losses incurred by state Medicaid but shifted to other payers. It could fairly be said we are just looking at a maldistribution of the uninsured, as a cost, and a maldistribution of non-inpatient revenues, as a profit, among the nation's hospitals. To what extent such maldistribution reflects uneven patient quality, as the loser hospitals claim, or provider inefficiency, as the winner hospitals would say, -- merely starts a distraction of attention which could last twenty years while we examine it.
And disruptions enough to take decades to fix.
Cost Shifting, Reconsidered

|
Cost-shifting is a necessary accounting evil, without which no large organization could survive. Confusingly large amounts of it, however, undermine trust in the leadership. More specific criticism of current healthcare leadership is its reliance on moralizing rather than an apology. That is a sure sign that oppressors (i.e. insurance and government) made it necessary, and suggests that leadership is toadying to them.
Since managers have no choice but to engage in cost-shifting, it seems better to cost-shift with some hope of repayment. By switching to lifetime health insurance to replace the one-year version, many more opportunities can be developed for repaying the older individual what had been "borrowed" from him as a youth. Even without the notion of paying interest on the loan with investment proceeds, it seems more comfortable to seek loan forgiveness from yourself at a later stage of life, if that proves the necessary insurance metaphor.
The proposal to revise insurance architecture also contains a transfer of the site of cost-shifting from hospitals to the external insurance mechanism, where the underlying problems originated. There is a certain justice to that, but its main attraction is to make it visible and consensual, and therefore more generally accepted. It is one thing to convince a classroom of business students, quite another to convince the whole public, of the regrettable need for cost-shifting that will never seem completely fair.
And finally, there is the investment income. The public is no more likely to forgive its mercenary features than it is to accept that bankers are interested in more than profits from the interest on a loan. After all, interest-bearing loans were forbidden by law for centuries. When it first hears of the fairly astonishing 10% return from a passive investment, and the even more astonishing sums to be derived from ninety years of investing, the public will likely scoff at some sort of trickery. A great many people still prefer managed accounts to passive ones, in spite of Professor Ibbottson's rather convincing data from the immediately preceding century.
Two sources of concern are nevertheless impossible to answer. America may lose its dynamism, as even the Roman Empire eventually did, and nothing can withstand the financial consequences. And secondly, so many people might switch to passive investment that it loses its edge, and eventually pays less than hiding all savings in a mattress. That is to say, high returns imply high risk; without risk, there will be no returns. These considerations are long term and have nothing to do with healthcare. For this reason, I have reluctantly made the suggestion that we establish an independent organization, for all its flaws, to study whatever is happening and continuously make mid-course corrections to adjust for it.
Proposal Number Seven: Buy-In Prices at Different Ages
If we aim for lifetime (or "whole life") health insurance, using a Health Savings Account, provision must be made for the vast majority of people who do not buy it with a single premium at birth, as we use for a simple example. If we know the lifetime goal and the expected average rate of return, it is easy to project the average growth of accounts by any future year. A simple table of such projections becomes useful for displaying the "buy-in" costs for any age. Naturally, it incidentally underlines how costs increase for late-comers since essentially the same costs are distributed among fewer remaining years. Conversely, compound investing while you are young is very attractive. These are important selling points and are valuable lessons to learn. But no strong argument is improved by exaggeration. This is not a way to reduce the cost of medical care, it is a way to pay for some unnecessarily added costs inherent in choosing a "pay as you go" design. The use of compound income does indeed give the initial appearance of something for nothing but should be viewed as a more efficient insurance design.
If it does nothing else, lifetime health insurance clarifies where this money is coming from. Under Medicare, for example, a person contributes all his life but gets no income on that contribution. At some advanced age, he spends that money at prices which reflect the Federal Reserve's 2% inflation of the money, but he pays no taxes on the gain. Meanwhile, some younger person pays his bills at the inflated rate, and in due course inflates it again before he spends it. In the case given, the last of three generations are spending money which includes eighty years of inflation at 1-2% tax-free. However, he has an opportunity cost: the money could have been invested in index funds which Ibbotson has shown would have grown at 12% per year over the same time period, tax-exempt if he put it in a Health Savings Account. And it wasn't even mostly his own money at work. It really doesn't sound impossible for that amount of compound earning to pay for a great deal if not all of the lifetime cost of one person's healthcare, providing he does not pay excessive investment costs to do it. And since this conclusion is based on considerations which have almost nothing to do with the cost of medical care or increasing longevity, it is nevertheless impossible to make precise predictions. Any investment outside the insurance plan will result in a considerable revenue gain, probably a big gain, and possibly pay for all medical costs. Fundamentally, this money is generated by obtaining a higher return on the money, and not sharing much of it with financial agents, or other contestants for your wealth, like the health industry, or like the luxury goods industries. In that sense, it's just like any other wealth.
It also should not matter much whether the planning design aims for the account to terminate at death or when Medicare takes over. Naturally, the same lesson applies to the terminal end as to the buy-in date; the more you delay withdrawals, the more time there is for growth of the principal. With a growing tendency for costs to cluster around the last year of life, many "young old" retirees have only minimal medical expenses for ten or more years after retirement. Since invested money at 7% will double in ten years, there would be a considerable advantage for latecomers in transition. If the latecomer intends to terminate deposits at an attained age of 65, he will need about $40,000 to see him out. If he intends to terminate at death, he will need about $300,000, but the buy-in price at any age before 65 should be the same. As experience gathers, there probably will emerge some distinctions matching health status changes, but curiously the costs seem to decline after age 85. After the preliminary layering by age, the annual lump sum can be broken into installments more realistically matching the income and health practicalities of individuals. Each annual step of a table would represent the "buy-in" price at that age, which is also the average account size achieved by a lump-sum at birth by that age, without withdrawals. The point about "without withdrawals" should be seriously considered as a reason to substitute out-of-pocket payments for trivial expenses. With the passage of time, it can be made more precise by experience. But it should be kept in mind that a regular HSA only hopes to make as much income as possible, while a lifetime HSA seeks an average lifetime target. As experience accumulates, it may be found that required balances actually shrink with advancing age, as the individual lives past the time when expenses had been expected but not experienced. However, without experience, the best conservative assumption is that expenses steadily rise with age.
Since a Health Savings Account tries to serve several purposes, a particular account may not have enough deposit content to match the deductible, for example, because the cost of an individual's illness has little to do with his investment history. The manager of an account will create rules designed to protect his own position, and for example might have a minimum designed for investment purposes, which happens to be considerably short of what the high-deductible insurance company needs as a deductible for a particular age-group's sickness experience. For another example, a gift from a grandparent at birth may be adequate to cover lifetime expenses, but not at first. Only after it has multiplied several times will it be enough to meet the deductible. Some managers impose fees on the first $10,000 of deposits rather than reject the account, and it really only becomes an attractive investment a decade or more later. At present, accounts have an annual limit of $3300 for deposits, so it takes three years to reach a suitable size, and perhaps ten years if only a single deposit is made. Investors must learn to be highly resistant to brokerage fees, especially in new accounts. True, the regulations are likely to be highly changeable in the first few years, so investors much learn to pay fees from outside sources, in order to protect the tax advantage when it is most needed. Unfortunately, educating young investors about complex new regulations can be expensive for the investment advisor, so it is, unfortunately, true that the interests of broker and client are not well aligned in the early years.
The rules should be adjusted to recognize this problem, even though many people would find it unnecessary. A subscriber may have enough savings to make a single-payment deposit but is hampered by the $3300 rule. Finally, an account might once be large enough to be self-sustaining, but be reduced below that level by one or two depletions to pay deductibles. Generally speaking, the conventional HSA does not need to concern itself with such issues, which only become a serious problem if lifetime Health Savings plans are contemplated.
Consequently, the regulations should be modified in the following ways:
1. A family of tables is prepared, showing the deposit required to equal the total average future health cost for each yearly age cohort of life, from now until the average death expectancy, using various extrapolation assumptions. It is possible to reach the same goal with almost any investment assumption, or almost any time period, or almost any starting deposit, but only so long as the other variables are adjusted to conform to that specification. A family of tables would show several investment levels of compound interest reaching the same goal, let us say $40,000 at age 65, at ten percent; seven percent; and five percent. Obviously, a higher interest rate gets you to the goal sooner. Attention should be focused on achieving $40,000 at age 64.Any subscriber should be allowed to buy into the lifetime Health Savings Account for a one-time deposit of $30,000 at age 48 assuming 5% return, at age 55 assuming 7%, or at age 57 assuming 10%, merely as a rough example. The subscriber may not have savings of that size, of course, and a separate calculation should be made for time payments, also reaching the same goal. If such tables are displayed on a computer terminal, it should not be difficult to make a selection, but "user friendliness" is often more difficult to achieve. As are later modifications, if life circumstances change. The relentless mathematics will soon demonstrate that the more money deposited, and the earlier it appears, the more attractive the investment becomes.
2. Salesmen for HSA should be required to carry their illustrations out to the goal of $40,000 at age 64, supplying achievement benchmarks along the way. So long as the account contains less than the buy-in amount for the subscriber's age, the manager of a fund should be allowed to wager a guaranteed band of investment results; let us use an example of 7% and 10%. If the funds make more than 10%, the manager keeps the excess. If the fund achieves less than 7%, the manager must make up the difference, either by reinsurance or by offering to be at risk for it. If fund results fall between 7 and 10%, the investor retains it all. This mandatory arrangement may (not must) terminate when the fund reaches a buy-in level, so long as it resumes if illness depletes the account.
The actual limits should be set after consultation with managers in active practice since the purpose is to create incentives to get the funds to self-sustaining levels without kickbacks to investment vehicles. The tension is between a subscriber who has investment choices to make, and a fund manager who must cover his expenses. In the long run, it is to everyone's advantage to maintain a steady view of the risks and rewards of income compounding, while serving the goal of paying as much as possible toward everyone's health care costs in a free-market system. It is best if the limits are realistic, and they should be chosen to drive all the participants toward the highest safe level of performance. Ultimately, the subscriber should recognize that an unsafely high level (with leverage, for example) will make paying his health bills more difficult, not easier.
3. The easiest definition of the top limit is the running cumulative average of the stock market, so total-market index fund results are ideal for the purpose. However, index funds differ in their results, so transparent competition should even be able to squeeze out somewhat better results than the 10% compounding which has characterized the past 90 years. Curiously results significantly worse than the market is not a sign of safety. Consequently, freedom to change managers should be as unhampered as possible, comparative results and costs widely available, and exit fees discouraged.
4. In general, single premium policies are rarely used. However, since starting an HSA at birth adds 26 years to the compounding, and while the amounts at first are so small they are somewhat unattractive to HSA managers, they could nevertheless become an important feature of their future. Throughout childhood, the paradox will be common that the necessary deposits in an account for lifetime coverage of health costs are nevertheless far too small for a deductible which is sensible for children with such low health expenses. Therefore, provision should be made for supplemental policies which cover this gap in childhood between the amount in the account and the amount of the deductible, which is often set with an eye to the parents' situation, not the child's. Intuitively, such insurance supplements ought to be quite cheap.
Proposed: A Republican and/or Conservative Healthcare Solution
Foreward: Written as Obamacare is beginning implementation amidst considerable resistance, the following paper offers an alternative proposal which is perhaps no less sweeping, but includes much more reform of the existing system than does Obamacare, and much more emphasis on the use of competition and individual responsibility. It is divided into three sections, I: Correcting Non-Cost Issues, II: Correcting the Cost Problem, III: Forestalling Unfortunate Side-Effects.
I: Correcting Non-Cost Issues
The Uninsured. Gail Wilensky, who once ran Medicare, recently commented about Obamacare, "It isn't reforming at all, it is merely coverage extension." Unfortunately, even though it seems to promise universal coverage by mandating it, the GAO estimates that over thirty million people will remain uninsured after Obamacare is fully implemented. Indeed, it is very difficult to see how to include illegal aliens (11 million), the mentally retarded or impaired (8 million), and those in jail (7 million) within one big program which adjusts to the situation of the rest of the American community. The proposal here is to revise downward the idea of universal coverage, to whatever extent the usual form of health insurance is unsuitable for these three (and possibly other) groups. Their special health needs are not easily adaptable to conventional health insurance and would be better served by specialized healthcare programs, structured with their particular problems at the center of the design.
Pre-existing Conditions The American public has become convinced that sick people have only two choices, Mandatory Insurance with compulsory community rates (i.e. Obamacare), or go without insurance. As a matter of fact, every textbook of insurance will list at least three ways of coping with "impaired risks." The industry terms are "Assigned-risk Pools", and Joint Underwriting Associations (JUA). One highly successful model exists for fire insurance, called the Fair Plan. A new insurance company was formed by selling stock to existing fire insurers, which sells fire insurance at standard rates, but only to someone who has been rejected by an ordinary fire insurance company. This form of impaired risk management was the preferred vehicle of the Pennsylvania fire insurance industry because the stock ownership enables the owners to take a tax reduction for losses. Somewhat to their surprise, the Fair Plan proved to be counter-cyclic in a cyclic industry, and actually produced a profit (for the insurance company owners) during economic downturns. An additional source of revenue was provided when other states than Pennsylvania requested to be included. Fire insurance is not the same as health insurance, but they are similar enough to appear workable for managing bad risks with a medical Fair Plan, which deserves at least a pilot study.
Under Obamacare, the problem of pre-existing conditions is solved by individual subsidies, an endless prospect, and by forcing those who do not want insurance to pay the bill for it. The main resistance to a JUA will probably be found among dominant health insurance companies, who have enjoyed near-monopoly status for many decades. Sharing risk is unattractive to them: when there is hardly anyone to share it with, and while historical "sweetheart" arrangements still remain ensconced. To the extent that a JUA would force readjustments, Ms. Wilensky would certainly not lack topics for revision.
Income Tax Reform. Representatives of large major corporations have twice disrupted Federal health proposals at the last moment, after a long period of lobbying as a supposed friend of reform. To that extent, they are friends of conservative forces in medical care. Nevertheless, it is now well past time to demand that their income tax preference devised by Henry Kaiser during World War II be eliminated. The employer gets a tax deduction, and their labor force escapes federal taxation for the gift of health insurance outside the pay packet. Meanwhile, the self-insured and uninsured are asked to pay for health insurance with after-tax income. In summary, the favored arrangements of their insurers with hospitals lead to a preposterous result (which would continue under Obamacare) that the people least able to afford high costs are the ones required to subsidize the people with the best jobs. This situation has three possible solutions: eliminate the tax preference of employed persons, or give the same to the rest of the country. Since there is little likelihood that this situation will be self - correcting, the obvious third choice is to cut the exemption in half and give the same to the rest of the population. No one needs to give Congress a lesson in such compromises, so obviously, progress will require a public uproar.
Interstate Health Insurance Competition The amateurish introduction of Obamacare's health insurance exchanges poisoned public opinion; it may now be even harder to address the political problem they tried to solve with computers. Tracing back to Constitutional restraints on Federal activities, health insurance has always been regulated by states. As a consequence of growing scope and complexity, many states had to choose between multiple small health insurance companies displaying vigorous competition, and a single large-but-effective monopoly in each state. To exaggerate, the result verged on fifty monopolies exhibiting monopolistic behavior.
Instead of devising a Constitutional work-around, Obamacare devised computer solutions to basically political difficulties, using computer subcontractors. It is possible some legislative designers understood the model of the New York Stock Exchange, which permits an interstate exchange to perform the single function of conducting competitive financial transactions between buyers and sellers of corporations which are themselves state regulated. They may have observed that computers superseded manual systems at the stock exchanges, so they took a short-cut. Integration would have required insurance experts and computer implementers to work together, preferably under one roof. A one-step version of this two-step idea might have transformed fifty local monopolies into a system of competitive interstate pricing. But this would have been and continues to be, a daunting time-consuming political process requiring very considerable negotiation with deep skepticism about advice from industry experts with axes to grind. As it now stands, any benefits will prove just as delayed by rushing computer solutions first, as by making the computer system the mathematical statement of a negotiated design. Indeed, negotiations among pseudo-cooperative partners commonly prove more filled with traps and smoke-screens when linked to other objectives, than if the exchange idea had been selected as the single, otherwise unencumbered, goal. It might have taken several election cycles, but the outcome would have been more acceptable.
II: Correcting the Cost Problem
Health Savings Accounts Unless Obamacare regulations somehow cripple the idea, there is nothing right now to keep anyone from starting a Health Savings Account and gather tax-sheltered income for the inevitable rainy day. Everyone should do so, regardless of any other insurance they may have, and right away.
However, Health Savings Accounts once assumed the need would terminate when the individual enrolled in Medicare. The turbulent arrival of Obamacare now raises concern that Medicare will be stripped in order to pay for Obamacare. Since the "single payer" system is the fall-back or possibly even the goal of Obamacare, its final goal is also redefined as lifetime coverage. Whatever the path, it becomes important to project what it might cost. The additional compound interest feature of Health Savings Accounts creates the possibility that HSA is the only approach which could succeed or at least be the first to reach achievability. The steady conquest of disease by Science, the steady increase in productivity by Commerce, the expiration of patent protection, and the relentless tendency of expensive illness to concentrate near the last year of life -- all suggest a feasible lifetime approach is likely within the next sixty years. The best path to feasibility is not speculative borrowing, but inducing the upper 50% of the population by income to overfund their HSAs, by allowing some acceptable ways to spend the unspent surplus. Over time, financial goals should become more precise, and deliberate surplus progressively lessened. As a matter of fact, considerably more than half the population could afford this approach right now, an extension to the rest of the population faces resistance which is more psychological than financial.
In the meantime, individuals need reinsurance. Competitive and political obstacles to high-deductible reinsurance are numerous, but almost all forms of traditional (formerly first-dollar) insurance are arriving at high deductibles by themselves. If that takes too long, individuals with funded HSAs are driven to become over-insured rather than re-insured, by distorting traditional insurance into reinsurance. That is a wasteful approach. Elimination of co-payments (and secondary or tertiary insurance to cover it) with no proven cost-restraining ability, would greatly accelerate the trend to high front-end deductibles, and that trend should be encouraged. Other foreseeable issues would be the sudden appearance of an expensive treatment which greatly prolongs life. Since everyone ultimately dies, this might transform a steady rise in lifetime health costs into two distinct bulges, which is more expensive than one bigger terminal bulge. At the present time, however, new cures for disease merely push back the inevitable average terminal care costs, to a later age. Another way for the future to confound predictions is for the cost of labor to rise more sharply than the Gross Domestic Product since medical care is labor intensive. Finally, life-sustaining organs could become enhanced more than life-enhancing organs, giving us an epidemic of blind people in wheelchairs in place of the charming wits and sages we imagine for our future. None of this is within the control of insurance reform, so we may just have to wait and see. Meanwhile, it would help a great deal for the information-gathering to begin steps toward the goal of continuous monitoring of costs, and projections of future moving cost trends. A universal HSA program will be slowed more because it is new, than because it is impossible.
The Health Savings Accounts uniquely provide a way to circumvent the problems created by "pay as you go," mainly making it possible to gather compound investment income on the unused premiums of young people, no matter how long it takes them to get sick and use the funds. Lifetime HSA also eliminates the issue of "pre-existing conditions", since all costs are calculated into the premiums; and thus it also eliminates gaming the system by those who delay the purchase of the insurance policy. These last two features of lifetime HSA require up-to-the-minute cost data, whereas the compound investment of idle premiums in an HSA terminating at age 65 probably does not. Either way, compound investment income is an intrinsic and unique feature, which has the great advantage of already having the sanction of law. Individually owned HSAs are portable, as employer-based insurance is not, and offer equal tax exemption.
Health Savings Accounts are disadvantaged by a general lack of discount arrangements with hospitals, long arranged for Blue Cross organizations and grudgingly given to newcomer competitors. HSAs lack a large sales force and are sometimes neglected by salesmen of high-deductible insurance, as well as exploited by debit card agencies with unnecessary fees, and investment advisors with excessive fees. All of these things are based on competitive resistance and are not inherent in the insurance plan. More effort should be made to ease them.
Compound Investment Income. Most people, strongly conditioned not to believe in any "free lunch", underestimate the power of compound interest, and fail to appreciate its tendency to accelerate over time. 2,4,8, 16, 32, 64, 128, 256, 512. The big gains are toward the end, while sickness costs get higher as we age; there's a fortunate match of timing. Luckily for illustration, money at 7% interest will double in ten years. Therefore, a dollar at birth is worth $512 at age 90. And it is slow to start; which means if you wait until your 40th birthday, it only costs $16 to catch up and have the same $512 by age 90. Another fact: the average healthcare cost of the last year of life is at present about $5000. That's less than most horror stories would have it, and this low average is explainable by the fact that many people just drop dead without any cost. Let's do some calculating.
Since current regulations permit a maximum $2500 contribution to an HSA, a deposit only once at birth and none subsequently, would find $1,250,000 in the account, surely enough to cover almost any health catastrophe. Depositing $2500 into the account every year from birth to death at age 90 would produce an unimaginably larger result, well beyond any reasonable expectation of average escalation of healthcare costs. Depositing nothing until age 40 and then depositing the $2500 would result in a death benefit at age 90 of only $80,000, but still 16 times the present average cost of the last year of life. Contributing a total of $2500 over twenty years would achieve the same result at twelve or fifteen dollars a year, but would actually encounter resistance from the investment people, who would object to handling such small amounts. But that's a welcome problem, indeed. If all you are worried about is the cost of the last year of life, get an HSA and stop worrying. Unfortunately, our government isn't investing at 7%, it is borrowing at 4%. That's the way we transform a $2500 deposit in an HSA into paying a bill that costs the government at least $10,000. The source of it: using the 1965 expedient of "pay as you go", which means today premiums immediately go to pay for the debts of the past, leaving nothing to invest. And with a retiring baby boom larger than the working generation, the government borrows from foreigners to make up the shortfall.
What's To Be Done With This? Simply paying for the last year of life is as simple as buying insurance to pay for your coffin. We can surely do better than that, but first, we need a transfer vehicle. The fact that Medicare is paying for just about everyone's death means we can transfer the money to Medicare to reimburse them for what they have already paid. They can accordingly reduce the payroll deductions and Medicare premiums by a comparable amount in advance, as an inducement for anyone who agrees and has enough money in his account. We can also use the "accordion" principle and pay for more years prior to death if there is money for it. Even using some of it to pay off the entitlement debt is better than not generating any income at all; only the Chinese benefit from the present approach. Don't forget that "the beneficiary" is really a constant stream of successive people. Although one is now dead, his successor is alive and will do other things once the government threatens to take some away.
It is tempting to consider whether lifetime healthcare costs could be covered by an extension of this idea. Not only present costs are incompletely available, but future costs and future investment returns are not predictable by anyone. The best that can be done is to overfund at first, extend in a deliberate manner, providing bailout avenues for both subscriber and government, and provide incentives to compensate for the overfunding. Seven percent projected income is perhaps generous and tax-sheltered, but still, must contemplate the possibility of a great deal of inflation in after-tax dollars. If it should not, more money will have to be deposited, and the subscribers must agree to that. Against that unpleasant eventuality, it should be a voluntary program, and thus slow to expand.
But therefore it must have enough reserves from the start, with latitude to use the surplus for non-medical purposes once the medical purpose is served. Perhaps something like the Federal Reserve should be considered to protect and regulate it -- public, but reasonably independent within a narrow mission mandate. The pressures to move authority entirely into the public sector, or into the private sector, should be somehow balanced to prevent either one from prevailing. At some times, the deductible will have to be shifted up or down, to keep it midway between the bulk of either outpatient or inpatient costs. Contributions will eventually have to be raised and lowered within broad bands. Alternatives will have to be found for approaches which are new or become obsolete. It is very clear that two insurance systems will have to run concurrently, one to invest and store the money, the other to pay the bills. They will need an umpire, especially if they are successful.
A Note About Investment Vehicles. In speaking of people of all ages and conditions, it must be assumed they are inexperienced, naive investors; some will chafe at this, emphasizing it is their money to do with as they please. There should be some appeal mechanism for this sort of person, but the best defense is good investment performance. Although Index Funds are relatively new, an equity index fund of U.S. stocks above a certain size should be both politically safest and reasonably profitable. The managers should have a certain discretion to use U.S. Treasury bonds, but nothing else without a formal appeal process. In view of the gigantic size, perhaps a few other options might be considered for those who demand them. The administrative costs of such a large fund should be quite low. The management should be aware that the investment advisory industry may not be completely pleased with this arrangement, so the opinion of experts should be treated carefully. The purpose of this fund is not to innovate financially, it is to pay medical bills efficiently, and with the minimum of public uproar.
III: Forestalling Unfortunate Side-Effects.
In the meantime, the Diagnosis-based payment system -- and the reaction of the hospitals to it -- has introduced a new dynamic. It usefully illustrates how far-reaching the unintended consequence of even a small reform can go, before it is even recognized as causing it.
Diagnosis-Related Groups (DRG) To change the subject, a budget reconciliation bill two decades ago slipped in a feature of paying hospitals one of two or three hundred flat rates (there are actually over a million possible diagnoses) for the whole hospitalization. It did not matter how long the patient remained in the hospital, nor how many tests or treatments he underwent -- same flat rate. In spite of efforts to look for "Episodes of Care", ambulatory medical care is not nearly so amenable to this rationing device. As a consequence, hospitals average a 2% profit on inpatient beds, 15% profit on accident rooms, and 30% profit on satellite clinics. Since most dual-use items have the same basic cost whether used for inpatients or outpatients, escalation of outpatient prices results in carrying some pretty fanciful prices over to itemized inpatients, for those items not covered by insurance.
The basic issue is severing connections between costs and prices, and exploiting the public's trust that some connection remains. This situation caused a notable surgeon to exclaim that the "only purpose of having health insurance is to keep the hospital from fleecing you." It is not clear to what extent discounts from inflated prices are used as a competitive weapon in the outpatient area, but the tightly controlled and overpriced ambulance arena suggests that practices bordering on antitrust violations may well exist in some regions. There seems to be the considerable exploration of the legal limits of the present system; medical school tuition is largely set by what the market will bear, and surpluses soon have a way of seeping out of the hospital system into the university's general finances. Colleges without medical schools are upset by this unequal financing mechanism. It is not clear how far this complexity is extending, but such unexplained disruption is bound to cause many eventual problems, return to cost-based pricing is an urgent need. The first step might be to require public disclosure of price/cost ratios in more relevant detail. To abandon cost-based pricing always invites governmental price controls.
Interest Rates, Investment Income, and Inflation When there is inflation, the value of money goes down, so you might expect interest rates -- the rental cost of money -- to go down, too. However, people anticipate higher prices, so lenders build a premium into the interest rate structure to compensate for the value of the money to be lower when it is repaid. That raises interest rates, and the Federal Reserve will generally raise them even higher to put a stop to inflation. So, buying and selling bonds is a zero-sum game, far riskier than it sounds. Consequently, there is a flight toward the common stock, thus raising its price. Meanwhile, inflation usually hurts business, tending to lower the stock prices. As a consequence of all these moving parts, long-term investors are urged to buy at a "fair" price and never sell, no matter what. Even that strategy fails for any given stock because somehow corporations seldom thrive for more than seventy-five years. So, the advice is to diversify into a basket of stocks, and the cheapest way to get that basket is to buy an index fund. In a sense, you can forget about the stock market and let someone else manage the index, for about 7 "basis points", that is, seven-hundredths of a percent. All of this explains the choice suggested for Health Savings Accounts of buying total market index funds. Limiting the universe to American stocks is based on a political hunch that it reduces the chances of harmful Congressional protectionism. Having said that, a Health Savings Account must raise cash from time to time, and to guard against forced selling in a down market, some average amount of U.S. Treasury bonds will have to be maintained. Ideally, the number of Treasuries would be small for young people, and grow as they get older, and therefore more likely to get sick. Pregnancy is the one universal cost risk for younger people, and they know better than anyone what the chances of that would be in their own case.
This approach is greatly strengthened by reference to the modern theory of a "natural" interest rate, to which the whole system has a tendency to revert, if only we knew what the natural rate is. It is not entirely constant, but over time it seems to be something like 2%. If we knew for certain what it was, we could set a goal for perpetuities like the Health Savings Account to be "2% plus inflation". Since inflation is targeted by the Federal Reserve as 2%, that would amount to an investment goal of 4%. If you can buy an American total market index fund consistently gaining at 4.007 % per year, you should buy and hold. If it rains less than that, it is either run by incompetents, or it is a bargain which will eventually revert to 4.007% and pay a bonus. If, on the other hand, it gains more than that, there exists a risk it will revert to the mean. That it is being run by a genius is sales hype to be ignored. We suggest buying into it in twenty yearly installments, which should balance out the ups and downs, so then you can forget about even this issue.
But don't count the same issue twice. In order to assure a 2% real return, it is necessary to obtain 4% in the real world of 2% inflation, and the compounded income of 4% accounts for both in equal measure. A compound income of 6%, however, is two-thirds inflation / one third "real", so artificially raising interest rates to control inflation can progressively overstate the requirement, and hence overdo the deflationary intent. Conversely, when the Federal Reserve fails to raise interest rates as Mr. Greenspan did, the result can be an inflationary bubble. The central flaw in adjusting prevailing rates to current natural rates is that we do not know precisely what the natural rate is. To go a step further for immediate purposes, we are also uncertain how much deviation there is between medical inflation and general inflation. As a result, the best we can expect is to make as much income on the deposits as we safely can, and continuously monitor whether the premium contributions to Health Savings Accounts might need to be adjusted. And the safest way to do that is to have two insurance systems side-by-side, one of them a pay-as-you-go conventional policy for basic needs during the working years, and a second one whose entire purpose is to over-fund the heavy expenses at the end of life and the retirement years, permitting any surpluses to be spent for non-medical purposes. With luck, the beneficiary might retain a choice between increased premiums, and increased (or decreased) benefits.
If these calculations are even approximately close, the financial savings would be several percents of GDP, a windfall so large that mid-course adjustments could be tolerated.
Competition With Hospitals, Not Necessarily Between Them It is comparatively effective for small hospitals to compete with each other, but as transportation improved they grew bigger and greatly expanded their market areas. At that point, they share with big banks the awkwardness of being too big to be permitted to fail. Exploiting this, they have more freedom to raise prices. As they become more efficient, the size which matters is their capacity to support a geographically wider community. It is mostly transportation feasibility which matters, so breaking up ambulance monopolies may hold part of the solution. Satellite clinics have many advantages, but price control is not one of them.
The institutions which suggest themselves as possible hospital competitors are Retirement Communities (CCRC). Because land is cheaper, they tend to be built in the suburban and exurban rings around cities, but the elderly population is growing. Severe illness and disability tend to increase with advancing age, so they suggest themselves as concentration points for all medical care in their region. Almost all of them have infirmaries, many of them have rehabilitation and assisted care capacity. It would seem that what they mostly need is inexpensive ambulance service and a relaxation of regulations which inhibit overlap with lower-level hospital facilities. And, let it be emphasized, an extension of health insurance coverage to allow them to be reimbursed. If general practitioners and pediatricians began to locate offices on the grounds of a retirement community, specialists would soon follow, along with laboratory collection stations and x-rays. Over time, they could be expected to transport surgical patients to distant hospitals, and return them to the local infirmary for convalescence. Some would acquire hospital satellite clinics, but there are too many of them for a single type of development. It is vastly preferable for them to have unlimited hospital connections and unlimited access to their facilities. Their great contribution is potentially to compete with hospitals for certain services, which would be greatly inhibited by single limited franchise affiliations. If competition is encouraged at this level, it could make the usual sort of governmental wage and price control much less necessary. The fear of abusive pricing is one of the major inhibitors of generous health insurance, and it is in the long term self-interest of all health care providers to resist it.
Stepping out of the Obamacare Frame
The most painful criticism of Obamacare, is it wastes so much opportunity to make important reforms -- and still doesn't make them. Gail Wilensky, who spent two years running Medicare and Medicaid, spending decades struggling with a reform of the healthcare system, recently deplored the program's inconsequential goals, if coverage extension is all there is to it. More likely there was to be more, but events overtook the project. Seemingly, the President underestimated the difficulties and overestimated his advisors. Under the circumstances, the natural thing would be, back off in the face of many other demands on his attention, hoping there would be time left in his presidency to recover. The longer he delays, the less chance this strategy will have.
Most of the things which are seriously wrong had been wrong for decades. Using insurance for small healthcare claims is too expensive, merely making administrative costs compulsory and universal for no purpose other than tax avoidance. The only insurance against large and infrequent medical expenses has some modest place we might retain and repair while betting on science to reduce sickness costs. Rather than play historian trying to explain the whole situation, let me devote this chapter to a handful of illustrative changes which might make a big difference, even if only a few prove spectacularly successful. That is, we should taste them to see if they work, not bully ahead and swallow a whole banquet. Listen to the famous warnings of Galen and Hippocrates: primum non-nocere . At least, don't make matters worse.
1. TAX EQUITY. I wish I could name a solitary blunder we could fix or a solitary villain we could hang, to watch everything get better. Our general problem has many contributing problems at its source, At the top of the list, It's a toss-up between a handful of insurance practices begun seventy years ago, and the World War II expedient which we will call the Henry Kaiser tax exemption. I'm sorry, but "job lock" is advantageous to employers, who should not be expected to give it up without a reason. Small businesses are small, but in the aggregate are still important competitors. The fairness argument is meaningless in a competitive environment; large employers must be given something in return for a concession. It is only necessary to review the many regulations which favor small businesses over large ones, to see that large employers feel abused that government's thumb is on the scale. The way to eliminate job lock is to be found in bargains struck in this other environment, where there are more opportunities to balance unfairness arguments. The difference in costs is 15-30%, and it's big enough to warp the system toward certain types of insurance. It's certainly big enough to induce almost anyone to take it when offered. In summary, the designers of the Affordable Care Act seem to have underestimated the value of the Henry Kaiser Law to large employers, and therefore have not made a high enough offer to induce large employers to give it up. Since that would create a tax cost for the government, the rate should be reduced by about a quarter and extended to everyone.
 If Congress simply must micro-manage -- 
|
| A few tips |
The importance of preserving the tax inequity in the eyes of big business has been under-estimated. However, the importance of eliminating it has also been underestimated by reformers. All tax exemptions stimulate overuse because they amount to a discount. Federal tax exemptions now mainly extend to two consumer purchases: health insurance and home mortgages-- and both of them are destabilized by it. We currently have a national crisis in both at the same time. The tax-subsidized home-mortgage housing bubble preceded the financial panic, and tax-subsidized health care has led health costs into a second unsupportable bubble. Considered on the level of economics, giving a tax advantage to one group but not to its competitors requires a truly substantial justification because it can distort whole industries. The point here is that you can't eliminate it until you give it to everyone, because only then will the lobbyists go away.
Giving a tax subsidy to employees but not to self-employed or unemployed persons created the uniquely American system of employer-based health insurance, and now largely perpetuates the rather odd fringe-benefit system. Many employers wish they could find a way out of it. Emphasizing the important but temporary origins of this tax quirk in the California war industries merely dramatizes its lack of justification for seventy years afterward. Since the tax preference has been sustained almost exclusively by lobbying, it even calls into question the sustainability of our form of government. It should not be necessary to describe collateral damage like job lock and internal hospital cost shifting. The issue of equal justice alone should be enough to justify the abolition of this unfairness. To go still further down this path, mandating individual coverage to large populations while also excluding some of them from tax exemption because of the nature of their current employers, is to invite a Supreme Court case. And since mandatory coverage has been passed, the sooner a case is granted certiorari , the better.
2. REVISIT THE INSURANCE INNOVATIONS OF THE 1930-40s:
INDIVIDUAL OWNERSHIP OF HEALTH INSURANCE POLICIES is really another way of saying eliminate employer ownership because somebody must be the owner. Aside from the person covered or the person paying the bill, there are no other obvious choices. The only conceivable alternative is government ownership. Because the present participants fear that particular outcome more than almost anything else, a major source of resistance to change is the lack of clarity about what would replace employer ownership. And the longer the Obama administration fails to adopt reassuring measures, the more they are suspected of having that motive. Determined opposition originates in the current owners of "self-insured" groups, the employers, or the unions who have acquired this function from employers. Since most such arrangements are de facto "administrative services only", insurer protests of higher administrative costs for individual ownership are often just relics of ancient combat between Blue Cross and commercial insurers.3. ADDRESS QUIRKS AND ABUSES WHICH DISTORT PUBLIC MANAGEMENT OF HEALTHCARE:Regardless of the internal structuring of incentives, healthcare reform cannot be permanently settled without individual ownership. It must be understood, however, that eliminating the tax preference could be resisted at first by patients who acquire it, because of fear the tax would in some way be shifted to them, too, rather than eliminated. That need not be true if consideration is given to the relative size of the losers and gainers. Since the membership of group policies greatly outnumber individual policyholders, the revenue cost of tax equity -- after redistribution -- would be considerably smaller than 50/50, and likely be in the range of 75/25.
PRE-EMPT STATE LAWS WHICH INHIBIT CATASTROPHIC COVERAGE. State mandated benefits now impact high-deductible insurance in many states, and are the main reason Health Savings Accounts have been slow to spread. The provisions of ERISA shield employer-based health insurance from the unfortunate health coverage mandates in question. ERISA could not have been successful without this pre-emption, so unions and management unite in absolute concern to isolate ERISA from congressional meddling, although for different reasons.
REVISIT McCarran FERGUSON ACT. This act effectively makes the "business" of insurance the only major industry restricted to the state rather than federal control. It should be amended to permit the sale and portability of health insurance policies across state borders, thus greatly increasing competition and reducing prices. Once more, present law discriminates in favor of the employees of interstate corporations, who are also exempted by ERISA.
RESTORE ORIGINAL FORM OF PROFESSIONAL STANDARDS REVIEW ORGANIZATIONS (PSRO). These physician organizations effectively regulated many issues which are now the subject of a complaint. They were lobbied into ineffectiveness in 1980, and together with "Maricopa", essentially turned medical oversight over to insurance companies who thus receive no physician advice except their own employees.
LEGISLATE OVER-RIDE OF 1982 MARICOPA CASE. This unfortunate U.S.Supreme Court 4-3 decision was never tried and upholds only a motion of summary judgment about a per se violation. It prohibits physician groups from agreeing on lower prices and has been taken to mean physicians are excluded from exercising control of HMOs and Managed Care. It also perpetuates the notion of individual competitors in a profession which is rapidly acquiring larger groupings as units of competition. By some quirk, the full tape recording of the 1982 U.S. Supreme Court arguments can be heard on the Internet. It is above this author's pay grade to know whether it would be better to ask the Supreme Court to review its earlier decision, or to make legislative changes in the antitrust law which would somehow result in a better outcome.
The Supreme Court Needs Help, Too
WIDESPREAD INTERFERENCE WITH MARKET PRICING. Of equal or greater importance, is the package of expedients introduced by the Blue Plans in the 1920s and refined up through 1950. They include first-dollar coverage (the Henry Kaiser tax subsidy may share equal blame), service benefits, internal hospital cost shifting, hidden discounts to favored insurance companies, and the "pay-as-you-go" system. A more recent addition has been the DRG system of inpatient reimbursement, a brilliant idea poorly implemented, leading to total confusion in hospital inpatient and outpatient pricing. All of these subjects have been discussed at length in this book, and will not be repeated here.
SUBJECT MEDICARE TO MORE UNDERSTANDABLE AND CONVENTIONAL ACCOUNTING. The present special accounting of transfers by an agency of government, escapes being treated as debt would be treated in the private sector, and actually treats interdepartmental debts as assets. Medicare is now the largest debtor in the world, rapidly becoming more indebted, and hardly anyone realizes it is 50% subsidized. The implicit need to extend this subsidy to the rest of health insurance makes "Single payer" wholly impractical, however attractive it is to get a dollar for fifty cents. The public is largely unaware that Medicare is 50% supported by tax infusions from the general fund, not to mention the tax deduction employers take on the payroll deductions supporting Medicare. The change sounds like an inconsequential technical one, but merging the debts of Medicare and Medicaid would be considerably eased by this improved transparency, as just one example of where the special accounting leads us. Uncoupling the debts of Social Security from those of the 1965 amendments would be another example, but in the reverse direction because of the accounting razzle-dazzle. Until the CMS reports make this subsidy more apparent, the public is not participating in the debate.
No surgeon can pay malpractice premiums out of Medicaid reimbursement.
Now hear this. TORT REFORM. Malpractice costs mainly affect surgeons and obstetricians, who sometimes pay annual malpractice premiums of $200,000. Not only does this provoke defensive medical behavior, but it also provokes local physician shortages which in turn lead to hospital cost-shifting and other responses. The only tort reform which has proven value is to place a limit on awards for "pain and suffering", the traditional catch-all cost expander. Resistance to a cap on pain and suffering might be softened somewhat by allowing the greater of $250,000 or 10% of the total award. It is entirely unreasonable for pain and suffering to be worth about seven times the medical or "economic" damages, as is currently standard in the malpractice insurance industry. There may be other approaches to curing the malpractice problem, but many have been tried, and the medical profession believes this is the only one with proven success. It is very clear that the public does not understand how small a proportion of a typical malpractice award relates to the injury, and how much it relates to appeals to jury sympathy.
 Treat liabilities like debts. And transfers from the general fund as liabilities. 
|
| Accounting, for Congressmen |
PARITY BETWEEN INPATIENT AND OUTPATIENT CHARGES. As a general principle, when a service, device or drug is used in both the inpatient area and the outpatient one has its price exposed to regular market forces in the outpatient arena, the same price should be applied to it in the inpatient arena, plus a (separately negotiated) inpatient overhead adjuster reimbursement which generally applies to inpatients, and a second adjuster for the emergency room. There will be some services which are totally unique to inpatients or emergency room, which will have to be treated as outliers. In this way, a mutually reinforcing restraint is placed on such dual-use items -- with the market holding down outpatient costs, and the DRG ultimately holding down inpatient/emergency costs including outliers. As a general rule, the overhead cost-multiple established for dual-use should apply to the single-use items of either in-patient or out-patient. The key to all of these balancing limits is to permit open competition between hospital emergency services and private competitors, and an absolute prohibition of linkages between providers and emergency vehicle operators. After a brief trial, all such price constraints should be exposed to re-negotiation with an eye toward establishing transparent regional norms. MANDATE DISPLAY OF DIRECT COST MULTIPLES NEXT TO PRICES (FEDERAL PROGRAMS ONLY) (whenever prices are displayed, as in bills, price lists, etc.) FOR ITEMS COVERED BY HEALTH INSURANCE. Some high mark-ups are justified, but the public has a right to criticize them. This would not prohibit, but would considerably hamper, cost-shifting. It should be presented to provider groups as forestalling the prohibition of cost-shifting because of abuse. For this and other reasons, it would enhance provider competition. REIMBURSE HOSPITALS ONLY ON RECEIPT OF ASSURED POST-DISCHARGE HANDOVER OF MEDICAL RESPONSIBILITY (FEDERAL PROGRAMS ONLY). Unfortunately, hospitals do need increased incentive to improve communication after discharge, which now increasingly occurs on a Saturday. Payment by diagnosis, otherwise a good idea, results in sequestration of medical charts in the accounting department. Similarly, REIMBURSE HOSPITALS FOR LAB WORK ON THE LAST DAY OF HOSPITALIZATION ONLY AFTER DEMONSTRATION OF REPORTING. Such lab work, frequently obtained within hours of discharge, is sometimes overlooked and may even be unobtainable for the previously mentioned reasons, which in this case also apply to the hospital's own physicians. ENCOURAGE THE ESTABLISHMENT OF REGIONAL BACKUPS FOR AMBULANCES DRAWN OUT OF AREA. At present, ambulances are limited to going to the nearest hospital, rather than to the hospital of patient preference. The main justification for such behavior is the possibility that a second call might come while the ambulance was in a distant area. Fire departments have long solved this problem by shifting reserve vehicles into an overstrained area, to cover that area while the home vehicle is temporarily unavailable. In some areas, a reserve vehicle backup might require additional ambulances, but mostly it requires a mobile phone network. In areas of extreme distances between ambulances, the main need would be to relax regulations which exclude volunteer vehicles from serving that function. In densely settled urban areas, we now have the preposterous situation of mothers in active labor being stranded at the wrong hospital, only a few blocks away from their obstetrician. When such situations are repeatedly encountered, the current IRS exemption from financial reporting should be rescinded from the ambulance sponsor.Pharmaceuticals:The Coonskin Hat
CONVENE A TWO-YEAR BLUE RIBBON COMMISSION REPORT ON MODIFICATION OF THE PURE FOOD AND DRUG ACT.The issue is this: The original Pure Food and Drug Act only required proof of safety before a drug could be sold. The Kefauver, or efficacy, a requirement was added in 1962, triggered by the Thalidomide tragedy which has no real bearing on the matter. A manufacturer is required to demonstrate the efficacy of a drug for some condition, in addition to safety alone, before he can sell it. The cost of new drug introductions has markedly increased by billions of dollars for double-blind studies, and inevitably consumer price rises must make up for it. A number of benefits of this efficacy requirement have been demonstrated, including a reduction of patent remedies with uncertain value, and increased public confidence in their healthcare. To a certain degree, the FDA has supplanted the role of the medical profession in creating dependence on evidence-based prescribing, approved by the FDA rather than by professional circles, and that malpractice claims are part of the hazard. It is true that proof of important efficacy can justify the use of drugs which otherwise have recognized dangers. Disruption of corporate balance, favoring larger corporations, can be surmised. Therefore while it is not obvious that the Kefauver Amendment should be abolished, it is likely that important financial savings might be expected from modification of its cost impositions.
Senator Estes Kefauver of Tennessee, who ran for President wearing a coonskin hat, left a legacy of high pharmaceutical costs according to his opponents, but among his supporters, he wears the halo of defeating deceptive practices. It is reported that in Kefauver's time the idea floated around, that the Food and Drug Administration should mandate a program of tests to prove that all of these new drugs were good for something, not just that they were safe to take. Otherwise, it was thought, a great many innocent citizens would be induced by advertising to take worthless patent remedies. For many decades, the American Medical Association had denounced something it called "Quackery", which sort of sounded as though they had the same idea. Homeopathy, which at that time competed fiercely with the AMA, repeatedly thundered however it was better to take useless pills than use those dangerous remedies like bleeding and purging. To impartial observers, it sounded as though these two medical competitors were attacking each other in code. The Latin phrase, Primum non nocere ("At least, do no harm.") resurfaced in common parlance. Kefauver was running for President, he seemed to have an issue, and the Kefauver Amendment passed into law.
Let's have a look at the implications. The Pure Food and Drug Act had quite sensibly demanded proof that a new remedy was harmless, or at least harmless in the doses usually employed; otherwise, the drug could not be legally sold or advertised. A new drug had to be safe. However, many chemicals are useful in small doses but entirely poisonous in large amounts, so it might seem reasonable to qualify approval by outlining the circumstances of safe use. However, the Kefauver Amendment seems to be more directed toward a quackery danger, where the public interest is more the protection of the public purse. In any event, the specifics of the law promote civil servants into scientific umpires without a major focus on their scientific qualifications. The Kefauver Amendment provided that an acceptable drug had to be proven scientifically efficacious, as well as safe. So the burden of proof was on the drug manufacturer whereas evaluating that proof shifted to the civil servants instead of resting on professional consensus. With billions at stake, the manufacturer had both an incentive to find new cures, and a further incentive to find evidence of efficacy. Concealment of evidence was a constant possibility, so the civil servants became wary and increasingly conservative. As judged by the outcome, pre-release testing was required to be increasingly expensive.
Somehow the incentives got twisted, in what started as a benevolent effort to protect the public. The thalidomide disaster is credited with imposing useful conservatism on decisions. But two decades later, thalidomide is proving useful for many otherwise hopeless cases of cancer. Could this doubly unfortunate experience have been improved, somewhat? Thalidomide is not good to give to pregnant women, that's pretty clear. But does that mean nothing should be marketed until it is tested on pregnant women? Maybe it does, but that was a very expensive decision to make. And it should not be made by trial lawyers or fear of trial lawyers.
There are many such quantities about the amendment, and it is time to review the experience. Maybe this is the best we can do, but I doubt it. The nation needs to impanel a group of experts, give them two years, and ask what they conclude.
---------------------------------------------------------------------------------Antibiotics were bursting on the public news at this time, so it was clear a drug might be efficacious for many conditions. Was it to be required that a new drug must be proven efficacious for all those conditions before it could be sold at all? The result of this quandary was that a new drug must be proven to be efficacious for at least one condition. It didn't take long for the industry to figure out what to do about this ruling; just spend the money to prove that the drug was efficacious for the easiest condition imaginable, one that had a dozen existing remedies that were as good as or better for the condition. That would satisfy efficacy, at a perhaps considerably lesser cost than for the usage that was really planned.
Or the opposite situation, illustrated by aspirin. Aspirin had been used for a century for headaches, when the astonishing discovery was made that half an aspirin daily would reduce the incidence of strokes and heart attacks, by at least half. Was the law to be revised, to take account of the second condition without disturbing the first one? If Congress wants to muck around in this huge area, they had better enlarge the Washington offices of Congressmen hugely, just to keep all the archives of pharmacology, in several languages, going back at least a century. The situation cries out for delegation of the decisions to more specifically trained experts, except for fear that someone will inevitably die of a mistake, and the trial lawyers who are abundant in Washington will sue, and somebody will lose his seat in Congress; can't allow that to happen.
Meanwhile, the clinical trials industry has flourished. It happens that I was one of the twenty or so founding attendees of the Association of Clinical Trials, which now attend concurrent meetings in hotels around the world with thousands in attendance. The meetings are filled with speakers bearing slides, boasting to each other of experimental groups in the thousands, and grant money in the millions. The amount of money spent on this sort of rote research is simply unimaginable. No doubt, useful scientific knowledge surfaces as a result of this effort. Somebody needs to compile the amount of waste which is created when some vice-president up the line, decides to abort the research because its potential profitability has been calculated to be low.
And where does that leave the doctor? He has spent years studying the disease, and the chemicals, and the risks. Is he to be deprived of having a conference with the patient and/or family, explaining the risks and what he considers to be the chances of the patient for a cure? Perhaps the family doctor, depicted in the painting as pondering the chances of the little boy on an ironing board, does not have the necessary experience. But surely the super-specialist, sitting by his computer in a sixty-story office building, can be trusted to take now-or-never chances with his willing patient. Because the chance to cure the patient may only come around once, and someone has to be empowered to assume the risk of being wrong. The trial bar probably is sincere in protesting they have no reluctance to see a better appeals system evolve, or a better system of best-efforts experimentation. But it will take a long time to repair the existing damage; the trial lawyer knows very well what the doctor probably thinks of him, based on a long experience of his own or his trusted colleague's stories to the effect that, well, you can't trust any of them.
Let's repeat what has just been said. Safety is not the present issue; it is to be assumed the Food and Drug Administration has approved the evidence that the drug is safe to use, submitted the evidence to a panel of experts, and has received an opinion that the drug is safe. Let us also assume that the doctor has a hunch or some happenstance experience that it might be good for some condition, and wants to try it. Does this warrant the requirement that, before the doctor may use the drug, millions or even billions of dollars must be spent on research showing that the drug is good for something or other, not necessarily the intended usage?
In the early days of this legislation, a reassuring paragraph was put on the leading page of the Physician's Desk Reference, still given free to every physician:
Once a product has been approved for marketing, a physician may choose to prescribe it for uses or in treatment regimens or patient populations that are not included in the approved labeling.However, these reassuring words are preceded by language wrapped around an entirely different threat:The FDA regards the words "same in language and emphasis" as requiring VERBATIM use of the approved labeling providing such information."They Don't Make That, Anymore"
They Don't Make That, Anymore These words from the nice young lady in the drug store, left me astonished, baffled, bewildered, and angry.
Although I am retired from the practice of medicine, my limited license permits me to prescribe ethical drugs for myself. I had not realized, until that very moment, that to some extent it also isolated me from the experiences of my fellow patients. Let me explain.
The drug involved was tetracycline, which I had surely prescribed a thousand times, and to which I had a sort of loyalty growing out of the fact that I took it myself. In the days when I was a college student, I came down with a form of pneumonia that involved a lot of coughing, like whooping cough. It was then called virus pneumonia because it was somewhat different from ordinary pneumonia, even though it was called Primary Atypical Pneumonia in polite academic circles. Eventually, we learned that its cause was neither a virus nor a bacterium, but rather something in between in size, called Mycoplasma. All of this is important to know, because it tends to appear as a question on a certification examination, but the fact of the matter is, it was a disease for which there was no effective treatment. We could cheer up a little to know that of four hundred recruits at an Alabama training center who came down with it, only one died. On the other hand, Legionnaire's Disease is also caused by a Clamydia and lots of them died, probably because most of them were older. But no matter, in 1944 there was no treatment, and I can tell you it is very unpleasant for a very long time, no matter how young you are.

CAT Scan In 1950 I got it again, but this time I was a doctor and knew there was a good treatment. It sounds strange to say so, but I was sort of happy to be able to try out the new medicine, which was then called Aureomycin because the powder was golden yellow. Aureomycin was a trading name, with a patent, and when the patent expired the generic form was called Tetracycline. It worked just fine, and in three or four days I was out of the hospital, perhaps a little weak and shaken, but cured. Incidentally, I discovered an interesting feature of the disease which I believe has not been previously reported. It had long been observed that the chest x-ray showed pneumonia while the stethoscope perceived very little abnormality, a feature which disconcerted those of us who were concerned with the cost of medical care, particularly members of a generation who felt sniffy about the dependence younger physicians displayed for x-rays, and nowadays for CAT scans and MRIs. Unfortunately, in this particular instance, x-rays are clearly superior to stethoscopes.
My third time around for "viral" pneumonia was a few years later; I was sitting on a park bench near the hospital when I recognized the old symptoms were coming back again, so I went straight to the x-ray department and had a chest x-ray less than an hour after the symptoms appeared. I planned to have an x-ray to prove it, go get some tetracycline and be all better over the weekend, with a rollicking anecdote to tell doctor friends about. Unfortunately, the x-ray was normal, so I was admitted into the hospital to see what was wrong. The next morning the x-ray showed a densely consolidated lung, so it had been viral pneumonia all along. And so my old prejudices were vindicated; it was possible to be too quick to order x-rays after all. Unfortunately, the extra twelve hours without treatment allowed me to get a lot sicker than I had to be. I think I know this because, doggone it, I developed the same disease several decades later, took no shortcuts to the drug store, and was fine in a couple of days after I immediately started taking tetracycline. You could say this strange recurrence of Mycoplasma pneumonia over one-lifetime sort of illustrates how medical care of the disease has become progressively cheaper. Instead of a month in the hospital with no treatment, it was now a matter of skipping the stethoscope, skipping the x-ray, skipping the hospital, and just swallowing some cheap tetracycline capsules. You have to have the nerve to do it, of course, and ethically you probably only have a right to do it to yourself, knowing the risks and being willing to accept them. There is, however, one flaw in this story.
When Aureomycin first emerged from the clutches of the FDA (and well before that accursed Kefauver Amendment), it seemed astonishingly expensive. Because I knew what it weighed (250 milligrams per capsule), and I knew what gold cost ($35 an ounce), it was easy for an idle mind to calculate that Aureomycin cost more than gold. Gold now sells for $1700 per troy ounce, so you could take this story in the direction of inflation. I rather prefer to take it in the direction of nominal dollar amounts, because Aureomycin retailed for $5 a capsule the third time I had the disease, and $1 per capsule when it lost its patent and became tetracycline. The fourth time I had the disease, I bought a container of fifty capsules for 76 cents. But as you have already heard, by the fifth time I couldn't buy it for any price, because everybody had stopped making it. Since my view of the economics of useful commodities is that low prices will only cause shortages if there is artificial market interference, the usual cause of shortages is rationing. Somebody who understands the 2500 pages of Obamacare better than I do will have to tease out the way rationing has caused shortages of tetracycline. And when they are done confusing the public, let them explain why you also can't buy KMnO4 crystals (potassium permanganate), which has cured more cases of athlete's foot for twenty cents, than all those cans of stuff in spray canisters.
Competitive Institutions: Paying for Assisted Living
Around the turn of the 20th Century, it was the fashion to build specialty hospitals, devoted to a single disease like tuberculosis or polio, or one specialty like obstetrics or bones and joints. Eventually, it was realized that almost any disease is handled better if a full range of services is readily available to it. Around 1925, some inspired philanthropists made it possible to combine specialties within a medical center, and it is now generally agreed this is a better way when population density permits it. On the other hand, it is likely a source of price escalation. Time marches on, and the problems of excessive bigness are also beginning to predominate. The idea immediately occurs, to winnow out the routine cases which do not need so much technology, so that we can concentrate and devote high technology (and costs) to patients who will really benefit. And, immediately the perplexing outcry is heard that such rationalization is "cherry picking", which will soon bankrupt the finest institutions we can devise. The validity of such assertions needs to be examined impartially.At the same time, the horse and buggy era has been left behind, causing new separations along class lines, the flight to the suburbs, and the migration of philanthropy toward the exurban sprawl, as well as into urban centers. In all this commotion it was overlooked for a long time that medical care was not merely following the patients to new locations, it was becoming more of an outpatient occupation. Inpatient care was shrinking, and somehow expensive hospitals were swallowing their smaller (and less expensive) competitors. It wasn't a necessary development; Switzerland still favors small luxury "clinics" of ten or twenty beds, usually containing wealthy patients of a celebrity doctor. Local customs like this will change slowly. What America appears to need is more hospital competition and more ambulance competition; the two may actually be somewhat connected issues. For amusement, I once studied the patients in the Pennsylvania Hospital on July 4, 1776, when historical notables were congregating three blocks away. The diseases were remarkably similar to what is seen in hospitals today; problems with the legs, mental incapacity, major injuries, and terminal care. People are treated in hospitals because they can't care for themselves at home.
A BLUE-RIBBON COMMITTEE NEEDS TO STUDY INSTITUTIONAL COMPETITION IN HEALTHCARE.
This is a complicated issue and may take several years, or even several studies to sort out. What is useful for urban settings may be inappropriate in exurban ones; local preferences must be separated from special pleading, and that is not always easy. However, the continuing care center seems to be a permanent direction which is growing in popularity, as is also true of rehabilitation centers and retirement communities. Many of these institutions might incorporate doctors offices for their surrounding community, using the same parking facilities and many of the same medical specialties for both the neighborhood and the core facility. There seems no reason to oppose either rentals or private condominium-style ownership nor any reason to resist group clinics. Exclusive arrangements, however, are more questionable. All of these arrangements should be studied, and unexpected problems flushed out. No doubt the preliminary studies would lead to pilot and demonstration programs. And some practices which initially seem harmless, should in fact be prohibited. We have a lot to learn before we start overturning the existing order. But nevertheless, some arrangements will prove to be superior to others, almost all of them are regulated in some fashion, and the regulations should be examined, too. It should accelerate needed changes to know in advance which ones are ready to be tested, and tested before they are demanded.*******
.jpg)
CCRCs Everyone knows Americans are living thirty years longer because of improvements in health care, and some grumpy people are waiting with glee to see if Obamacare will put a stop to that sort of thing. It must be left to actuaries to tell us whether the nation saves money or not by delaying the inevitable costs of a terminal illness. But one consequence has already made its appearance: people are entering retirement villages in their eighties rather than their seventies. Presumably, people in their seventies are feeling too well to consider a CCRC, although other explanations are possible.
Accordingly, a great many CCRCs are seen to be building new wings dedicated to "assisted living". A cynic might surmise there must be some hidden insurance reimbursement advantages to doing so, but the CCRCs are surely responding to some kind of increased demand when they make multi-million dollar capital expenditures. Assisted living is a polite term for people with strokes or Alzheimers Disease, or some other condition making it hard to walk, or, as the grisly saying goes, perform the activities of daily living. One really elegant place in Delaware has suites with servants quarters, but for most people, the only affordable option is to be in a room designed around the idea of assisting an invalid. It's generally smaller and more austere but fitted out with railings and bars and special knobs. Meals generally have to be supplied by room service.
Not everyone is destined to have a protracted period of decline, but it's fairly frequent and universally feared, so it's a comfort to know your present residence is attached to a wing which provides for it. The question is how to pay for it. There are two main approaches currently in use, adapted to the limited financial resources of the aged and the particularities of CCRC arrangements.
In the first arrangement, there is no increased charge for moving to assisted living, which helps overcome resistance to going there. However, the monthly maintenance charge for others who remain behind in "ambulatory living" is increased, usually about 20%, to provide funding for those who eventually need special assistance. That's a financial pooling arrangement, sort of an insurance plan, and like all insurance, it has a tendency to increase usage unnecessarily. It also increases the cost to those who enter the CCRC at an earlier age, because they make more monthly payments before they use them. Although the monthly premium probably goes up as the costs rise with inflation, there may be some savings hidden in applying an earlier payment stream at a lower rate. That's called "present value" accounting, but like just about all accounting, its unspoken advantages and disadvantages contain a gamble on unknown future inflation.
In the other common financial arrangement, you pay as you go, when and only if you actually use the assisted living quarters. Because of the likely limit to resources, there is usually an attached agreement to garnishee the initial entrance deposit if available funds prove insufficient. The one thing which won't happen is being thrown out in the snow for non-payment; there's a law prohibiting that. Bigger apartments with large initial returnable deposits are of course better off paying list prices. Those with smaller apartments may have smaller deposits, and favor payment by a percent withdrawal. Some places haven't thought this through and offer no choice. In that case, more attention should be paid to those list prices and the percentage markup from audited cost. Better still is to have a free choice of both options, with cost transparency.
The remaining choice is between two CCRCs with differing options, made at the time you enter. The Obamacare fuss has made a lot of people acquainted with "adverse risk selection", which is largely based on the idea that an individual has a better idea of his health future than an institution does since that includes family history as well as earlier health experiences. But in general, a young healthy person is going to live longer without needing assisted living than an old geezer who going to need it pretty soon. A hidden adverse incentive is created for younger healthier people to set the choice aside, and come back in ten years, providing they remain alert to the underlying reason the monthly fee is then somewhat higher than in some competitive CCRC. At the far end of the age spectrum, an incentive is created to go into assisted living quarters a little earlier in life, generally regarded as an undesirable choice.
All this financial balancing act can seem pretty overwhelming to an elderly person who isn't entirely comfortable with the CCRC idea in the first place. Rest assured that everything has to be paid for somehow, and after you die you won't care what choice has been made. If you trust the institution to have your best interests in mind, the only consideration of real importance is whether your money will last you out. The institution cares about that even more than you do, so while they aren't likely to offer unrealistically bargain choices, they may offer a few which are too costly.
America has had a ninety-year romance with insurance because it is so comforting to be secure and oblivious to finances. This is just another example of the struggle between the search for a security, and the struggle to devise ways to pay for it. While no one can be positive about it, we're all in this together.
July 4, 1776: Patients in the Pennsylvania Hospital on Independence Day
According to the records of the Pennsylvania Hospital, the following 48 persons were patients in the hospital on July 4, 1776:
Richard Brinkinshire (Admitted 11/15/1775) John Ridgeway (Admitted 12/26/1775) James Chartier (Admitted 1/6/1776) patient (Admitted 1/6/1776) patient (Admitted 1/20/1776) patient (Admitted 1/20/1776) Mary Yell (Admitted 2/7/1776l) John Beckworth (Admitted 2/7/1776) Bart. McCarty (Admitted 2/10/1776) John King (Admitted 2/10/1776) Robert Alden (Admitted 2/17/1776) William Patterson (Admitted 3/6/1776) Elizabeth Hanna (Admitted 3/9/1776) John McMahon (Admitted 3/13/1776) Mary Burgess (Admitted 3/23/1776) Mary Anderson (Admitted 4/10/1776) John Hatfield (Admitted 4/15/1776) Eliza Haighn (Admitted 4/17/1776) Charles Whitford (Admitted 4/24/1776) patient (Admitted 5/8/1776) Susanna Carrington (Admitted 5/8/1776) patient (Admitted 5/8/1776) William Johnson (Admitted 5/13/1776) Lazarus Chesterfield (Admitted 5/22/1776) Mary Spieckel (Admitted 5/22/1776l) William Edwards (Admitted 5/22/1776) patient (Admitted 5/23/1776, Lunatic) Jane White (Admitted 5/25/1776) Charles McGillop (Admitted 5/29/1776) ---Fitzgerald (Admitted 6/1/1776) Michael Rowe (Admitted 6/6/1776) patient (Admitted 6/6/1776) John Hughes (Admitted 6/12/1776) Joseph Smith (Admitted 6/15/1776) Esther Munro Lunda (Admitted 6/15/1776) Mathew Coope (Admitted 6/19/1776) Anne Patterson (Admitted 6/19/1776) Thomas Savoury (Admitted 6/20/1776) Rebecca Winter (Admitted 6/26/1776) Elizabeth Manning (Admitted 6/26/1776) Negro (Admitted 6/24/1776) Elex. Scanvay (Admitted 6/24/1776) Fanny Stewart (Admitted 6/24/1776) Peter Barber (Admitted 6/29/1776) Catherine Campbell (Admitted 6/29/1776) Ann McGlauklin (Admitted 7/3/1776) Elizabeth Lindsay (Admitted 7/3/1776) Ann Jones (Admitted 7/3/1776)
The records indicate the following diseases were the reason for admission of those patients. Although in Colonial times there was no medical delicacy to avoid offending readers, present privacy standards require that we strip the diagnoses from the name of the patient and list them independently. There is some overlap, sometimes making it difficult to judge which disorder caused the admission.
- Sore, poisoned or ulcerated legs: 16 cases
- Lunacy, mind or head disorders: 10 cases
- Syphilis: 7 cases
- Fever and Rheumatic fever: 7 cases
- Dropsy: 5 cases
- Gunshot: 4 cases
- Diabetes: 1
- Blindness with clear pupil: 1
- Spitting blood: 1 case
- Dislocated arm: 1 case
- Inflammation of face: 1 case
- Scurvy: 1 case
- broken arm: 1 case
The following physicians were elected at the Managers Meeting dated 5/13/1776:
- Dr. Thomas Bond
- Dr. Thomas Cadwalader
- Dr. John Redman
- Dr. William Shippen
- Dr. Adam Kuhn
- Dr. John Morgan
Obamacare And Its Repair, Executive Summary
For a while, there was a great air of mystery about why President Obama was in such a hurry to get his healthcare bill through the Democrat-dominated House of Representatives, after passage by a Democrat-majority Senate. There were to be no amendments, and in front of television several thousand pages were dumped on the desks of Congressmen with no amendments permitted, under orders to call a vote within a day. Just read Jacob Hacker's book The Road to Nowhere about the Clinton Plan for Health of ten years earlier, and since Hacker was a campaign advisor for Obama, make a strong guess that Obama was following the same plan -- but encountered a sudden twist. Everybody in the House and Senate had been encouraged to submit his best ideas, so inevitably the House and Senate versions differed so much they had to go to a House-Senate conference committee, also dominated by Democrats. As related by Hacker, the plan was for the President to appear before the conference committee, pick the cherries out of both puddings, and emerge with his health bill. The rest would be discarded as useful camouflage.
Unfortunately, the Senate bill passed but Senator Kennedy died, and to general amazement, a Republican Senator (Scott Brown) was elected to take his seat in Massachusetts. Senator Byrd of West Virginia died soon thereafter, and the ability of the Senate to defeat a filibuster was destroyed while the health bill was half-way through the plan. Since an amended bill would have to be resubmitted to the Senate, it would never pass. So an identical copy of the Senate bill was hammered through the House of Representatives, avoiding the need for a conference committee, and thus avoiding certain defeat in the Senate. So the Obama bill is really the Senate version, containing much baggage which was originally intended to be dropped. And failing to contain some nuggets which would have come from the House bill, which might have made the final product make more sense. Soon afterwards, the House of Representatives suddenly elected sixty-some Tea Party stalwarts, making it absolutely certain that Obama was just going to have to live with the 450 sections of the Senate bill, because these hootin', hollering Congressmen quite naturally supposed that their districts had sent them to Congress to defeat Obamacare, anyway they could. Rather than accept the voters' mandate that Obamacare just wouldn't do, an effort was made to portray the new Republican Congressmen as mindless obstructionists. Which is exactly what they thought the voters wanted them to be. When the Supreme Court then put its foot on the federal government telling the states to take the uninsured into Medicaid, this lesson in what the Tenth Amendment says, was soon followed by the utter failure of the computer programs for the Electronic Insurance Exchanges, and nobody could see what their health plan looked like (or cost), to say nothing of being unable to buy it if they wanted to. Although Section 1251 of the Affordable Care Act assures that everyone could keep his old plan if he preferred it, millions of letters were sent to subscribers who couldn't buy one of the new plans for computer reasons, that their old plans were canceled, while the President confused everybody by repeating the mantra that they could keep their old plans.
Quite soon, employers of more than fifty employees were given a two-year delay in mandated switch-over, echoing the experience which had caused the Clinton Health Plan to be withdrawn a decade earlier, and arousing the suspicion that Big Business was again going to pull out. Individuals were given no such reprieve and naturally were upset about it. Just about every newly offered plan contained a far larger deductible than most people had ever seen and a higher premium than they had ever paid. What made it affordable was the government subsidy, which the computer mess made it difficult to measure. Very few had read the 450 sections of the new law of the Land, and if they had, would have been highly disconcerted. Much of it was never intended to be enacted, but it was impossible to know which sections they were, and so it was not reassuring to be told that the President intended not to implement such unidentified sections. With our troops retreating in Afghanistan and Iraq, and both Syria and Russia conducting acts of war in defiance of us. And the economy still in a slump after five years of "recovery". And the Federal Reserve buying dud bonds by the trillions of dollars worth. And the rest of our allies in worse financial shape than we were -- incompetence was a word on every tongue, to defend against it by the Democrats, to denounce it by every Republican.
So that's where it stands, six months before the next election. In the meantime, I have been working on two projects for real reform of the healthcare system. The first is to improve on the Health Savings Accounts, which John McClaughry and I devised in 1980. The proposal is that since anyone and everyone can start an account, it is universal by definition, portable between jobs, tax-deductible for everyone, and running about 30% cheaper than conventional insurance. I am proposing to expand the program by making Flexible Spending Accounts convertible to it and permitting it to pay the premiums for the deductible catastrophic insurance which is a condition for buying it. Doing so would extend the income tax deduction which you get if your employer buys insurance for you, to everyone. But all of that is without mentioning the astonishing amounts of money that would accumulate from investing the HSA in low-cost index funds of premium American stocks. Nothing is guaranteed, but the experience of the last century is that this approach would assure enough internal income to pay for the entire lifetime healthcare cost of most people who bought it young enough. If you are sixty-four years old, you may have missed most of your chance, but younger people could have quite a windfall. The transition from here to there is pretty technical, and I hope I have not over-simplified it.
The second theme I have pursued is to start listing the many simplifications and cost savings for American healthcare, which I have assembled in sixty years of practicing medicine. What I am suggesting is what real healthcare reform would look like, not just coverage extension. The Congressional Budget Office predicts that spending a trillion dollars will still leave us 30 million uninsured people under the Affordable Care Act. Instead of that, I propose we develop three specialized (and probably non-insurance) programs for 8 million people in jail, 8 million mentally impaired, and twelve million illegal immigrants. Forget about mandatory; if you want to help thirty million people, devise three specialized programs aimed at these three groups, and you have it. Meanwhile, a whole group of flaws was introduced into American health insurance during the last Depression of the 1930s, and they should be repaired. It is preposterous to use three insurance plans to pay for a medical service (80% primary, 20% secondary, plus Major Medical for outliers). First dollar coverage was designed to exploit the Henry Kaiser income tax deduction, which should have been repealed decades ago. Co-pay of 20% has no effect on utilization, and 50% co-pay would infuriate people; co-pay should be abolished. Service benefits mean you never know what your bill is, and never know how much it is going to be; costs escalate. Payment by diagnosis means it doesn't matter how long you stay in the hospital, or how many tests you have, the hospital gets paid the same; consequently, it is essentially a rationing device for inpatients, making hospitals charge emergency room and outpatient services astronomical amounts. And the whole thing has transformed the purpose of health insurance. Nowadays, the real reason to have health insurance is to keep the hospital from fleecing you. Which they have to do, to remain solvent. The list goes on and on, to the point where you have to concede that you can only do so much in a short time. You just have to hold back to keep from overturning the system.
Psychiatry: Last Cow in Philadelphia
The present problem with PSYCHIATRY can be summarized as follows: At the suggestion of the American Hospital Association, Congress introduced the DRG system of paying for inpatients by diagnosis, rather than itemized services. It worked well except for psychiatry, where the diagnosis usually implies little relation to the later costs it generates, so an exception was made. The dual system of payment created loopholes which unfortunately overpaid psychiatric hospitals and were described as exploitation. Congress over-reacted in a way that was unsustainable, and essentially all of the psychiatric hospitals of the nation were forced to close. This is not a history for anyone to be proud of, and the lack of outcry is also a disappointment. However, after twenty years without reform, evidently, nothing is going to be done without an outcry.CONVENE BLUE RIBBON COMMISSION TO REPAIR PSYCHIATRIC INPATIENT CARE. The 1983 BRA switched hospital inpatient reimbursement to payment by diagnosis (DRG). Abuse of the psychiatric exclusion then led to "corrective" legislation which has essentially reduced American's psychiatric inpatient care to an underfunded national disappointment. The problem is not an easy one, so a commission should devise a workable methodology for psychiatric hospitals, relying neither on present approaches nor on DRG. But overpayment is a better outcome than no care at all. Homeless people sleeping in cardboard boxes on downtown steam grates are the consequence any visitor to the area can observe at night after the commuters go home. Psychiatric social workers readily recognize their daytime patients in the boxes.
* * * * *

Daniel Blain, M.D. Daniel Blain, M.D. (1898-1981) was just about the most important psychiatrist in America. He was the Physician in Chief of the Institute of the Pennsylvania Hospital at 49th and Market, the first and in many ways the most prestigious psychiatric hospital before it was closed. Before that, he was the first Medical Director of the American Psychiatric Association, itself the first (1844) medical society in America. His fame rested on organizing the disorganized psychiatry of the Veteran's Administration into a chain of advanced "Dean's Hospitals", a huge and very important achievement. Before that, he had achieved considerable fame as the man who took the dilapidated State Psychiatric Hospitals with a reputation as "snake pits" and made them a respectable part of the medical community. And before that, he had been born in China as the son of missionaries. As a matter of fact, even before that, he was a descendant of General Mercer of Revolutionary War fame.
Dan was an outstanding example of the peculiar fact that Psychiatry was dominated by social upper crust psychiatrists in Philadelphia for a very long time. In fact, Benjamin Rush of the 8th Street branch of the Pennsylvania Hospital is known in some circles as the "Father of Psychiatry", while in other circles he is known for signing the Declaration of Independence. That isn't true in other cities, and it definitely isn't true in New York City, where the psychoanalytic school of Sigmund Freud took that city by storm, and essentially drove every other school of psychiatric thought out of town, out of medical schools, out of psychiatric hospitals. The famous sixteen-year psychoanalysis of Woody Allen is an example of the extremes of that fad. Every profession has petty civil wars of that sort, best left undiscussed in public. But in the case of psychiatry, it was indirectly a material contributor to the present disappearance of inpatient psychiatry, and the related appearance of lots of homeless people on steam grates. Let me give a biased view of what is a massive human tragedy, which someone else can "rectify" if he chooses.
APA It starts with a Budget Reconciliation Act of the 1980s, which brought us the DRG (Diagnosis-related) system of paying for hospitalized patients. The idea was that appendicitis resulted in essentially 7 days in the hospital, give or take a couple of days, and the bills for admission for appendectomy were for more or less the same amount. If you had fifty or a hundred cases a year in your hospital, the high bills balanced the low bills, and the overall hospital reimbursement was essentially the same without itemizing the bandages and whatnot. Congress bought this package, and after it got going, just about all hospital bills were reimbursed at one of three hundred prices, the cost to the government was the same, and there was a whole lot less bookkeeping and accounting cost. It was a success, except for a few cases where the costs did not closely line up with the diagnosis, and psychiatric hospitals were where they concentrated. So, psychiatric hospitals were excluded, and psychiatric bills skyrocketed. This experience has been carelessly cited as an example of the evils of payment by service ("fee for service"), when in fact the duration of psychiatric hospitalization is related to features of the condition, like danger of suicide, rather than the diagnosis itself. Psychiatric leadership at the time contained many in a subset of physicians who did not think much of inpatient psychiatry in the first place and even less of lobbying, and they underestimated the severity of the assault on the specialty. Apparently, no workable formula for pricing inpatient psychiatry has since been brought forward to be approved by a Congress which is more accustomed to getting its lobbying in the form of one-liners. And would you believe it, psychiatric inpatient care soon disappeared.

Pennsylvania Hospital That's right, if someone in your family needs psychiatric hospitalization, I wouldn't know where to tell them to get it -- at any price. From considerably overpaying for psychiatry inpatients to paying scarcely anything for them, this little change of the regulations caused every psychiatric hospital I know of by name, to close. It helped balance some state budgets, but it also was a considerable factor in filling the steam grates of American cities with people who sleep on cardboard boxes. And what it illustrates is that this is what political society always seemed to do, before Dan Blain and a small group of upper-crust psychiatrists were temporarily able to shame them into something better. In fact, if there is any tattered remnant of good inpatient psychiatric care left in America today, it is in the Veterans Hospitals that Dan was able to straighten out.
Dan Blain will probably eventually be bypassed as a curiosity, like his wife. She was a Wister Logan Blain, descended from families who ruled Philadelphia a hundred years before even General Mercer came along. So the Blain couple lived on an enormous farm plot, centered at 20th and Olney right next to LaSalle University, which is built on their property. It also contains the Peale House, where Charles Willson Peale lived as the elected president of the rebel faction of the American Revolution. Peale didn't know what he was supposed to do, so he resigned and painted portraits of people. The Blains enjoyed keeping a cow on their land, the last cow in Philadelphia, and the LaSalle students enjoyed stealing the cow and leaving it on the top floor of a dormitory, for laughs. Meanwhile, the Blain couple had cocktail parties on their front porch for visiting dignitaries. They usually wore blue jeans, and Mrs. Blain, the absolute Queen of Philadelphia society, was occasionally observed to pour vodka into her glass of beer. That sort of background may well have been useful when psychiatry needed to be built up and humanized, but it became a liability when the rest of inpatient psychiatry failed to appreciate what was knocking on its door.
What's The Matter With a Partial Answer?
It has to be noticed that developing lifetime health insurance is hampered by the considerable pregnancy and newborn costs which intrude at the beginning of the earning period from ages eighteen to forty-five. Otherwise, there is a reasonably manageable medical cost at the end of life, potentially preceded by a long period of negligible medical costs where compounded interest could be at work. So the thought naturally arises we might somehow pay for pregnancies in some novel way, essentially borrowing those costs against the future. What's involved here?
Instead of taxing each affected individual working person to subsidize his newborns and terminal care, the necessary subsidy could take place between three insurance plans, assuming the three costs to fall in separate insurances. Everyone owes a debt for being born, and everyone needs to save enough for getting old and dying. Society's benefits and costs of having children are not confined to those who have children. An unhealthy incentive to delay the first child has been created by paying for pregnancies this way, spreading the consequences to higher education and disrupted careers. Instead of regarding neonatal care as an expense of pregnancy (which we currently regard as part of the mother's health cost), just reverse matters, and include pregnancy costs as part of the baby's own debt for being born. Any move assigning pregnancy costs must somewhat fudge the transition cost of getting born without paying for it or even asking for it. Attitudes depend to some degree on whether people generally want children to help on the farm, to help care for their own old age, as entertainment or plaything, or accidentally. The theoretical fact is that pregnancy costs might be judged fairly split between the child and his parents if it were only practical to do it. Once those practicalities are addressed by covering the first and last years of life with entitlement, transfers become relatively easy. If we must have entitlements, birth and death are certainly inescapable ones.
Unfortunately, once the finance is made practical, other issues assume greater importance. Science is beginning to make single parenthood more feasible, while easy divorce makes multiple parenthood possible. Easy sharing of the costs could reasonably be resisted as a moral issue we never had, and now don't need. The longer you live, the more interest you earn on those first 26 years. But the longer you live, the more medically expensive you become, toward the other end of life. There is still a great deal of argument about what is a fair division, and much time will elapse before final resolution can be considered a settled matter. But ultimately, serious savings could occur from keeping the first and last years of life in mind as the only universal medical costs, extracting maximum savings as one argument for choosing accounting tricks to settle the pregnancy part of it. What would be left would be accidents and occasional health calamities, which paradoxically are the only parts of current health insurance which truly fit the current insurance model.
Let's give an example. Lifetime health expenses are said to be somewhere around $300,000. If you have $40,000 in a Health Savings Account on attaining the age of 65, you can passively achieve $300,000 by age 86 (which we hope is at least average life expectancy) by letting the HSA grow untouched. In this example, all other sources of health insurance revenue are available for other purposes -- they are the "profit" from using compound interest, but it is unnecessary for that to be exclusively the case. Now, the problem transforms into achieving $40,000 by age 65. That could be reached by investing $150 at birth, or $2400 at age 26. Both are achievable, neither is easy.
But it's nice to have some choice, which including the first 26 years will give you. You can even do it twice, once in the child's account, and secondly in your own. My guess is that about a third of people could spare $40,000 at age 65 right now, trading a single payment for Medicare for its present wobbly finances. With overlapping populations, 2/3 of people could afford to spare $75 from each parent of a newborn, or $150 for a single parent, in return for eliminating the obstetrical premium within their health insurance. Considering the problems of young parents, some might prefer to combine $150 with $4800 for both parents at age 26 into a financing package of $4950 spread over ten years, from 26 to 36. But notice it gets harder, the longer you wait. Finding $80,000 for both parents now aged 65 gets really hard to do, but at least the child is all paid up. If you wait, it gets pretty hard to do this without extending the retirement age to 70, sacrificing five of your thirty years of retirement, but reducing the amount you need to save by about a sixth. Nothing like these choices would be readily accepted. But the policy axiom remains: the younger you start, the easier it is to stretch the distance. And the more attractive it becomes to treat some or all obstetrical costs as the responsibility of the person getting born.
Before concluding this approach is impossible, try to remember it is quite unnecessary to make lifelong healthcare free to the last penny, although some will demand it. In fact, first-dollar coverage (i.e. making all healthcare seem free) is a big part of what got us into this mess. If we only achieve a quarter or a third of this promise, the national aggregate would amount to a stupendous amount of money. A more realistic goal might be to reduce projected medical costs by a third, offset another third with investment income, and pay a third in cash. All three of those approaches seem comfortably achievable.
As this chapter is being written, Obamacare has been struggling for three years to achieve its twin goals of reducing the cost of medical care, while improving its quality and scope. The public has long been skeptical that the two goals are incompatible. During those three years, we have achieved a cure for Hepatitis C. That cure will save millions of lives and eventually the costs will decline. In time, the public will be able to see the difference between the results of the two approaches. During that time, biological science has discovered the relationship between sleep and the circulation of spinal fluid through the brain, probably the greatest advance in physiology since Harvey discovered the circulation of blood in 1628. In another field, Joachim Frank has identified the function of the Ribosome, making strips of protein the way a zipper works, and very likely the step at the beginning of cellular life, operating at room temperature and without caustic chemicals. These three discoveries are surely less than 1% of the scientific advances of the last three years, giving promise of vast advances in the cheap production of protein drug therapies, saving of lives, and ultimately the extension of life expectancy at a lessened cost. During these past three years, what has Obamacare accomplished, at enormous cost, and widespread turmoil in the medical system?
As we approach the elections which will serve as a national judgment on Obamacare, it still remains difficult to say what it is. It clearly will raise costs, not lower them. It will extend a few subsidies to people who were uninsured, but the subsidies could have been extended without so much uproar. In any event, a number of people will have worse insurance after the dust settles. A regulation factory has been established, pumping out confusion, but changing comparatively little after three years of trying. It begins to seem incredible that there is so little to show for so much uproar, and there is room to doubt anything dramatic will emerge so late in the process. If the goal is to establish a regulation factory to shift control to the regulators, the public is quite right to ask what good will come of that; at the present rate of revelation, the eventual product will just be an expensive nuisance. So it seems fair to compare the final product with the Veterans Administration health system, which has been operating on a large scale for more than fifty years.
The Veteran's Administration health system is in the news, finally. Perhaps we should examine what is the matter with the VA, as at least a source of ideas about the forces which hem in any government health system. For example, whether it is a municipal, state or federal hospital system, it seems to be much better at constructing new buildings than maintaining them. Perhaps it is time to convene a study or a series of studies to address this discrete issue. Why is the system of control by budget relatively successful in an environment of designing and building a project, and so unsuccessful in running it?
Second, is there an inherent problem in setting the rules by the Congress or Legislature, instead of an appointed board of overseers? No doubt, there is an occasional abuse of power by a trustee of any organization, but lower-level administrators do not act as though this a big problem for them in private institutions. So what is it about governance by politicians which encourages the endless intrusion of politicians into the admissions, purchasing methods, hiring and disciplining processes of public hospitals? Does it make a problem to have control at the highest level be unified in a Congress or City Council, or is it the other way around, with too little authority vested in the operating divisions? Every administrator complains about staff physicians intruding into daily operations, but is it possible that the public institutions have gone too far in hierarchy, or else possibly not far enough? Most physicians hate administrative work, allowing a few tyrants to emerge, who do like it. When these would-be dictators are in administration because they are poor physicians, trouble is almost inevitable, and it cannot be improved by giving the power to nurses, pharmacists or other professionals who are normally lower in the pecking order than the professionals who now report to them. There is no good substitute for physician control, but what if all the physicians in a health system would rather quit than do administrative work? Maybe, just maybe, the private sector has something to teach us in this delicate issue.
To go on, politics may play the same disruptive role as professionals harnessed as administrators. Administrators detect and quickly resent a Union or American Legion official placed in a role which can disrupt the official power structure, just as if a pharmacist were appointed, or a nurse practitioner, or even an eminent neurosurgeon.
Finally, some new title should be applied to the type of corruption which is seen when union officials get their way in disrupting the day to day business of a health system. Quite recently, I was forced to hear the Director of local city Veterans Affairs say to an open meeting of strangers that he was totally and permanently disabled with a service-connected disability, and also working full time for $50,000 a year. Furthermore, he had recently declined an offer to work at a higher government level, at $200,000 a year -- plus, of course, his 100% permanent disability payments. There is more than a small chance he was making some exaggerated boasts, but even so, it is appalling to hear such indiscrete remarks being offered, without the slightest sign that he recognized the revulsion such remarks made on his audience. It seemed obvious to all of us that he heard such remarks so constantly, that he regarded such politics (new word needed) as reflecting a normal, legal and desirable state of affairs. If Obamacare contemplates anything approaching what seems to be the normal attitudes prevailing in the VA, it really will not matter much what is written in its regulations. In defense of the VA, a more compassionate history may reveal a plausible explanation.
It is my view that Congress is more responsible than they themselves realize, and the problem is worse than we think. Things have been trending in the present direction for fifty years, but the adoption of the DRG system of hospital payments came along in the 1980s. It was a brilliant rationing system, but it did not work well in Psychiatry, where the diagnosis has little correspondence to the cost. After a few convulsive experiments, Psychiatric hospitals were offered a payment system so unsuitable they could not exist with it. One by one, inpatient psychiatry disappeared no matter what the patient's finances were, and there is really only the Veterans System left. The situation was so egregious that admission officers simply ignored any rules which prevented admission of a case which clearly needed it. The distinction between service-connected and non-service-connected was most readily shoved aside, since humanitarian and medical urgency so clearly over-rode the rules. After twenty years, the disregard for administrative admission rules spread out to almost every condition, and it is going to be very hard to put the genie back in the bottle, when so many involved participants never wanted such non-medical constraints, from the very beginning.
Building a network of modern buildings in every section of the country, running an organization dominated by unions and their counterpart the American Legion, within a system which most doctors in the country avoid if they can, the VA is a quiet disgrace, slouching along for half a century. The underfunding, the political favoritism, the squelching of pride and achievement and the waste, are all about what you would expect from a union-dominated or politically dominated system. But most disheartening is to watch reform efforts squelched. Under the leadership of Dr. Dan Blain, a system of Dean's Hospitals had been created to infuse the high standards of neighboring teaching hospitals into what seemed like systems similar toward medicine, reformed by the Flexner Report in 1914. For a few years, it seemed to be working, but in time the financial ethics of teaching hospitals seemed, not to raise the standards of the VA, but to be dragged toward imitating their behavior. The medical school doctors assigned to VA hospitals served out their time, then agitated to be transferred back to the teaching hospitals, with difficulties in replacing them with the same quality, slowing winning. When you begin to see elevator operators running the self-service elevators, you can be pretty sure the administrators have lost the battle. There are thank goodness, plenty of exceptions. But nobody seriously expects them to change things very much. If you like what you see at the VA, you are going to love Obamacare.
All Right, Hippocrates. So What's the Basic Problem?

Affordable Care Act It took me a chapter to describe what went wrong with the Affordable Care Act. Five chapters to describe what should be done about it, in whole or in part. But the best final goal of it all, one which has the best chance of making medical care affordable, can be described in a few words. Until we decide where we want to go, we are unlikely to go there. and I simply can't believe that modification of health insurance is worthy of all this uproar. Health insurance executives may be forgiven for thinking so, but it is hard to imagine the rest of the nation has such priorities. Without stopping to argue that unprovable point, I offer what I believe is a self-evident, and better, goal. One paragraph more of history is needed.
AMA Medical turmoil in its present form seems to have begun in the Progressive Era, sometimes called the Gilded Age, which briefly preceded and probably had something to do with, the First World War. It certainly involved President Teddy Roosevelt, who first proposed National Health Insurance, generating considerable appeal within the American Medical Association. After a brief flirtation, the Association then changed its position and has been more or less opposed ever since. At that time, the AMA turned its attention to the so-called Flexner Report of 1914, which advocated the physical and managerial relocation of medical education into the existing Universities. Out of this grew an unexpectedly vigorous medical research environment, responsible in time for the amazing transformation of medical care which characterized the 20th Century. This transformation which in turn probably generated the idea that Medical Schools were the natural center of the profession, a suggestion which greatly annoyed the AMA, triggering an unfortunate power struggle between medical school faculty and their practicing alumni. Since this battle divided those who were paid salaries from those whose income came from patient fees, parochial teaching issues were allowed to migrate into conflicts about how all doctors should be paid. From that the two groups soon split over the payment arrangements of health insurance, which also seeped out into questions of how all "health" care employees were to be paid, especially nurses, and thus who should manage them. In short, the subject material for a restructuring of medical payment wandered around for a century, getting further and further from resolution as new voices were heard, times changed, and the new arguments had little to do with the old ones. To summarize this century of argument in a few sentences leaves everyone confused about the topic, but certainly leaves no participant in a position to criticize the others. It is even possible to claim this bickering was good for the profession, because, for all the scolding, medical care has undeniably flourished in the meantime. I only picked up the trail, joining the profession during the Second World War. I was a practicing physician for fifteen years before Medicare made its appearance. My viewpoint may be narrow, but I have been at work in Medicine before, during, and after most of the major changes in the medical care of the last seventy years.
To come to the present concluding point, I believe the American medical system actually does have its own unique plan already for the future of health care. Never mind what the rest of the world does; they never had the resources to do what comes naturally to Americans. It goes like this: We resolved without saying so, to pour tons of money, in amounts the Europeans cannot even imagine, into a medical system populated by the best students we could identify. This somewhat pampered priesthood has one main mission: eliminate the disease, and thereby eliminate the cost of disease for everyone, rich or poor, the world over. Some physicians are more idealistic than others, and there is some grumbling. But scarcely anyone dares to challenge the results, summarized by thirty years of increased life expectancy achieved in a single century. Arithmetic alone makes it impossible to repeat that performance.
Sounds pretty grandiose, doesn't it? As to costs, how much do we spend, today, on polio, tuberculosis, rheumatic heart disease, and thirty other diseases I once spent my time with? And how little will we soon be spending on Hepatitis C and HIV? A lot, at first, but in ten years, probably very little. The great killers of my medical student days, like syphilis, subacute endocarditis, heart attacks, and strokes, are declining fast, so probably no more than a quarter of what they used to be. People have their gall bladders and appendices removed, but they don't even go to the operating room to do it. Improved longevity is taken for granted. Doesn't anyone want to live an extra thirty years? Doesn't everyone want his cataracts and knees replaced? The list goes on so long it is ineffective to recite it. We got our orders, and we delivered. No other nation on earth could even dream of such a project, and yet someone still occasionally challenges me with statistics about infant mortality in Luxembourg. Our inpatient psychiatry is a disgrace, yes I will give you that. But wipe out disease, that's the way to reduce health care costs for everyone. We're going to do it, and nobody else has a prayer of a chance. It is remarkable that costs keep rising while disease keeps disappearing, but even that trend must come to an end. Inevitably, there will be a reckoning of details.

NIH, Jim Shannon It's probably fair to ask who told us to do such a thing. Everybody did, and nobody did. As much as anybody, my contemporary at the NIH, Jim Shannon exemplified this dream of the conquest of disease, and was in a position to do something about it. Maybe it was Vannevar Bush, who was the same sort of scientific evangelist. But somehow that search doesn't feel like the right one. What feels right is that the generation of Americans who conquered the armies of the world just pushed us onward to conquer a little thing like a disease. American exceptionalism did it, and right or wrong is going to get it done. It's true that I worry we will keep people on thirty-year vacations, which our grandchildren will take at the beginning of life instead of the end of it. It begins to sound as though Reverend Malthus may have been right about feeding all these people, and maybe there will be problems with employment. But that isn't our mission. We feel the nation wanted very badly for us to do what we did, and they are just going to have to whip up a generation of environmentalists, or sociologists, or banjo players -- if there are to be new directives. Passerby, go tell the Spartans: We lie here, forever obedient to their laws.

Vannevar Bush Since I am about to launch, in closing, a proposal for revising the goals of American health care, it seems appropriate to begin it by recalling a remark of one of my medical school teachers, delivered at the close of the Second World War. "The goals for medical research,' said this pathologist, "are relatively small. When we've found a cure for cancer and arteriosclerosis, we're about done." Since the current generation of students would regard anything known before 1945 as not worth knowing, and the treatment of cancer has not advanced much since the time of this prophecy, we had best be modest about what we already know. It is widely stated that fifty percent of drugs currently in use, was totally unknown only seven years ago. That may well be true and may continue to be true for centuries to come. The limits of knowledge for medical students were once defined in a study by Howard Becker called Boys in White and go as follows: First-year medical students are determined to learn it all. By sophomore year they have decided you can't possibly learn it all, so you only try to learn what is important. By Junior year even that seems impossible to learn, so you only try to learn what is going to be on the tests. Essentially what this says is that the faculty finally gets control of things by Junior year, and their selectivity defines the horizons of what students pay any attention to.
This is a strangely limited selection of topics, which is finally set straight by the training directors of postgraduate Residency programs. Having played each of these roles in my time, I feel the residency directors have it about right, but only for inpatient care. Outpatient care is now the source of nearly half of hospital revenue, and the proportion is rapidly growing. The inpatient faculty reasserts control by writing the Board Examinations, and the final mixture is defined as the present state of medical knowledge, but it remains strangely neglectful of the outpatient half of medical care (notice, I did not say health care, which has become a rapidly growing world as non physicians assert control over funding sources).
But even an assessment based on all these biases may still not be a good measure of where Society stands in its search for scientific progress. For one thing, we haven't been serious about science for very long. The first course in science, of any sort in any American university, was only offered at the time of the Civil War. Although I had already decided to enter the Medical Profession by the Second World War (eighty years later), I nevertheless chose a college major more suitable for a gentleman. English literature, now that was the thing. In a few elite colleges, it still is. A bachelor in engineering is a degree for people who invent things; a bachelor in science was for those who would discover things. But a bachelor in the Arts was a degree for someone who planned to run things. Until that witticism loses its bite, we haven't really become serious about how much we can depend on the average patient knowing what he needs to know, to assume cost-effective control of his health. Young women and mothers chatter about pediatric topics quite a lot, but for the rest of the population, the state of medical information remains what the physician priesthood understands and has the time to communicate.
In 1945, the limits of medical knowledge were thus only two: how to cure cancer, and what to do about atherosclerosis. Today, we finally discover that sleep has a lot to do with the circulation of spinal fluid through the brain, which sounds about as advanced as Harvey's discovery of the circulation of blood in 1642. This year it became possible to see that protein synthesis is like a zipper in thousands of ribosome molecules inside zillions of cells inside you, me, Eucalyptus leaves, and dinosaur bones. Since cellular chemistry is pretty much protein chemistry, the potential for drug synthesis, to say nothing of understanding cell activities, is immense. I have had a reasonable acquaintance with a couple of dozen Nobel Prize winners, and mostly I don't know what they are talking about. The point is this: right now, it is practically impossible to know how much more there is to know, and therefore what discoveries are possible in the next twenty-five to fifty years. My pathology professor was obviously pitifully ignorant in 1945 about what lay ahead, and we haven't even cured cancer yet. How long it will take for a lot of billionaires to be created after they discovered a cure for something, isn't known and isn't knowable. But God bless them all, because the money they will save us in the cost of medical care, simply staggers the mind. Who will care about the cost of health insurance, when every disease the present generation of medical students will learn about, has disappeared? On the other hand, perhaps the scientific opportunities which are uncovered will trivialize the new pharmaceuticals of only seven years ago, which are half of the drugs presently in use. As long as the music keeps playing, we will have to keep dancing and hope for the best.
ACA Synopsis, July 4, 2014
The Affordable Care Act, commonly called Obamacare, contains two clashing provisions. Although the public may believe the Act provides for Universal Mandatory Health Insurance for all Americans, it actually only sets standards for minimum coverage. Because of later Supreme Court decision, the applicable section was renamed Section 5000A of. In the same section, it delays applying these standards to employees of big business and exempts about thirty million others entirely. (Section c). In an independent section of the same law, Section 1251 clearly states that people satisfied with existing coverage may keep it. Even after millions of Americans nevertheless received cancellation notices, President Obama repeated on television that no satisfied person would be required to drop existing coverage. Even disregarding mere verbal assurances, the two written sections did follow the rules for enactment and were signed by the President. just how are they simultaneously possible, to say nothing of workable?
A quick answer would be that the first sentence of the first Article of the Constitution vests sole power to create legislation in a Legislative Branch composed of a Senate and House of Representatives; thereby requiring the agreement of both, for a law to be a product of the entire Legislative Branch. It did not take long before a Conference Committee system was established, where the two Legislative Houses could negotiate any differences. When one party has voting control of both Houses, however, it is occasionally able to create identical language, eliminating the need for reconciliation. According to a book by an intimate, the Clinton administration planned to take this process a little further in their own Health Plan of 1992, including undesired provisions when that was useful to obtain a wavering vote, or otherwise to obscure the true direction of the legislation for extra time. Having complete control of the process, the party in power would later be able to delete undesirable provisions. The true nature of the legislation might thus only emerge at the last possible moment when timing could be manipulated to make it difficult to object. It is not possible to know whether this strategy has been used in other legislation, but circumstances strongly suggest it was partially implemented in both Clintoncare and Obamacare, and by many of the same people.
In any event, Clintoncare was withdrawn by its sponsors, before a floor vote, and for undisclosed reasons. Obamacare was enacted by the Senate, but the death of Senator Kennedy and his replacement by a Republican Scott Brown made it impossible to survive a filibuster on its return for final Senate adoption. To avoid this outcome, the Senate bill was forced through the House of Representative's word for word, and the Senate bill then became the final law, even though it was known to include booby traps. Largely as a result of public outrage, a strong Republican majority was returned to office, and the possibility of the further amendment was ended. So that's why we are essentially where we are.
What happens next is much more uncertain, because more actors have an opportunity to initiate events. Setting aside international adventures and financial crises, Congress could lose control of events by failing to negotiate a solution. After that, it is probably up to the electorate of seven states with tight Senate races, if not the United States Supreme Court, which has its own private agenda. All of these potentials put pressure on Congress and the President to negotiate a compromise. I suggest a simple first step would be to see if the entire section 1251 could become an amendment by addition to section 5000A, That would have the effect of adding a fourth class of exemption (people who don't want to change) to Illegal immigrants, incarcerated persons, and those with religious objections. Alternatively, they could be added to employees of big business as "temporarily" delayed. A case could be made to the Democrats that a smaller initial transition group could be more readily implemented. And a case to the Republicans would essentially be that "nothing is so permanent as the temporary". In both cases, the November Senate races would suggest what the public will support.
The public tends to believe the central agitating issue is health care, but more likely the central issue is state versus national regulation of health insurance. Health care was universally regarded as a local or state issue for three hundred years, and the issues were all technical and peaceful until pre-paid insurance began to be the dominant method of paying for it. No one seems to be noticing that ERISA has peacefully solved almost all of the problems of interstate mobility, which is what agitates interstate health insurance. Essentially, my position is that healthcare regulation can safely return to state control, at least during the period when the techniques and insights of ERISA are copied and experimented with, for health insurance. The public actually has very little interest in the interstate regulation of health insurance, so fifty years of agitation have essentially been over nothing.
With regard to health insurance, I believe we are working with the wrong design. Young working people accumulate savings, and old retired people spend it. Lengthened longevity has created the potential for enormous savings from compound investment income generated by working people, but such savings have been frittered away by using a "pay as you go" payment system. If we created portable systems for saving and investing income during the working years (the Health Savings Account), we could almost dispense with health insurance of the present model until people reach fifty or sixty years of age. Lifetime health insurance would be one approach, but all that is really necessary is lifetime savings accounts. Dispensing money from a fund could be quite adequately managed with a debit card, leaving only the problem of disciplining the fees of investment managers. But the details of such saving, investing and disbursing are of only secondary interest to the public, probably best left to the industry itself, because the industry will be very interested, indeed. As for reducing the cost of health care, we have stumbled along, letting the scientists eliminate disease costs by eliminating disease itself. They still have worms in Africa, and Asia could use some sanitation, But we have reached the point where our fastest-growing age group is over 100, and out biggest unsolved health problem is not dying too soon; it is living beyond our savings.
Changing Environment
My wife once remarked that having children was like making pancakes; just throw the first two away. But she only had four children, her grandmother had ten. Her daughters had two. Increased education makes childhood longer, while improved health lengthens retirement. The working period, age 25-65, however, has already extended its borders, pretty much to the limit. Ben Franklin's crusade to use healthcare to put sick people back to work, has been superseded for lack of orphans and invalids. In the past fifty years, miscarriage changed from passing nuisance into a devastating disaster because waiting to have the first child is largely an athletic event. In the future, population unbalancing will mostly depend on more retirees. There's a big economic effect. Neither children nor retirees earn very much, so the wealth of the country comes from ages 25-65, which must support everybody else. Countermovements seem remarkably feeble. The pressure to retire later in life is voiced but not much acted upon while starting work younger must contend with the publicity that more education increases lifetime income. It is too early to know how realistic it would be to shorten school vacations or to pack more education into shorter time at school, with electronic teaching.
In a simpler age, parents supported their children and their aging parents. It was unusual for women to earn very much, so marriage contracts enforced a support requirement. While the employment of women broadened the base of earnings, weakening the marriage institution threatened the retirement security of unmarried women. The political reaction to these changes has been a tendency to substitute government support and retirement programs for the family-based support system. Our national commitment to equal justice has had a tendency to make the new government system more expensive than the old family one. It once seemed just and natural for the wife of an impoverished man to be impoverished, but now the standard has moved to equality of treatment. In all classes of life, there is a tendency for discordance between males and females. The poor single woman gets more money, the poor single male probably gets less. The prosperous single woman gets less that she has been accustomed to, the prosperous single male is probably better off. It is too early to know how the new legislative climate will affect homosexuals. There is little doubt these changes will affect political attitudes of almost all demographic groups, but great uncertainty about the degree and direction.
Nothing makes it likely there can be much change in the dependence of the whole system on financial transfers from working groups to non-working ones. However, the system of collecting in the form of taxes and disbursing in the form of subsidies is both inefficient and disagreeable. A particularly inefficient way to accomplish this response to a weakened family structure is found in health insurance, now representing close to 18% of Gross Domestic Product (GDP). If we are to take money from younger people and transfer it to older ones, we should be collecting investment income on the decades-long interval. This is a continuous process, not a one-off transfer, and the amounts involved are seriously large. While the issue is the same for Social Security as it is for Medicare, it is easier to see how it came about in Medicare. In any new program, there is usually a transition problem to be financed, quite often by phasing it in. In the case of Medicare, the choice was made to facilitate passage of the legislation by employing "Pay as you go". In this system, the early recipients receive full benefits without paying anything toward them and are paid by the contributions of the new younger beneficiaries who will not need benefits for many decades. In other words, the system functions on the cash flow of the system instead of on funded reserves. Its great danger lies in the possibility that some generation (in this case the Baby Boomers) will eventually create a beneficiary class too large to be supported by smaller later generations. This pitfall has received much attention, but unfortunately, very little attention has been given to the problem mentioned earlier: no interest or investment income is derived from funded reserves, as is quite common in whole-life life insurance.
Nor should it happen, if the price to be paid is to have the Federal Government become the largest owner of common stock control of the private sector. That would be a very large step in the direction of government ownership of the means of production, otherwise known as Communism. With present artificially suppressed interest rates, the investment return available to governments is so small it could well be counter-productive. Borrowing from yourself is a useless exercise, and if confined to government bonds, puts the nation in a vulnerable position with potentially hostile foreign nations, or even supra-national organizations like the UN, who could one day have an agenda we consider hostile, under the control of a unicameral body dominated by one-state, one-vote system. No matter how it is arranged, it involves a loss of sovereignty for an unacceptably large part of our economy, eventually leading to a total loss of sovereignty. This transfer of funds from young to old must remain in private hands, with individual voters retaining control of it. Unfortunately, a great many intended beneficiaries are incapable of managing their own affairs, so there is a significant agency risk. That's a nice way of saying that a great many people have been cheated by friends and relatives they unwisely trusted, and there is every reason to look an offended politician straight in the eye and say, "I'm sorry, but I don't trust you." Unfortunately, this commonly results in the ones you can trust, charging an exorbitant fee for the simple role of being trustworthy. This is not a new problem. The only solution is to have at least two systems at the same time: a Prudential group of experts with themselves much to lose from being exposed as less than perfect, giving oversight to at least five competitive funds. How you chose the funds, and how you choose the expert overseers, are crucial.
Let's Annex Canada

President Donald Trump To read the newspapers, President Trump's revoking the Paris Climate Agreement is the biggest thing around. But it has no enforcement provisions, everything is voluntary, and its prospects of making the world colder are slim. The President is acting like a bull in the china shop, while the effectiveness of the document is questionable, indeed. The opposition party appears to have the motive of keeping him busy, so he won't have time to do anything substantial, and his motives are probably similar, except in reverse.
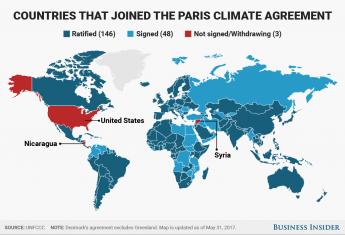
Paris Climate Agreement So I hereby propose a different global warming project, following the example of the cavemen. You will recall that during the last Ice Age, the cavemen didn't have a Treaty of Westphalia to worry about. So they adopted a different strategy: they migrated. Since 1648, we now have national boundaries to consider, so our way of creating room to move is to annex Canada. Those Americans who feel like getting colder would then merely have to go where it is cold. What would the Canadians think about that?
Louis-Joseph de Montcalm The French Canadians in Quebec might not like my proposal, since they have dark memories of Montcalm, or was his name Wolfe? But the oil-rich parts of Western Canada have oil which probably has some border tax they would like to be rid of. The Eastern part, the Maritime Provinces, petitioned America a few decades ago to annex them, so presumably, they would like to have some gerrymandering, or possibly fishing subsidies would suffice. At least half of the Canadian political class would oppose, but they would be neutralized by the other half who would be in favor. It sounds politically feasible.

Arctic melt The attraction would be that it's cold up there, although Toronto and Montreal went underground to keep warm. The Arctic ice pack is melting, and climate change people keep telling us about it, with photos, and the Russians are selling tickets for tourists on ice breakers. If there are any Tories still around, they would vote Republican, whereas the people in Saskatchewan would probably still vote for Socialized Medicine. The French? Well, they would probably have thirty parties and cancel each other. Certain parts of Canada are immersed in the Gulf Stream and are warmer than Boston. I understand some provinces don't have taxes, certainly suggesting a paradise. From what I hear of the behavior of Esquimaux women, there are attractions for men, and the male surplus would certainly attract some American girls.
So what are we waiting for? The Chinese or the Russians might get the same idea, and we could always sell it to them if we are disappointed.
Martin Feldstein Does It Again: Eliminate Tacit Tax Exemption for 70% of Workers Denied To the Rest
Headlines in the Wall Street Journal announced collapse of Congressional healthcare reform. In the same edition, a small short article buried in its depths described a possibly major step toward its reform. Martin Feldstein calmly observed, a tax exemption for healthcare insurance of 2.9% really amounts to a wage increase whose elimination might go a long way toward paying for the eighty-year mess Henry J. Kaiser had created. (In fact, it was effectively taxable income of 4%.)
It was all so simple: healthcare extended longevity, created thirty years of new retirement cost. In turn, exempting the premium for healthcare became a tax-exempt increase in wages -- for the 70% of employees getting insurance as a gift. Maybe not at first, but wages adjust to expect it during eighty years. Social Security could not cope with an extra thirty years, so SSA was going broke, while health insurance was actually the main cause of increased longevity.
But notice how unused Health Savings Accounts automatically turn into retirement accounts (IRAs) for Medicare recipients. So if you are lucky and prudent with healthcare, or if you overfund an HSA, unused healthcare money makes a reappearance in retirement funds where it belongs. If you have used up the money, you have probably been sick, and maybe won't need so much for a shortened retirement. Increasingly, expensive healthcare hits the elderly hardest, so there are many years during which compound interest overcomes inflation. At the rate things are going, retirement may become four times as expensive as Medicare, so let's consider that future.
Medicare doesn't save its withholdings, it uses "pay as you go" and spends the money on other things, like battleships. Therefore, to make any use of this windfall, it is necessary to save it, invest it, and use it for retirement. Just doing that much might redirect the other 30% of the withheld tax to its intended purpose. So the economic effect would be considerable, just by stirring around in that corner of it.
Posted by: G4 | Jun 30, 2012 12:38 PM I wonder if what is meant by the claim that the PPACA abolishes catastrophic heath insurance is the abolition of co-payments, co-insurance, and deductibles for benefits considered to be part of an "essential benefits package", which the HHS website defines as including the following:
- Ambulatory patient services
- Emergency services
- Hospitalization
- Maternity and newborn care
- Mental health and substance use disorder services, including behavioral health treatment
- Prescription drugs
- Rehabilitative and habilitative services and devices
- Laboratory services
- Preventive and wellness services and chronic disease management
- Pediatric services, including oral and vision care
Posted by: G4 | Jun 30, 2012 12:08 PM Sorry, the administrator remove the theme.
Posted by: netteplo | Aug 23, 2011 7:12 AM the 12 suggestions need to be reader accessible right where they are referred to in the last section --they are the red meat of the whole essay
Posted by: bzp | Oct 3, 2009 10:24 AM
49 Blogs
Table of Contents
Clintoncare and Obamacare: Historical Foreword

Picking Out the Raisins From the Pudding
 President Obama's present political pickle is a veritable textbook of the loopholes, traps, and flaws of our legislative system.
President Obama's present political pickle is a veritable textbook of the loopholes, traps, and flaws of our legislative system.
Welcome to Welfare
New blog 2014-06-24 18:42:35 description
Reforming Health Reform, New Jersey Style
 U.S. Representative Robert Andrews (D, NJ) had a night he won't soon forget on August 24, 2009. Facing 3000 constituents angry about Health Reform, he practically had a public stoning.
U.S. Representative Robert Andrews (D, NJ) had a night he won't soon forget on August 24, 2009. Facing 3000 constituents angry about Health Reform, he practically had a public stoning.
Children, Playing With Matches
 Is health insurance now mandatory?
Is health insurance now mandatory?
Text of AFFORDABLE CARE ACT, PL 111-148, March 23, 2010, Renamed HR 3590
Using a home computer, the full text of any section of the Affordable Care Act can be read in three steps: first, find its section number in the table of contents we provide in this blog. Second, call up the entire Act in any search engine's URL box: Third, enter this section number into the internal search box. (The internal search box is called up by pressing control and f simultaneously. On Apple computers, call up the internal search box by pressing command and f, instead of control and f). In either case, the search box should pop up, in the upper right-hand corner of the screen.
The Real Obamacare, Unveiled
 The method of Obamacare enactment made it hard to know what was enacted. The entirely unexpected bungle of insurance exchange introduction made the public ask pointed questions about big issues, without getting lost in little ones. Underpromise but overperform is certainly a forgotten guideline.
The method of Obamacare enactment made it hard to know what was enacted. The entirely unexpected bungle of insurance exchange introduction made the public ask pointed questions about big issues, without getting lost in little ones. Underpromise but overperform is certainly a forgotten guideline.
Text of Section 1501, renamed Section 5000A: MINIMUM COVERAGE
Section 1501 is generally described as mandating individual health care insurance for all Americans. It doesn't exactly say it that way, and sections (2), (3) and (4) list the main exceptions. Officially, it's an amendment to Subtitle D of the Internal Revenue Code of 1986.
Text of Section 1251 (H.R. 3590):PRESERVATION OF RIGHT TO MAINTAIN EXISTING COVERAGE
New blog 2014-02-25 22:39:59 description
Proposal: Coordinate Sections 1501 and 1251
New blog 2014-07-03 20:25:48 description
Health Care and Education Reconciliation Act of 2010
New blog 2014-07-09 20:12:33 description
State and Federal Powers: Historical Review
Obamacare's Constitutionality
 Obamacare's constitutionality was argued before the U.S. Supreme Court in late March, 2012.
Obamacare's constitutionality was argued before the U.S. Supreme Court in late March, 2012.
Roberts the Second
 Chief Justice John Roberts seems to be intent on radical changes to the Supreme Court, made in a conservative way.
Chief Justice John Roberts seems to be intent on radical changes to the Supreme Court, made in a conservative way.
More Work for the U.S. Supreme Court: Revisit Maricopa
 Once the Supreme Court acts, it is very difficult for anyone else to act.
Once the Supreme Court acts, it is very difficult for anyone else to act.
What Can Supreme Court(s) Do About Tort Reform?
 The Chief Justice is in charge of the Court System.
The Chief Justice is in charge of the Court System.
ERISA Is Thrust Into the Battle
 The 1963 bankruptcy of Studebaker led to The Employee Retirement Insurance Security Act of 1973. And last-minute amendments suddenly included health insurance for most big industries. The result is a significant conflict for Obamacare to resolve if it can.
The 1963 bankruptcy of Studebaker led to The Employee Retirement Insurance Security Act of 1973. And last-minute amendments suddenly included health insurance for most big industries. The result is a significant conflict for Obamacare to resolve if it can.
Money Bags
 When Medicare started it was chaos, worse confounded.
When Medicare started it was chaos, worse confounded.
Electronic Insurance Exchanges
The first real taste of what Obamacare was all about, came on October 1, 2013, when Electronic Exchanges were opened for the sale of competitive health insurance policies. In spite of warnings that the computer system had been inadequately tested, political considerations seemed to dictate that it was best to go ahead with the system, planning to fix any minor technical problems as the system unfolded. The problems were worse than anticipated, and no amount of stress on its theoretical advantages could overcome the embarrassing reality of its abysmal implementation. The public lost confidence in the competence of the Obama administration to do what it said it would do. Much the same thing happened in 1965 when Medicare was introduced, but at least Lyndon Johnson demonstrated the political skill to smooth over his mess.
Redesigning Electronic Insurance Exchanges
Insurance Exchanges permit the direct sale of insurance from insurer to client. That wouldn't likely please the middlemen it puts out of business. Cleverly designed, they could get around Constitutional limitations to the inter-sate sale of insurance. And by expanding to a larger market place, they provide an opportunity for niche products which cannot survive without a minimum customer base.
Creative Destruction for Health Insurance Companies
 Corporations rarely survive for more than a century.
Corporations rarely survive for more than a century.
Streamline Health Insurance?
Maybe the simplification of health insurance selection could save appreciable amounts of money, but it looks as though it might create too much uproar
to do it all at once. Compared with this, perhaps we should review the imagined advantages of one-size fits all.
Electronic Medical Record
 The electronic medical record has been an attractive idea for thirty years, but doctors find it is too much work, both for data entry and for extraction of data. Partial implementation is possible, and might even be cost effective, but there is much-hidden resistance.
The electronic medical record has been an attractive idea for thirty years, but doctors find it is too much work, both for data entry and for extraction of data. Partial implementation is possible, and might even be cost effective, but there is much-hidden resistance.
Computerizing Medical Care
 Healthcare is mainly information processing, but utilizing computers has been a disappointment. Be prepared for high costs and continuing disappointment for decades to come.
Healthcare is mainly information processing, but utilizing computers has been a disappointment. Be prepared for high costs and continuing disappointment for decades to come.
Smothered to Death in Greenbacks
New blog 2014-07-18 23:55:26 description
Average Lifetime Medicare Balance Sheet
Doing much estimating, lifetime Medicare costs average somewhere between $250,000 and $300,000 per person, not counting a great deal of custodial care.
Economics of Chronic Disease and Catastrophic Illness
Until the antibiotic era, all illness was a catastrophe. Nowadays, chronic illness can be financially catastrophic, too.
Indemnity and Payment by Diagnosis: Fair Prices For Healthcare
Trust, but verify.
Diagnosis Related Groups (DRG), in Relation to Medical Electronic Records.
 The DRG classification system was developed independently of the hospital payment system, for a different purpose. The hybrid use for hospital reimbursement has worked surprisingly well but needs extensive revision.
The DRG classification system was developed independently of the hospital payment system, for a different purpose. The hybrid use for hospital reimbursement has worked surprisingly well but needs extensive revision.
An Unending Capacity to Generate New Problems
New blog 2013-06-11 13:51:10 description
Classical Health Savings Accounts (C-HSA)
In a big legislative package, there are technical areas where the lobbyists have considerable sway in the outcome. Here are a few.
Cost Shifting: Indigent Care Out, Outpatient Revenue, In
 Hospitals probably shift costs ten or more ways; here are three ways. Picture yourself as a Congressman trying to modify this mess, and then you try to do it in a couple of weeks. Probably Galen, not Hippocrates, first said Primum non-nocere -- don't make things worse.
Hospitals probably shift costs ten or more ways; here are three ways. Picture yourself as a Congressman trying to modify this mess, and then you try to do it in a couple of weeks. Probably Galen, not Hippocrates, first said Primum non-nocere -- don't make things worse.
Cost Shifting, Reconsidered
 New blog 2013-07-16 16:55:35 description
New blog 2013-07-16 16:55:35 description
Proposal Number Seven: Buy-In Prices at Different Ages
For one reason or another, an HSA may not be able to match the deductible for a number of years.
Proposed: A Republican and/or Conservative Healthcare Solution
There certainly is a negative case to be made about Obamacare. Here is a positive alternative that should unite all Conservatives, and maybe some Democrats.
Stepping out of the Obamacare Frame
Gail Wilensky, after struggling more than twenty years to improve the American healthcare system, recently expressed her disappointment with how little reform there is in Obamacare, "only coverage extension". I feel the same way. Here are some of the things which need, and needed reform.
Pharmaceuticals:The Coonskin Hat
New blog 2014-01-10 21:50:43 description
"They Don't Make That, Anymore"
 Pharmaceutical drugs seem to follow a trajectory of fifty years, from new and expensive, to cheap, old and eliminated.
Pharmaceutical drugs seem to follow a trajectory of fifty years, from new and expensive, to cheap, old and eliminated.
Competitive Institutions: Paying for Assisted Living
.jpg) Everyone knows that Americans are living longer, but it creates some new problems.
Everyone knows that Americans are living longer, but it creates some new problems.
July 4, 1776: Patients in the Pennsylvania Hospital on Independence Day
Patients in Pennsylvania Hospital on Independence Day, 1776.
Obamacare And Its Repair, Executive Summary
Psychiatry: Last Cow in Philadelphia
 Daniel Blain, just about the most famous psychiatrist in America, lived at 20th and Olney, West. Not only was that the place he lived, but he also kept a cow there. And this was within living memory.
Daniel Blain, just about the most famous psychiatrist in America, lived at 20th and Olney, West. Not only was that the place he lived, but he also kept a cow there. And this was within living memory.
What's The Matter With a Partial Answer?
New blog 2013-04-24 17:55:22 description
All Right, Hippocrates. So What's the Basic Problem?
 Such goals unite us, unlike directionless strategies like universal health insurance; and partial success remains a total success in governance.
Such goals unite us, unlike directionless strategies like universal health insurance; and partial success remains a total success in governance.
ACA Synopsis, July 4, 2014
New blog 2014-07-04 12:18:44 description
Changing Environment
A healthy long lifestyle sometimes puts a strain on a prosperous one.
Let's Annex Canada
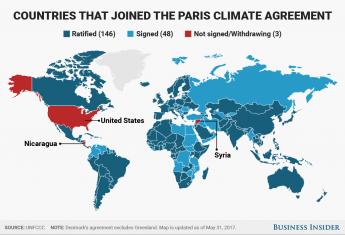 Are you as tired of global warming talk as I am? Here's a different plan.
Are you as tired of global warming talk as I am? Here's a different plan.
Martin Feldstein Does It Again: Eliminate Tacit Tax Exemption for 70% of Workers Denied To the Rest
The Henry Kaiser tax exemption for health would pay toward Social Security, indirectly paying for retirement, which health insurance prolonged.
What is the tax imposed by the "mandate" that the Republican peanut gallery is now screaming is the largest tax increase in history?
Per Wikipedia:
An annual tax of $95, or up to 1% of income, whichever is greater, on individuals who do not secure insurance; this will rise to $695, or 2.5% of income, by 2016. This is an individual limit; families have a limit of $2,085.
I don't know what "income" is but AGI seems a good guess. 1% of a $250,000 AGI is an effective health insurance premium of $2,500. I don't know how I'd like the coverage I might get for that amount but I certainly do like the price; even at 2.5%.
And, anyway, I have my own Heath insurance, so what do I care? Who is it that doesn't have health insurance and doesn't want it so much as to make such a fuss about it? Whatever the answer to that question, it sure ain't the largest tax increase in history.
With respect to taxes, the part I don't like is increasing the Schedule A threshold for medical-expense deductions from 7.5% to 10% of AGI. This is very directly a penalty for buying one's own health care policy rather than getting it from an employer who gets full deductibility or from an exchange.
Why can't the Republicans scream about something meaningful?