3 Volumes
Health Reform: A Century of Health Care Reform
Although Bismarck started a national health plan, American attempts to reform healthcare began with the Teddy Roosevelt and the Progressive era. Obamacare is just the latest episode.
Health Reform: Children Playing With Matches
Health Reform: Changing the Insurance Model
At 18% of GDP, health care is too big to be revised in one step. We advise collecting interest on the revenue, using modified Health Savings Accounts. After that, the obvious next steps would trigger as much reform as we could handle in a decade.
Reflections on Impending Obamacare
Reform was surely needed to remove distortions imposed on medical care by its financing. The next big questions are what the Affordable Care Act really reforms; and, whether the result will be affordable for the whole nation. Here are some proposals, just in case.
SECOND FOREWORD (Whole-life Health Insurance)
This second Foreword is a summary of a radically modified proposal. It cannot be implemented without further changes in the law or at least some clarifications of the Affordable Care Act. To state the issue, it is that increasingly larger proportions of American lifetimes are not employed, and therefore are not able to take full advantage of an employer-based system. It becomes increasingly doubtful that thirty years of employment can sustain sixty years without earned income if you include childhood. Further, there is every reason to expect further migration of illness out of the employable age group. And finally, while there are signs of reasonableness, the mandatory stance of Obamacare is not greatly different from a package of mandatory "benefits" imposed on all attempts at innovation before they can be tested. If changes in the law are required before implementation, liberalization might as well be in place before innovations are proposed. No private company could proceed at arm's length without advance assurances resembling cronyism. Everything else is negotiable, but the notion of mandatory pre-approval of any modification must be softened to something less sovereign.
Sickness itself has moved into the retiree age group and will continue to migrate there. The means of payment cannot move from the employee group, so a two-step process is resorted to, with the middle-man government controlling the flow of money between age groups. If we are ever to remove middle-man costs, this feature must be removed, as well. Meanwhile, the paraphernalia of medical care, the medical schools, hospitals, and doctors, remain largely in the urban areas where employment formerly centered. So the government once more becomes a middle-man, and the system begins to resemble a virtual system, based on computer systems which do the job without actually moving. Until everyone stops moving, such duplication increases costs degrade the quality and start riots. We must move people less, and move money more. At one careless first glance, that sounds like shifting money between demographic groups, but picking winner and loser demography has repeatedly been shown to be too divisive; almost a prescription for a second Civil War. In short, we have fallen in love with a computerized virtual model, based on the faulty assumption that it is without cost. Here and there it might be tried experimentally, but it is far too early to make it mandatory. Consequently, it proves much easier to re-design the payment system, shifting money between different stages within individual lives, than to make everyone find a new doctor, just because the insurance compartment changed. It is absurd to make everyone move to Florida on his 66th birthday. Even redesigning transaction systems is not easy, but it is by far the easiest choice. Nevertheless, there is still too much friction in the various systems to make such improvements mandatory.
The best model to adopt is that of the university president who ordered a new quadrangle to be built without sidewalks. Only after the students had worn paths in the lawn along their favored routes to class, did he cover the paths with concrete sidewalks.
The issue at the moment is that money originates with employers, supporting the whole system, but their employees no longer get very sick. To reduce complaints, they are given benefits to spend which they really don't need, raising the cost of transferring the money to retirees who do need the money but are covered by Medicare. We are in danger of repeating that whole cycle with Medicare, piously calling it a single payer system, when in fact it would be a single borrower system as long as the Chinese don't collapse. Expensive sickness now centers in the retirees, but within fifty years a dozen diseases will be conquered, and we will then need the Medicare money to pay for retirement living. Constructing massive systems without that vision will just make it harder to replace them. We are, in summary, in great need of a gigantic funds transfer system, since moving the people and institutions to match the funding is preposterous. But as long as the system has two champions (Medicare and the Employer-based system) in possession of all the money, we flirt with collapses in order to force rearrangements.
All of this is divisive, indeed. For years to come, the easiest thing to move around will be money. Eventually, institutions and clients can sort themselves out for geographical unity, and probably improved efficiency. But a financing system with the money for sickness in the hands of people who aren't sick, plus a governmental, system dedicated to an age group with almost all the coming sickness but unsustainable finances -- is a wonder to behold. Therefore, we offer the Health Savings Account as having the flexibility to collect money from the young and healthy, invest it for decades, and use it for the same people when they get old. It can cross age barriers and follow illnesses, or it can remain with survivors and pay for their protracted retirement. If Medicare is modularized, it can supply the money to buy pieces as they begin to appear less desirable. It can redistribute subsidies to the poor if an agency gives it money, and it can adjust to changes in geography and science, since all it works with, is money. And it avoids redistribution politics by giving the same people, their own money.
For all these reasons, Health Savings Accounts on a lifetime or whole-life model seem the logical place to fix the broken vehicle, while we somehow keep its motor running. If successful, it will grow too big, so it should remain modular from the start. It has feelers in the insurance, finance and investment worlds. It could easily arrange branch offices for retail marketing and service. It should have networks for research and lobbying. But as long as it retains the branch concept and avoids the imperial one, it should manage to keep the doctors, patients and institutions functioning as the whole universe rearranges itself -- at its own speed. The first major step in this process would be to clear up some regulations which did not anticipate it. With Classical HSA adjusted for the interim role, the design stage can be undertaken to link the pieces of a person's health financing. Variations of lifetime Health Savings Accounts can be tried in demonstration projects, perhaps staying out of the way of the Affordable Care Act by unifying parts other than age 21 to 66, as the New Health Savings Account. And then seeing which version of lifetime HSA survives the squabbling. That isn't all. The really big picture is to absorb the pieces of Medicare, one by one, as sickness retreats from being the central cost, and the cost of retirement becomes the real threat.
Foreigners Are Fed Up With Paying Our Bills.
|
| Obama Signs Health care Bill |
Implementation of the Affordable Care Act, often called Obamacare, is about to begin, but a majority of the public express fear of it to pollsters.
Obamacare is essentially a modified version of Medicare for the younger generation, so at first it's a little hard to see why that is so threatening. Presumably, Mr. Obama is also a little puzzled by the reaction, although he has an unfortunate way of attacking anyone who disagrees with him. Can it be that he fails to see the main thing the matter with Medicare itself is its cost overrun?
The first announced preference, and now the fall-back, was a "Single Payer" system, which would simply combine the two deficits into one bigger deficit. The Affordable Care Act does indeed follow fifty years of general satisfaction with Medicare for people over age 65, because everybody enjoys a dollar for fifty cents. The main source of public uneasiness arises from a vague recognition of Medicare's unsustainable mismatch between costs and revenue, which has been pretty effectively buried in a mass of information. You might say it is in plain sight, except it really isn't plain.
Medicare is 50% subsidized by debt, so everyone gets a 50% discount from real costs, and naturally loves it. But after fifty years of off-budget borrowing, the nation now wonders if we can even keep Medicare up, let alone add another program to it. The public surely does not understand how the deficit was "overlooked", maybe doesn't even want to know. But when the debt gets so large it begins to crowd out everything else the public wants, people are not stupid, and they see it plainly. In fact, they have realized it for some time, and the elderly in particular are fearful that giving the same generosity to everyone mught eventually mean taking some of it away from them.
The small businessmen who are the main strength of the Tea Party movement, see they have been excluded from the income tax subsidy enjoyed by employees of big business for the past seventy years. They are particularly enraged by the new cost barrier to going from 49 to 50 employees, and the implicit penalty for working more than 30 hours a week. It doesn't seem fair, it shows no sign of going away, and they fear to see it extended. On the other hand, the employees of big business, just like the Medicare recipients, know very well they have been given an undeserved free ride, and are fearful it will be taken away to pay for other people.
In short, the economy is hurting, leaving no room for sprinkling goodies to everybody. America's balance of trade went negative in 1965, and has stayed negative ever since. So the crunch of borrowing from foreigners was a long time coming, but it seems to be getting to an end. It can't continue without squashing someone. Omitting the youngest and poorest of our country, just about everyone recognizes that to be true, and is uneasy about where it might lead.
Since healthcare costs are "only" 17.6% of current Gross Domestic Product (GDP), extra financing might not be required for Obamacare as long as the rest of the economy remains steady. After all, we proved you could borrow 75% for short periods, by trying it for a while during a recession. Even if the nation -- at any age -- could afford 17.6% of GDP for health, some method is still needed to share out the medical debts of those who cannot support themselves. If the upper half of the population supports the bottom half, for example, and graduated income taxes take increasing proportions off the top, it's not clear even the rich could afford 17.6% medical costs plus 74% in taxes, as the French do and some economists advocate. Especially if you double it to 35% to account for the hidden subsidy, and arrive at a total of 124% of income. So the real breaking point depends on details, but a national mandate is getting clear: Don't make things worse.
From the point of view of the non-rich, it's probably worse, because it always is. Campaign rhetoric has encouraged most people to suppose their own needs will be met, but foresee minority interests suffering to protect the interests of the majority; "crowding out" is the familiar danger during a recession. Gradually raising the present 17% -- to 18%, 19% or even higher -- suggests the frog-boiling approach of heating up the pot before the frog senses what approaches. One possible limit to public tolerance can be imagined: It is plainly unacceptable for the top 49% to pay all the costs for the bottom 51%. If "fairness" means anything like that, fairness will be discarded, and that would make a fine mess. It is clear the designers of the Affordable Care Act are disconcerted by the amount of cost-shifting they discovered was already taking place, and it does not soothe the public for Nancy Pelosi to announce we had to pass the Act to find out what was in it. To act without investigation is pretty much what happened with Medicare in 1965, so it's less likely the public will tolerate a repeat of it.
 At least, don't make things worse. 
|
This book does not address redistribution by social class, but by age. The "pay as you go" system practically guarantees the last one in will get the worst of it. The proposal parade begins with only one suggestion for new revenue, emerging from modifying Pay/Go by compounding investment income within Health Savings Accounts. Because the sums are large, several following chapters explore pitfalls, safeguards, and accommodations. Following that, come a dozen proposals for cost reduction. Waste is unfortunately also abundant, and must be cut. However, it is generally less useful to hunt down villains because, after the struggle is over, we must live with each other.
Simple Gifts
So much for expecting foreigners to help us. They remain grateful to America for winning World War II, but that was seventy years ago. Forget about reserve currencies, a declining surplus of gold bars, the Marshall Plan, Truman Plan, and all that. After seventy years of thanking us, foreigners quite rightly expect us to pay for our own health care without monetary subsidies from them. Or protectionist trade policies, either.
To begin with healthcare basics, lifetime medical costs over the past century have progressively migrated toward the end of life, and the end of life has itself moved later. Lifetime earnings remain concentrated near the middle of life, so a gap widens. Collectively, the population accumulates wealth during its working years, spending its savings for healthcare after it retires. If lifetime health costs could be pre-paid and funneled into savings, with the savings professionally invested, a large proportion of medical costs might be paid out of investment income. It could be called the difference between pre-payment, and insurance, except whole life insurance, employs the same principle. Considerably expanded, this insight could markedly reduce the cost of healthcare, making it more affordable without changing it. Because medical care is undisrupted, the hidden cost of disrupting it might vanish, too. It creates what the Japanese call a virtuous cycle. (It wouldn't hurt to read this last paragraph a second time.)
 If lifetime health costs could be pre-paid and funneled into savings, with the savings professionally invested, a large proportion of medical costs might be paid out of investment income. 
|
The average American healthcare costs we are discussing are in the neighborhood of $10,000 a year, surely somewhat less for younger peopleFootnote . They are about double that for the last year of life, somewhat less than that for the first year of life. Medicare is about 50% paid for by subscribers, 50% subsidized by additions to the national debt. Ignoring inflation and tax effects, the net average real lifetime health cost at such rates would be at most $800,000, of which $400,000 would be additions to the national debt. Remember, projecting healthcare costs seventy years in advance is a very hazy business. We certainly hope these projections prove to be a gross over-estimate, but to remain on the safe side the proposal here is to make a lifetime investment to cover only the first and last years of life because the heavy costs of birth and death affect 100% of the population. The projected cost of these two benefits would be $30,000, from which $15,000 could possibly be subtracted as the national debt, or else subtracted as double-counting the cost-shifted expenses of indigents. Meanwhile, removal of the first-and-last year costs would reduce annual costs by about 4%, or $30,000 lifetime. So it seems safe to start with a $ 15,000-lifetime goal, which could be achieved by investing $8 at birth at 7% tax-free return. That's right, eight bucks. Different assumptions produce different answers; the only purpose of the example is to demonstrate easy feasibility of the approach. Multiply the initial contribution by five or ten times, and you reach the same conclusion.
Scientific advances during the last century greatly changed the shape of two curves, of lifetime income and lifetime medical expenses; future advances will surely do the same. The life expectancy of Americans roughly lengthened by thirty years and continues to increase. The logic of compound interest demands that money at 7% will double in ten years; the longer you live, the more times it will double; that's pretty old stuff. What is new and unique is the way adding three extra doublings helps the virtuous cycle, maybe changes it significantly, because 2,4,8,16,32 keeps getting a lot bigger at the far end. Three more doublings make the difference between 32 and 256, and that's a drastic difference.
But, whoa, on the other hand, the longer you keep money in a bank, the more opportunity there is for financial crashes, inflation, "moral hazard", mismanagement, changes in political philosophy, wars and a thousand other things. Eighty years is a long time from now; who says the money will be there when you need it? And even if all the 19th Century nightmares are merely pipe dreams, an awful lot of Americans remain mistrustful of financial institutions. Presidents Jefferson, Jackson, Van Buren and an equal number of nearly-successful candidates for president were even in favor of abolishing banks. A large and possibly growing number of Americans distrust the Federal Reserve, and with some reason. After all, a dollar in 1913 when the Federal Reserve was founded, is now worth a penny. Pause for a moment, reader. You have now heard both sides of the argument, the opportunity and the risk. Everything from here on details. At some point in the next century, investing a few dollars at birth will generate enough income to pay for both being born and dying, the two medical conditions which are 100% certain. It might even generate enough to pay for lifetime medical care, and more, but that isn't the point. What matters is for us to have the wit, and the courage, to take advantage of something which sort of crept up on us.
Footnote The data used here are rounded-off and approximated 2011 data obtained from HHS reports. It is intended that a later edition of this book will contain an appendix of actual 2013 statistics, the last year before the Affordable Care Act became operational.
Grand Strategy: Semi-Insured Health Insurance
Employer-based health insurance. Although improved health care has added moderately to working years of life, a lot of people hate to work, whereas to other minds, thirty years of improved longevity mostly result in a thirty-year vacation after the end of productive careers. The famous American work ethic is not universally celebrated. Pensions and savings sometimes only partially anticipate the cost of enjoying this health windfall, which unfortunately competes with yet another unexpected cost, the steadily increasing expense of dying. These changes were both rapid and unexpected, so confusion is inevitable.
There is still another way of describing this readjustment to a wonderful scientific windfall: Most sick people are now either too old to work or else too young to work, even before they get sick. Health costs therefore relentlessly concentrate toward the first year of life and the last year of life. The strategy we developed of hiding the health costs of the young and the old within the health costs of the worker class confronts the new reality: middle-aged people have many fewer health costs, themselves. That leaves less room to hide the costs of the sickly young and the sickly old, which all along have been buried within the premiums of workers' health insurance. Let's face a fact: Those who are neither near the first year nor the last year, must somehow pay for those who are -- because there is nobody else.
 Hiding the health costs of the young and the old within the health costs of the worker class confronts the new reality: middle-aged people have many fewer health costs, themselves. 
|
So now we have the Affordable Health Care Act, commonly called Obamacare. It remains to be seen whether even Obamacare can be made to stretch, because thirty years is a long time between retirement and the last year of life, and fifty years a long time to wait to judge results. With wars, globalization of industry and depressions to contend with, the task is hard, perhaps too hard. Unfortunately, having passed a law containing the Affordable Care Act mandates, we must try to do it in 2014, and do it in a rather utopian way for everybody at once. For what amounts to a level "community" premium for everyone, we must make no allowance for differing costs and pre-existing conditions, economic or medical. Many of these wounds are self-inflicted, costing the program many sympathizers who might have endorsed the same goals at a slower pace.
We Had a Secret Plan. It might as well be mentioned that Americans once nursed a secret plan for all this. We consented to spend incredible amounts of money on medical research for eliminating the disease. In fact, we made a pretty good try, considering we never officially admitted it was our goal. If there is no disease, there will be no medical costs to worry about, right? Directly confronted, eliminating acute disease would unfortunately still leave those first and last years to be paid for. There was just no escaping it, everyone has to be born, everyone has to die. And while substantially eliminating disease among the young and middle-aged is an important economic stimulant, it also lengthened life expectancy by almost thirty years in a single century. Those who managed to prosper were indeed rewarded with a thirty-year vacation, but some of the windfalls had to be set aside for those whose luck was bad, destined to spend thirty years in the shadows. It was a big, bold gamble, and in an American sense, we won it. Never acknowledging it was a goal, no one could say we lost it.
 Americans will help others if they can, but first, they must be convinced that others cannot pull them down. 
|
We are now engaged in a great upheaval described as insurance reform, to test whether a great nation which secretly believes it can do anything, can satisfy both those who believe it has attempted too much, and those fearful it will fail by aiming too low. Arguments abound. One description of victory would be this: we must abandon the essentially European idea of rich and poor as permanent classes of society. In its place, we should reaffirm the traditional Whig position that rich and poor are largely two or three, or four, stages of every American's life. In Lincoln's view, we all arrived as poor immigrants, gradually worked our way upward in society, usually taking several generations to reach the top. No more than a handful of born aristocrats ever immigrated to America. In a revised version of the same epic poem, all infants are poor, adolescents are always confused, and gradually we become self-sufficient members of society; eventually, we all die. Whigism refuses to see us as members of tribes, some eternally rich, some eternally poor; Whigs mainly hope that Liberty and personal responsibility will be sufficient to preserve the more perfect union. In Lincoln's case, it was a close call, but we made it, even then.
Obviously, people with income must support the disabled, since there is no one else to do it; equally obviously, the nation has not evolved to the point where it can be done by having one angry tribe tax another. Instead, what is needed is to organize some sort of insurance pool in which younger people contribute for their own individual future, recognizing frankly that people will chiefly fear the system cannot keep its fingers off the money to give it back eighty years later. That's really all that is essential, since many models have tested the insurance market, and watched eyes glaze over with the details.
Young people must subsidize sick old people, all right, but the only old person you surely enjoy subsidizing is yourself. For the moment, forget about the difficult transitions, about which 2500 pages of the law were written and will prove to be too little. The challenge to the country is whether we collectively have the courage to stake our lifetime earnings on the proposition that the average person can save enough of average lifetime earnings to pay for average lifetime medical costs, and still have enough left for a comfortable life. If he can't, this scheme is not going to work, because even if he can, the scheme might still fail. A thousand folksy mottos teach us that Americans will help others if they can, but first, they must be convinced that others cannot pull them down.
The Law of Compounded Interest. There's a seldom mentioned advantage to individually owned and selected insurance-like pooling of lifetime health costs. If insurance premiums are pooled, stored, and invested by professionals, they will gather investment income, or compound interest in quantities which always surprise a newcomer. To wit: money at 10% will double in seven years. Or, stretched over long time periods, the owner can withdraw 4% a year, forever, and still have as much as he started with. Within ages, 25 to 75 exists an opportunity for five doublings at 7% or 3,200%. Hidden in this is another incentive: if you only spend half as much money on healthcare as average, you can eke out another doubling, making it 6,400%. Transforming medical insurance from term insurance to a "whole life" insurance model carries the potential for vastly diminishing the lifetime cost to the average subscriber, but that opportunity probably did not exist a century ago. We may say we sacrifice this new opportunity because we do not quite believe it, but in fact, we mostly do not trust any government to give it back, eighty years later.
 "Whole life" insurance model carries a potential for vastly diminishing the lifetime cost to the average subscriber which did not exist a century ago. 
|
This paper, therefore, urges a voluntary approach, individually owned and individually selected, primarily because it seems safer to go a little slower than we could if we just followed a command. Anything which includes the word "mandatory" also forbids the testing of alternatives. At least theoretically, alternative approaches are forbidden forever, with the implication that nothing better will ever be possible. At the barest minimum, the Affordable Care Act must be amended to encourage the testing of new ideas by Congress and by state governments. Another similarly hampering word to avoid, is "perpetual", but it seems more conciliatory to avoid the word "insurance" and to outline the nature of this proposal as a non-insurance savings mechanism limited to lifetime health expenditures. To a framework of five proposals, about a dozen other features are later described but held in reserve, waiting to be added slowly as the system can absorb them. This is neither an Executive Branch initiative nor an insurance company product. It is a national strategy, which starts with individual Health Savings Accounts and builds on that foundation. It adds a high-deductible health insurance policy, preferably without co-payments. It strips down the benefits offered by the HSA to the first and last years of life, to prove the concept safely, and to pay for transition costs. After that, it should expand like an accordion to cover as much as it can afford. Beyond that point, we can argue some more, but we are aiming for maximum elimination of complication and subsidy, not because they are necessarily bad, but because they should in time be unnecessary.
Pre-Paid Death Benefits
There's an old joke about a small town with an ordinance that "Fire hydrants must be painted before each fire." Similarly, it is at first a little confusing about how pre-paid health insurance could pay for the health care costs of someone's last year of life. Necessarily, such a proposal implies the existence of a second mechanism for paying for the costs as they arise, but getting paid back for them later.
Right now, that primary insurer is Medicare. The vast majority of people who die will be covered by Medicare when they do so. So, let Medicare pay the bills, and let the Health Savings Account pay Medicare back. And looking backward, when the Health Savings Account reaches a certain amount, reduce the premiums and payroll deductions for the individual. The overall payment cycle thus means the individual only pays for his care once, with compound investment income contributing the bulk of it. The final intention is to start with the goal of paying for the last year of life, and expanding the number of years like an accordion if you have been lucky and contributed a lot toward the fund, early in life, and not depleted the fund with illness. I'm no actuary, but as a physician, I can tell you that if you have a lot of major illnesses, you will probably have a foreshortened future.
 The individual's Health Savings Account is a long-term investor in longevity, paying Medicare back when the last-year costs are known, and receiving a reduction in payroll taxes or Part B premiums in the meantime. 
|
In this example, it is Medicare, universally available for at least Part A (hospital costs), which is imagined as the transfer agent. However, it also ought to work with patient self-insurance, paying for out-of-pocket costs like deductibles and copayments, or with coinsurance, or Major Medical, or any other verifiable source of health payment. Because of such contingencies, it is better to keep track of actual expenses which reimburse individual expenses outside the Health Savings Accounts. Payments through the HSA account should certainly count if they fell within the last year of life, but safeguards would have to be created to discourage gaming the tax deduction. However, we are envisaging transfer payments only at death, so this might not prove to be the problem it seems.
There is no doubt that transferring to Medicare the nationwide average last-year-of life costs as a lump sum (rather than true itemized individual costs), would greatly simplify the accounting, and perhaps Medicare could devise a way to reimburse self-insurance contributions and other participating payers. The trouble with passing it all through Medicare is that it gives the Medicare administration an opportunity to make the rules, which other payers would immediately complain about. Itemizing also has the advantage of putting pressure on the process of billing, which for mysterious reasons now takes six months or more.
In the meantime, the money has to be set aside in some sort of "lockbox" or escrow fund. Individual records must be maintained because it is anticipated the existence of this pre-funded last-year escrow fund provides continuing authorization for reducing payroll taxes and Part B/D premiums by 4%, the amount of the future reduction of Medicare beneficiary costs in our example. Because it is anticipated that the last-year escrow system might eventually accommodate accordion-like extensions of itself, it should be careful not to take early short-cuts which would hamper that evolution. Eventually, the annual Medicare deficit should be reduced by at least 4% fewer costs in our example. Going all the way to 100% of costs is imaginable, but unwise to implement quickly without some experience to act as a guide.
Post-Payment for The First Year of Life
Having observed the medical student adventure of assisting uninsured home deliveries, where the main tool employed was a pile of old newspapers, I am acutely sensitive to the wide variation in obstetrical costs. Wide-spread obstetrical insurance is almost certain to increase the cost of being born, and the intrusion of their disproportionate malpractice defense costs also seems uncomfortably open-ended. Just glancing at the inordinately high malpractice premiums for obstetricians will tell you who is doing the suing, and for what justification.
By including the post-natal checkups and immunizations (with their own malpractice component), it becomes difficult to extrapolate what first-year-of-life insurance costs might become, under pressure of the illusion of being cost-free. However, we seem to be in a demographic decline, where it becomes increasingly desirable to increase the birth rate by diminishing its cost obstacles. If abuses can be minimized, obstetrics is one area where public subsidy seems to encounter public approval, and self-insurance is not at all practical. In fact, almost the same could be said about all health expenses up until the age of eighteen, but it seems a pity to lose the opportunity for two doublings of investment income because of unsettled disputes about marriage, divorce, feminism and the responsibility for child support.
Although expediency in the direction of taxpayer support may prove to overwhelm this admittedly contentious area, the expenditures are comparatively small, so it still seems useful to explore what could be done with first-year pre-payment. Health costs which someone must pay do exist for children growing up, and the emotional appeal of insurance for this group is strong. Getting their health care finances organized before they reach the workplace would be a useful thing since the tendency of healthy young adults to duck the costs is part of what caused a present uproar about uninsured obstetrics. All of which is to say: social gains might justify public subsidy for the first year of life, at least in part.
 The individual's Health Savings Account becomes the long-term banker for the first year of life, with the first conventional health insurer acting as short-term banker. 
|
Someone is paying for the first year of life health costs, and that someone would appreciate getting reimbursed for it, fairly soon. Therefore, the addition of less than a hundred dollars to the costs of the first health insurance company to enroll an individual would not deter the enrollment very much or even stimulate much switching between insurers later to evade it. The intent is to open a Health Savings Account, borrow from the first insurer, and pay it back when enough money has accumulated in the HSA.
If no insurer steps forward in a reasonable time, a small and temporary government loan might be in order. In return, the insurance company could anticipate a profitable and "sticky" customer for many years, meanwhile exerting more downward pressure on obstetrical costs than the young parents ever could. That is, by retaining the right to reject a customer for bringing along excessive obstetrical prices, those prices would re-open to negotiation. And realistically, a disproportionate share of obstetrical deliveries are paid for by Medicaid, which would lead to some taxpayer subsidy. In the case of uninsured obstetrics, it would appear the individual Health Savings Account itself would have to be the banker. But since the purpose of the Affordable Care Act was to leave no one uninsured, this might conceivably pose little problem. To say much more about this approach would be foolhardy until the Affordable Care Act begins operations and stabilizes its rules. The essence of it all is to make the Health Savings Account the payer of last resort for obstetrics, in the far distant future when compound investment income should be ample. The first childhood health insurer would become a voluntary short-term banker until the HSA grows enough in size to buy it back. Because it is so vital to keep opening costs low, the pressure to maintain obstetrical provider costs within reason is essential.
The advantage of looking at the retrospective payment for the first year of life lies in its quality of affecting 100% of the population. Its disadvantages mainly grow out of the ambiguity of who is responsible for the costs, the child or the parents. For obvious reasons, Society has chosen to select the parents. However, this leads to hidden incentives for the employer and the insurer to discourage procreation. In turn, this brings culture and religion into the discussion to an unknowable extent. It is probably not a safe subject for a book on medical economics, and we will conclude by merely mentioning the matter.
The First Year of Life, Leading to the Rest

|
| Locked Savings |
We have already discussed how relatively easy it would be to anticipate the average medical costs of everyone's last year of life, put the money into a securely locked piggy bank, and gather interest to help pay for that dreadful last year in the same way whole life insurance pays for funeral costs. One hard part is to keep Congress from dipping into the lockbox, or the Federal Reserve from robbing its real value by allowing inflation. However, if protecting the Lifetime Escrow can be presented as financing everyone's health into old age, the public might well rally to it. Any agitation necessary to defend the piggy bank might by itself be a boon to reminding the public what is at stake for them. By comparison, generating the funds might actually be the easy part.
But what about the first year of life, whose expenses have already been spent? (The term is loosely applied here to include pregnancy and post-partuum, plus pediatrics). The concepts are introduced of pre-funding terminal care, paying off the debts of getting born, and current-funding the long healthy stretch through most of life. The proposal is to merge it all after transition steps taking decades, fully recognizing that some people will have to pay twice for having been born, and some will never pay for having to die. Indeed, in any insurance plan, there is some unfairness in order to remove risk. First, get the terminal care fund established and funded, showing benefits in the first year or two as proof of the concept. Then, start collecting additional contributions to the terminal care fund for the moral debt each citizen has for his early childhood costs, and do it for perhaps ten years. Add this money to the terminal care fund, but make its finances as visible as if they were separate. Meanwhile, keep chipping away at the maternity and childhood costs of litigation. The first chip is to recognize that malpractice costs are disproportionately concentrated in this group, so the fund would greatly benefit from tort reform. Vaccine costs are also strongly influenced by liability costs. One subordinate goal is to present the cost of childhood as partly a score-card on progress in tort reform, broadly defined, ultimately rallying the public to restrain itself in the jury box. The mechanism would be to dramatize the disproportionate concentration of these costs by local and national aggregation, letting the news media speculate on the variation.
Finally, it should be said the Health Savings Accounts are a vastly more flexible way of paying for health care than using the service benefits approach, at a time of great flux in the system. These accounts are described in greater detail in subsequent sections, but the main advantage at this point is to translate fund transfers into money without service benefit attachments, to make unification and substitution more plausible.
To some degree, service benefits are in conflict with indemnity benefits, in a manner resembling the conflict between debt and equity in the banking sphere. The best one can hope for is to shift the location of the interface between service benefits and indemnity, bringing the friction out into public view, and equalizing the power of contending sponsors. Therefore, the best place to present the issues is to regard DRG diagnosis groups as service benefit subsets, and outpatient costs as aggregated indemnity. But one of the main mistakes of the DRG system was to extend it to every hospitalized inpatient. This is particularly important in situations where the diagnosis has no relationship to a particular length of stay or average cost level. Inpatient psychiatry should be paid for as if it were an outpatient service, and chronic diseases such as Alzheimer's disease should be excluded from DRG as well. Emergency room visits should also be separated into two groups, depending on whether the patient is subsequently admitted to the hospital.
We started by saying these issues should be chipped away, during the period when more pressing issues are being addressed head-on. The first and last years of life are disproportionately expensive, so they need special attention to cost reductions. But the list of other small issues is a long one, providing ample opportunity for trade-offs within ambiguous opportunities. The main goal of these new proposals is to redirect cost-shifting perceptions from something to escape if possible, into a vision of advancing sensible provision for your own risks at a different age. The notion of generating investment income is not a small part of the notion of prudent behavior.
After this short treat, of a long-term vision, we now return to more practical short-term proposals. The heart of them is the Health Savings Account, but several preliminary features must be explained in advance.
Ideal Universal Health Insurance on the Accordion Model
Let's compress the basic idea to simple end-of-life funding, to show how much can be made of the two basics. And then using the accordion model, expand the basic ideas to five, in order to cover the health expenses of an entire average lifetime. And eventually, expand the patient contributions to match. If the parents or grandparents of a newborn child deposit $2000 in a Health Savings Account at the time of the child's birth, using 7% return as the projected lifetime average investment return for life in an index fund of the entire American stock market, and do not disturb the account for a life expectancy of 80 years, there should be $512,000 in the account at the baby's death. That is the extreme limit of optimism, generating far more income than is likely to be needed. Beyond this limit, overcoming initial obstacles of a zero-interest environment, the uncertainties of inflation and war, resistance by competitive insurance and political alternatives, and other risks and alternatives -- make the whole project unlikely to succeed. That sort of defines the general limits of the idea's initial feasibility as extending from a low investment of about $10 to an upper limit of $2000; more is possible, but this is enough. It uses two ideas (the Health Savings Account and the Last-Year of Life Escrow) to show that there is surely enough money generated to cover the cost of eliminating the last year of life cost of Medicare. With that sum in escrow, a calculation should also be possible to estimate how much Medicare premiums might be reduced for the owner of that escrow, acting as the ultimate goal of everyone involved. There are of course some people who would want a solid gold casket for their own funeral, so there probably must be some "service benefit" features to the program, but in general, it is envisioned as an indemnity, leaving the issue of price control undefined for the present. Taken all together, a package can be assembled within the rule of reason to show how much a lump-sum advance payment would reduce Medicare premiums as an incentive for the average person to enter into it. Naturally, if you wait to enter into the agreement late you will need to deposit more money, but that figure is easily derived from looking at the average net value of four or five index funds at the time you finally make up your mind to take a chance on the idea. No doubt, beginning contributions at the age of twenty is more realistic than having a grandparent donate at birth, but it becomes too complicated to establish detailed premiums right now. If you wait until you are twenty, you will need to deposit approximately $8000 to catch up; or only deposit $2000 and be satisfied with a final balance of $128,000. The longer you wait, the harder it gets, and no doubt the proponents of "pay as you go" will object to it. But that's exactly why individual options are preferable. You can start with one program and switch to the other, but it becomes more expensive if you wait. Those who recognized a bargain earlier are rewarded for their risk.
Now, $512,000 is probably more money than is necessary in the idealized, no-problem example. So, let's see what it would take to fund the projected lifetime healthcare costs in their entirety, no illnesses, no stock market crashes, no fees or taxes. The amount projected is surely enough to cover that and leaves some room for illnesses and administrative overhead, but it's getting closer to the bone. At the very least, you would have to subtract the premiums for a $5000-deductible catastrophic health insurance policy, guaranteed renewable, of course. That's needed to pay the retrospective cost of having been born, well-baby visits and all that, so it must have a premium somewhat higher than the quoted one. And there probably ought to be a surcharge for re-insurance, in case the deductible is invaded more than once. Remember, the assumption made is that you will remain in perfect health, which is definitely not the average experience. So, it probably must be conceded that you will also carry routine healthcare insurance for maintenance during your working years, or else pay for your working-life healthcare out of pocket. Out-of-pocket may actually be better, in order to support an active marketplace to set prices, because providers must always be suspected of exploiting a heavily insured environment. On the other hand, let's not be completely naive about the inner workings of life insurance. A lot of its profits are derived from subscribers who drop their policies and never file a claim. Let's go over this, once more:
Liberalization of the Health Savings Account.To start with, let's begin voluntarily, and let the success of the first-responders encourage the timid. There are surely several thousand new parents (or more likely, grandparents) each year who know a good deal when they see it and could afford to pre-fund health insurance for their newborn children for the rest of their lives. (Class warriors will snort to hear this, but it is a basic fact of risk-taking that well-to-do people are about the only ones who can afford to take the untried risks of trying something new.) Starting at birth adds a couple of doublings, and reduces the lifetime net cost remarkably; middle-class people have to hang back because a loss means more to them. Portrayed as an estate tax deduction, it would seem an attractive generation-skipping way to transfer income to the next generation and to grandchildren who would be thereby relieved of the obligation to support the middle generation. Ask your lawyer to explain it to you, it's a good deal.
Do not put a limit on contributions to a Health Savings Account for the children; what's the point of limiting contributions when withdrawals are going to be limited to actual health expenditures? Surplus funding would only be lost and is therefore self-policing. (Eventually, any surpluses in the account should flow into a reinsurance fund for those who exhaust their deductible more than once.) Your accountant can explain that one to you. After the first year, non-participating members of the child's age cohort can catch up by contributing, not the same amount, but the average amount to which the fund has grown in the meantime.
The contributions themselves should be invested in index funds for the whole U.S. stock market, so if stocks have gone down the latecomers have a chance at a bargain, if the index has risen, it shows what a good idea it has proven to be. Essentially, it is an investment in U.S. common stock, which in all but occasional years can easily prove itself. As explained later, the fund will have to maintain a certain investment in U.S. Treasury bonds in order to pay claims, but the extent of this will depend on what the benefits include.
From this basic investment must be subtracted the cost of a catastrophic health insurance policy for the child, with a deductible not less than $5000, net of inflation, to be purchased with the dividends of the fund (premiums for the catastrophic policy are waived until the dividend income will cover them). Essentially, this insurance policy is the source of advance funding for the last year of life escrow. By shifting catastrophic premiums to later years, it is also retrospective funding for the first year of life.
Last Year-of Life Escrow. The issue of trusting anyone, even our own government, with appreciable amounts of money for eighty years is solved in the following way: The funding has been described; it is placed in an index fund and remains there until the beneficiary dies, theoretically eighty years later. The investment performance is therefore widely available on a daily basis. Meanwhile, the average annual cost of the last year of life is available from Medicare. Meanwhile, the average life expectancy of the age cohort is available from the life insurance industry; the average yearly investment return is published by the index mutual fund industry. A year after the death of the beneficiary, the fund transfers the average cost of the last year of life to Medicare and publishes the investment results and theoretical results of alternatives to the cohort. What to do with any surpluses remaining in the fund need not be fully described at this point, but it is envisioned that surpluses remaining after the death benefit is paid to Medicare will go toward the first year of life, followed by other years if additional surpluses appear. On the other hand, reducing the cost of Medicare for the last year of life would enable a reduction of the premium costs for other years, so perhaps it would be better to pay off the existing debts of Medicare.
The immediate purpose of the steps described is to reduce the cost of Medicare. If it does not cover the complete cost of the last year of life, it at least reduces it significantly at little administrative cost. Since lifetime medical costs ordinarily reach a peak during the last year, there is a potential for virtuous cyclic increases to include more of Medicare costs than the last year alone, but this is not promised. If it reduces Medicare costs significantly, donors of the fund enjoy lower Medicare premiums than otherwise. Numerous alternative proposals are available, as described in later sections, and it is not useful to start unnecessary quarrels about such contingencies at this stage of the debate.
Commentary This proposal combines features of first-year and last-year insurance, resting on a framework of Health Savings Accounts, with the funding incentive of generation-skipping tax avoidance to provide seed capital. With adjustments based on revenue experience, it can be designed to remove about two-thirds of lifetime medical costs from future federal budgets, but it intends to leave undisturbed the comparatively routine health costs of the working population. Although it addresses the majority of costs, at present it affects only two years of the average lifetime and does so by indirect reimbursement.
Problems Needing Attention. Seventy years of health insurance have demonstrated that any provider system will readjust to any generous source of funds by attempting to make it even more generous. It is a theory of mandatory universal coverage that eliminating other funding sources will result in the elimination of cost-shifting, but unfortunately, it will not. State and federal governments compete to shift costs to any easy revenue source, and both the suppliers and the management of healthcare institutions will unceasingly seek to increase their share of the revenue from a compliant source of it. In retrospect, it is extraordinary that we ever thought otherwise. Therefore, this proposal seeks to provide easy income to the health system, but it will surely fail if it relaxes its vigilance. Therefore, the absolute minimum requirement is to lodge investigative power at both the federal and state levels, to be certain that only market-based prices (or relative values) are paid, and that indirect mark-ups are reasonable. It seems advisable to retain a small portion of healthcare costs with the consumer so that rebates and surcharges coming from the main fund will serve to remind the public of its need for vigilance.
Secondly, if cost controls do become efficient, incursions into the quality of care must soon be looked for. Professional self-regulation is one defense, consumer vigilance is another. Both approaches suffer when they are undermined by careerism, of which the plaintiff bar is an outstanding example. The whole matter needs re-examination, and probably would be improved by establishing greater direct tension between these three groups with the greatest conflicts of professional interest. At the moment, they all need more term limits if rotation within professional silos is not feasible. The Constitutional Convention of 1787 would be a good model for working out the proper balances between interested parties; they should be given six months to work it out, but not a day longer.
Concerns Provoked by "Whole life" Health Insurance
An entirely new concept like reconstructing health insurance on the "whole life" model can be expected to provoke concerns. Here are a few of what surely is not yet a complete list:
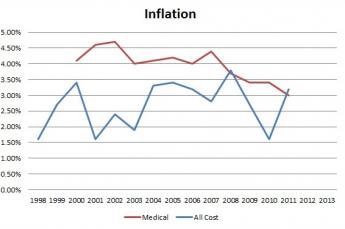
Inflation. It is true that rampant inflation would be injurious to the whole idea of permanent health insurance. However, it is the job of the Federal Reserve to maintain price stability, and many changes have taken place in the Federal Reserve's methods of operation since 1913. The most notable one was the abandonment of the gold standard by President Nixon in 1972 as a late consequence of flaws first introduced at the Breton Woods Conference in 1945. Observers may be of the opinion that the gold standard was stronger protection against inflation than the present inflation-targeting one, but the latter is nevertheless the system under which we operate. It should be recalled that in 1945, America had two-thirds of all the gold in the world, and international trade was being stifled by the unbalanced distribution of any common means of exchange. The correction of this gold maldistribution finally came to an end when a correction was no longer necessary, and indeed in 1972, it was possible to foresee an American gold shortage if trends continued. The American currency is no longer supported by a link to gold or any other commodity. In its place, the Federal Reserve issues or withdraws currency from circulation in response to inflation, attempting to maintain a steady inflation rate of 2% to match the growth of the economy. There are disputes about exactly which inflation rate would be ideal, but the ability of the Federal Reserve to maintain its stated targets has been reassuring. While there is room for argument among economists about the precisely optimum inflation target, the variation has been less than 1/2 %, even in times of economic disorder as severe at the present one. The projected finances of funded health insurance can safely sustain much greater miscalculation than this. If a threat is present, it comes from other directions.
|
| Inflation |
The suggested choice of an index fund composed of the entire list of domestic American common stocks was intentional and may be vital. The Affordable Care Act's provision for mandatory universal coverage makes it official that the full faith and credit of the American taxpayer stands behind the funding, so the American stock market is a close surrogate of that pledge. Anything which could destroy the stock market would constitute a threat to America much greater than a collapse of its health insurance, and enormous efforts would surely be invoked to prevent such a disaster. The wisdom of ransoming the whole economy to a comparatively small component of itself can be questioned, but it is nonetheless difficult to imagine a default when such heavier consequences would follow it. The same can be said of a permanent stock market decline, a devaluation of the currency, or a bond market default. These things can happen, but injuring health financing would scarcely enter the discussion.
The Changing Mix of Disease. Most of the rest of the world still concentrates its medical attention on the treatment of contagious diseases. In America, contagious disease scarcely makes the top ten concerns. No one would have predicted this a century ago, and no one can predict the mix of diseases, or their cost, a century from now. We do know that people will continue to be born and invariably to die, but we do not know what will kill them or what it will cost. It is even possible that an epidemic will unexpectedly sweep the globe, or an asteroid will hit the earth, but in general, big changes occur over more than a decade and give some time for readjustment. We tend to feel confident that our longevity will continue to lengthen, although in Russia it has lately shortened. Generally, new treatments have patent and development costs at first, and then become cheaper. But even healthcare workers enjoy raising their own salaries. It is difficult to predict population costs for healthcare eighty years from now, or whether they will be distributed evenly throughout the population. Unfortunately, this uncertainty will bedevil any system of financing that can likely be devised, but that does not mean reimbursement systems cannot be designed to cope with it.
Therefore, it is essential that any long-term plan, not just this one, build an accordion system into its initial design, and assign the task of watching over this problem to a permanent oversight body, particularly one which is able to resist the general economic pressures bearing down on the Federal Reserve. Inevitably, there will be times when the two bodies are adversaries. The easiest approach is, to begin with, the first and last years of life as anchors, and extend the reimbursement to intervening years as needs can be projected. This is one of several reasons why it is advisable to anticipate two parallel systems, one paying the bills as they appear and raising premiums if need be, while the other reimburses the first one as its fund permit. If a cure for cancer or Alzheimer's disease should appear, there might be funds to reimburse the other system for eight, ten or more years, readjusting premiums as it goes. If those miracle cures prove to be astonishingly expensive, the accordion would contract the other way, or its premiums would readjust in the other direction. Let us be clear what we are attempting: to reduce the annual premium of health insurance for the working years of life as much as we can. We must resign ourselves to remaining uncertain how much the premium can be reduced in the far future. No one spends public money as carefully as he spends his own. Complexity is therefore useful in areas where moral hazard is an important issue. Otherwise, grown-ups will behave like children at someone else's picnic.
Fluctuating Interest Rates.
At the time of this writing, the Federal Reserve has forced American short-term interest rates almost to zero, and held them there for three years. Japan did the same thing two decades ago, and they have had the unprecedented experience of remaining near zero for nearly twenty years, held there against the will of the Ministry of Finance by what is known as a "liquidity trap". Meanwhile, by the Fed buying long-term bonds in what it calls QE3, long-term interest rates have been forced in the opposite direction to a higher level than normal by the Federal Reserve. It is not necessary to explain here how this was accomplished, or why.What it is important to see is that the value of bonds, both short and long-term, can be manipulated by the Federal Reserve at the will of the Chairman or at most a handful of committee members. Therefore, predicting future prices or rates is nearly futile for everyone else, and investing in bonds is much riskier than it seems. However, there are economic consequences to interfering with markets, so over long periods of time, there are limits to what the Federal Reserve can do without destroying the economy. In a sense, this is one of the prices we pay for controlling inflation by inflation-targeting. There are boundaries within which the Federal Reserve can operate, and eventually, interest rates will revert to their long-term averages. In the very long run things will average out, and in the present context, we are imagining investment horizons of eighty or more years. This is why insurance companies can buy bonds with serenity, and just wait long enough for interest rates to normalize. But there must be an organization with some feature of immortality to intervene if the counterparty (The Federal Open Market Committee) is immortal and has unlimited funds at its disposal.
However, the Federal Reserve is not independent, no matter how hard we try to make it so. We are here discussing money which belongs to individuals who can vote, and who will surely be concerned about the investment policies of 17% of the Gross Domestic Product. The Federal Reserve can thus be easily imagined to develop an occasional severe conflict of interest between what is good for healthcare financing and what is good for the economy as a whole. The pressures which the public might decide to exert are not predictable, except that they would be hard to resist. The public has long proven itself to be a poor investor, buying high and selling low, even when it knows better. It almost seems better to avoid bonds in the portfolio of investments entirely rather than take the political risks, until it is recognized that this fund would soon develop the need to pay its claims every year, even if the stock market is at a low or stock dividends are zero. Therefore, it becomes clear enough that when bonds start paying 4% or more, the fund ought to buy some of them and hold them to maturity, just as life insurance companies do. Perhaps it becomes clearer why insurance companies hold a portfolio of 60% stocks and 40% bonds, but it is not exactly clear what to do when a fund of this size proposes to start when interest rates are at their present extreme. This sort of technical issue just has to be left to bond market professionals, since it involves short selling and other arcane issues that the public ought to know enough to stay away from.
The Investment Fund Becomes a Gorilla. Any insurance company must segregate a claims reserve fund, to assure it always has money available to pay its claims. In the system we envision here, the potential claims are too far in the future to be confident how much they will eventually become for a newborn baby, etc., but for the cohort just beginning that last year of life, the average cost of the previous year's Medicare claims will be abundantly clear in Baltimore, where they keep such records; it will probably be close to 20% of Medicare's budget. It certainly will be clear contributions to the pool of Health Savings Accounts cannot possibly match the claim cost of the first year in operation, and should try to do no more than reducing the initial end-of-life claims by whatever is available.
Adverse selection of beneficiary composition. Since the actual beneficiary would be the Medicare Trust Fund (and not the subscribers, who would then be dead) the impact of the news of this program would focus on the reduced Medicare premiums for younger subscribers. Medicare premiums would be reduced by no more than 20%, which would nevertheless probably be greeted as a windfall. The true beneficiaries would mainly be successor cohorts already in retirement, although paying off some of the Medicare debts dating back to 1965 would be a splendid idea. The fund will gradually level out, but it will likely take at least ten years to do so. Social Security and Medicare had the same problem at the time of their beginnings and elected merely to borrow the money, essentially never repaying it to the "pay as you go" system.
Eventually, Medicare will be put to the expense of developing premium billing systems of some complexity. At least, this new system has a source of revenue in the investment of its cash accumulations, with an estimated time of twenty years for it to catch up with itself. Much would depend on the medical costs of the twenty years prior to the individual last year of life; at the moment, they are might even be sufficiently lower to make this approach workable. But if some new treatments, for cancer let us say, are more expensive than the years they would add to longevity, this mixed blessing would have to be treated as an independent problem. Other solutions are available; the ability of the government to borrow at lower than prevailing rates are based on the assumption that it is a sovereign debtor. While this advantage is not guaranteed, it does exist and probably would be difficult to change. Furthermore, whether pre-funding would initially appeal more to younger or older people is hard to predict, calculating the potential source of revenue or losses from various mixtures would have to account for any difference in costs among various ages. Creating enrollment quotas for various ages in the early years of an accordion expansion might be workable.
And then, there are some macroeconomic perplexities. As mutual fund and index fund usage expand, fewer stockholders vote their proxies; the present proposal would make this problem worse so there would be even less resistance to lavish management salaries. The influence of family controlled stock within the portfolio, and of hedge-fund control would increase; possibly, foreign control would be easier. While true enough, these issues are not for this paper to deal with, only to mention.
The success of a pre-funded program would probably be judged by the extent of voluntary acceptance of it, and success would mean the endowment fund grows to be vast and well-distributed. Success would entail huge sums of money, potentially disruptive of the existing financial system. At peak capacity, the financial markets would have to absorb weekly inflows of about 1/4% of GNP, and eventually liquidations of double that size. Success might also entail a significant shrinkage of our oversized medical complex. Background churnings of that size would soon underlie every calculation in the markets, with uncertain consequences for what would probably be a steadily growing world financial marketplace, perhaps a disruptively international one. Not everything can be predicted so far in advance, but it is safe to say it would be tested for flaws until the markets conclude it is flawless, a very long time indeed. Such a Leviathan cannot be set on automatic pilot, but neither dare it relies on having the wisdom to make unblemished mid-course corrections. There are risks in attempting a middle approach, which must just be accepted as being less than the potential rewards of taking the risk.
No Plan is Free of Risk; Long Range Planning is Political
In recent years, Congress has taken to producing laws of great complexity, sometimes thousands of pages long. This is particularly notable in the Obama administration but can be viewed as a non-partisan tendency throughout the Twentieth century, starting with Teddy Roosevelt and Woodrow Wilson. As part of the phenomenon, the workload of Congress has increased to the point where the Legislative branch is particularly weakened by its traditional procedures. The Executive branch has responded greatly enlarging itself, able to create most of the Law through regulation after the law is passed; and the Legislative branch reacts by creating excessive detail in later laws. This recipe for self-defeat has come to be called "micromanagement" by business theorists, who tend to view "command and control" as a solution. As long as the Constitution stands, that approach will not be allowed to work. It is not the purpose of this book to redesign government, or even to discuss it in detail. However, it is wise to remember that even good proposals are undermined by the change of circumstance. Unwisely freezing details when not truly necessary could defeat the main goal, which is to pay a large share of health costs with compound investment income.
 The main goal is to pay a large share of health costs with compound investment income. 
|
The main concern is this: our present or future systems of managing the currency may not permit compound interest to compound faster than inflation. That can't be blamed on the Health Care system, but it would certainly injure health care. At the present moment, long-term U.S. Treasury bonds pay 2%, but inflation reduces the value of the bond by more than that, perhaps 3%. Income tax reduces the value by perhaps 0.5%. The graduated income tax already makes it useless for the top quarter of the population to buy Treasury bonds, to say nothing of the top 1% of the population. Whatever the outlook for bonds, insurance companies must keep a large bond portfolio to pay claims. Whatever the outlook for stocks, a large stock portfolio is necessary to stay ahead of inflation. The public must not force its managers to ignore these rules in order to match the investment results of others.
Congress has responded to unrelated pressures by trying to collect the same taxes from a loophole-less tax code, primarily for the purpose of lowering the rates on the top bracket. Whatever the outcome of this struggle, it dramatizes that the usefulness of investing in bonds can readily be destroyed by modifying the tax code, by the stroke of a pen, as it were. You certainly would not want your lifetime health insurance to be risked by that sort of thing happening, sometime in the next eighty years, so you do not want the government to be too tightly in control of your investment portfolio. You may love your government, but its agenda is not necessarily in harmony with that of an insurance company.
Legislative extremes probably won't happen, because of the historic sensitivity of Americans to taxation. But inflation could be equally destructive, and control of that lies in the hands of an un-elected committee at the Federal Reserve. Much of this power was unintended, created by going off the gold standard, and then replacing it with the power of the Federal Reserve to issue (or, not issue) vast amounts of currency in response to "targeting" inflation at 2%. Since a casual observer has trouble seeing much of a match between 2% and the actual amount of currency issued, the Federal Reserve Chairman has been given wide latitude in adjusting interest rates for his own purposes. The outcome for present purposes is that a fifty-year history of this system would have allowed the following statement: "You could withdraw 4% a year from an investment fund, indefinitely, and still have the same amount remaining in the fund." In the past year, however, the following analysis emerged from David C. Patterson, the CEO of a very large investment fund: "A draw of 3% a year at any time since 1926 would only have resulted in a steady purchasing power 60% of the time." Whether this attack on a fundamental investing maxim was caused by inflation, going off the gold standard, or the actions of the Federal Reserve, it is a lesson that interest rates cannot be predicted eighty years in advance, within the boundaries of what experienced financiers considered safe enough to depend on.
The Bottom Line. The life insurance industry faces exactly the same problem, and if the life insurance industry has a solution, it hasn't made it public. What the life insurance industry surely has, is lobbyists. The solution they would devise doesn't necessarily address someone else's problem, but health insurance for the last year of life comes pretty close to what they do for funeral cost protection, so one could be confident they would be allies in any congressional manipulation of income tax upper brackets, to the disadvantage of investment funds. And the same thing could be said of the financial community. And the banking community, so one could be reasonably confident there would be plenty of allies against any overt congressional assault. That does leave the loopholes created in any plan by the unintended consequences of some other plan.
All in all, it seems the best strategy to begin with an investment fund which has already been authorized and given a tax exemption: the Health Savings Account. Put as much as you can in one and let it grow. Spend it for some health expenditure if you must, but anyone who puts in two thousand dollars at the birth of a grandchild is probably going to be glad he did, even though it might be left undeclared just how it would later be spent or disposed of. Walk a couple of blocks and open a debit card for the fund, and walk a few more blocks to a broker who can sell you a high-deductible health policy. Link these three features together when, and only when, some changed circumstances make it useful to link them in a single integrated system. If this direst of dire circumstances never comes about, you are no worse for leaving them independent. But if something bad does come about, you may possibly be motivated to change the basic arrangement, or even dissolve it and take your money out of it. Under really dire circumstances, your own ability to judge what is sensible is probably the best protection you can reserve for what is, at the best, a very dangerous world we live in. For far distant planning, it is necessary to rely on our form of government to produce leadership which can handle the problems.
REFERENCES
| The Game The Fed Plays With Your Investments | Wall Street Journal |
| The Federal Reserve And Financial Crisis | Amazon.com |
Comparatively Easy Financing for the Uninsured
|
| Paul Krugman |
Paul Krugman has been quoted as saying "Health Savings Accounts will increase the number of uninsured while benefitting only the wealthiest taxpayers." In fact, financing healthcare for the uninsured is pretty simple, if it would use Health Savings Accounts for pre-funded insurance. To do the very simple math (mind the zeroes, please), giving or loaning $5000 to 30 million uninsureds would cost a total of $150 billion dollars, or fifty billion a year for three years. By contrast, the annual deficit of Medicare alone is $250 billion. We'll get to the quibbles in a minute or two, but because most people aren't accustomed to dealing in numbers so large, let me introduce the jab that financing permanent health insurance for the uninsured would be quite a relief, compared with the unsustainable costs looming for the Affordable Care Act. The Federal Reserve currently spends $80 billion, every month, purchasing treasury bonds which perhaps few private investors should buy. The HSA subsidy cost would not be entitled to tax exemption, so it would actually be somewhat cheaper than $150 billion after-tax. This isn't a monthly cost we are describing or an annual one, it's a one-time expense, spread over three years.
To repeat the refrain, this one-time expense if invested would comfortably fund the average lifetime health costs of the uninsured population, except for one thing. The clients would have to buy a high-deductible health insurance policy (but only during the years the account is building itself up after being used), paying benefits in audited costs, not posted charges. People eligible for a subsidy would probably invade the fund for small expenses more than tax-sensitive people do so the statistics on existing use may be skewed. There would be startup administrative costs. State laws mandating small-cost items would have to be re-examined. Before all this cost shifting became popular with hospitals, the AMA offered its members a $25,000 deductible for $100 annual premium.
Yes, there would be an annual in-flow of new uninsured being born or imported, and so there would likely be a mechanism for recapturing the loan from those who move out of the subsidy category, structured so as not to act as an incentive to remain uninsured. No one can possibly predict future cures for disease or their cost/benefit, but that is true of any system. We hope the cures will increase and their costs will go down, but we certainly can't promise it. We can safely predict that reducing the cost of the uninsured would reduce everybody's liability for them, including the wealthiest. But also including minimum-wage earners, for whom a proportional reduction would be much more beneficial and welcome. And -- the 30 million recipients of this subsidy would undeniably be better off. It would, however, be entirely sensible to use part of any savings to reduce the national debt from earlier borrowings.
It would, however, be entirely sensible to use part of any savings to reduce the national debt from earlier borrowings. Furthermore, newspapers relate we have 7 million people in jail, and we steadily produce replacements when they are released. There is a constant inflow of new citizens mentally retarded enough they will never be self-supporting. The local school district where I live spends 8% of its budget on what it calls "special services for the mentally handicapped". The uninsured will always be with us. The American public is spending, and will always be spending, a great deal more on charitable healthcare than it gets credit for. We probably should be spending even more on these problems, but universal health insurance isn't going to do the job.
Without much doubt or dispute, the most serious problems with implementing this funding innovation would come from unanticipated effects, about which its opponents would be happy to expatiate without help from its proponents. In general, unanticipated effects begin to appear slowly, and if we remain alert, they may be minimized. But what about the unanticipated beneficial effects? If we really succeeded in wiping out the main causes of health cost, what then? Since an awful lot of people are employed within 17% of gross domestic product now spent, what in the world do we do with them if the expenditure is seriously reduced? Come to think about it, you really have me, there.
Increased Potential for Retirement Villages

|
| Pennsylvania Hospital, Nation's First Hospital, 1751 |
Healthcare institutions may well have mission statements, but the main force visibly shaping hospital mission is third-party reimbursement. One must be sympathetic with institutions which really prefer their own mission to the pressures from third parties, particularly when the "second party" -- the patient -- also likes the original mission better. Teaching hospitals surely would prefer to concentrate on streamlining tertiary care, retirement villages on enriching the lives of elderly residents, etc. And they could probably make a better case for what they prefer than third-parties can. When one-size-fits-all health insurance is imposed on institutions which must survive by internal cost shifting therefore, insurance mandates invisibly prevail. It is not always strictly a matter of "Who pays the piper calls the tune", as it is "Who pays the most can run the place."
Considering these invisible forces of control at work, it seems highly desirable to search for situations in which the incentives of the third-party do not run parallel to the incentives of the provider community. In the case of government third-parties, the goals of the agency may not even be parallel to the will of Congress. The public clearly prefers to pay for private rooms and private duty nurses if it can afford to, but those are mainly relics of the past. Doctors used to work out of offices in their homes, but you seldom see that, now. There once were twenty hospitals in Philadelphia which were owned, paid for and operated by churches, but now at most, the church name is a relic on the front door surviving from a former era. If these changes were a response to public preference it would be another thing, but they are usually not even traceable to a written mandate which might be appealed. So it becomes all the harder to defy a mandate which grew out of the hospital's surmise as to what the third party would probably prefer. Perhaps some examples of social pressures at work would be useful.
It happens my own first office experience was in the home of an older doctor on vacation. The location of that family residence was a careful triangulation of convenience, expense, distance to the hospital, and the preferences of the patients. It was a grand experience to put aside the breakfast coffee, walk into the next room, and see the first patient of the day. Or to interrupt office hours for an emergency in the neighborhood for less than an hour and to have your excuses readily accepted by the waiting patients upon return. My colleagues had explained the financial advantages of sharing a roof and heating system with a tax-deductible business. But my accountant explained that the Internal Revenue Service didn't like offices in the house, and would surely audit any doctor silly if he persisted. So I spent fifty years in an office across the street from the hospital, commuting and seeing patients who had to commute to see me; the extra expenses of parking and the rest of that arrangement are easy to imagine. True, it was easier to visit the hospital patients, and nice to eat lunch with other doctors in the hospital cafeteria. But all of these decisions were not my own first choice. I never got a letter from the IRS or heard a murmur from them, but I always believed I was responding to their mandate. When an IRS agent finally wandered into my office as a patient, he admitted the IRS prejudice but said he believed it grew out of fear the business expenses reported would really be the expenses of a hobby, not a business.
A second relevant experience occurred when I was a resident physician. A staff physician at the hospital had a heart attack, and the Chief of Medicine asked me to take a few days off to tend to the problems in the stricken doctor's practice. His home and office were in the midst of a row-house district of town. When I arrived, the office was empty of patients, but the nurse was waiting with an umbrella. "Before we see the office patients, we must make rounds to see the bedridden patients at home." To my amazement, within a three-block radius of his office, there were nearly twenty patients in hospital beds at home. Some of them had oxygen tents, several of them had intravenous fluids dripping into their arms. The nurse told me that she drew blood for pickup by a laboratory and that with a little argument a portable x-ray machine could be brought to the home. At the foot of each bed was a hospital chart, all up-to-date with notes and reports. It might not be possible to run such a show in many other neighborhoods, but the city row house neighborhood was ideal. Or, not ideal perhaps, because there must have been many problems. But it was clear why Blue Cross had slow progress making sales to the people accustomed to this arrangement. And it even made clear why patients were content with open twenty-bed wards in a hospital, for at least ten years after Medicare would have gladly paid for a semi-private room. No private duty nurses, however, it might set an unwise example.
Two things are at work, here. Things happen to medical care which is undesirable, so someone needs to complain about them, and complainers must be provided with a place to appeal. The reverse is also true; good things which ought to happen, don't happen. So in addition to providing an appeals system, we somehow have to provide a wise and unbiased ombudsman to suggest what new initiatives ought to be undertaken. And the two functions, negative and positive, need to commune with each other. Parenthetically, since everybody gets involved in health care to some degree, adversary roles must be filled in this process, containing representatives of patients and also providers (both institutional and individual), as well as guardians of the purse. Since the process quickly becomes unwieldy, it needs to be associated with a special committee of Congress and needs to be able to summon both witnesses and experts. An annual convention in some pleasant spot might enhance the concept.
Institutions are another matter since quite often the personal opinions of the spokesman are constrained by the incentives of the institution. It must be made clear to them which opinion is desired.
Institutions choose their location for other considerations, chief among which is cheap land, but the location near public transportation is another factor. Whatever the thought process underlying it, nursing homes and retirement villages are almost always in the far suburbs. A related problem is a vexing difficulty for a center-city hospital to find a nearby nursing home for convalescents. These annoyances are protracted by the licensing rules in a round-about way. When a corporation is formed, typically a lawyer with a yellow pad asks two questions: "What are you going to name this organization?", and then, "What is its purpose?". Presumably, he then completes some forms and files the necessary applications. The stated purpose may well have other uses, but it defines the sort of license needed, and eventually either match or does not match the rules some third-party reimbursement agency has laid down for what sort of institution is eligible for reimbursement. After that, the system becomes much more rigid than it needs to be. As long as the institution remains defined as a hospital it will be paid by the third-party, and without that designation, it won't. Effectively, the state licensing board acquires the power to shut off the revenue of some institution which displeases it. But what displeases it (let's say, mice in the kitchen) usually bears a scant relationship to whether or not the institution is capable of performing additional tasks. It does not take long for these issues to get blurred and forgotten; the retirement village can't receive hospital reimbursement because it doesn't have a hospital license. A hospital license would permit it to do a lot of things it doesn't want to do. While the general idea is sound enough, the rigidity it imposes is excessive, particularly when you consider the penumbra of reluctance it provokes from employees. Obviously, the interpretations vary greatly between jurisdictions. It leads to hospitals which may perform heart transplantations but may not run a day-care center for the children of their employees.There are many simple solutions to this simple problem, but because so much of it is buried in-laws, it would probably require a special court to be appointed to oversee it. How busy that court would be would depend on how vigorously competitors would resist it, which would probably vary with the region.
In any event, Society has a legitimate interest in preserving the quality of care, but it does not fulfill that duty by transferring it to reimbursement agencies. During wars, surgery is satisfactorily performed in tents, for an extreme example of how expendable much oversight can be. Another principle would be to ease impediments to overlaps of functions between institutions, particularly including the backward sharing of component services and records toward the lower-level institution. Since such sharing is often observed to occur without objection within vertically integrated institutions, there is every indication it is both desirable and feasible between competitors.
Going much farther back to the town meeting form of oversight, the most radical departure from present custom would be to encourage a shift of the center of care from inpatient hospitals toward retirement villages. The simplest definition of the center of care would be the location of primary physician offices, and the most important step would be to discourage mandatory links between referring physicians and particular acute care hospitals. Doctors left to themselves will locate where the patients are, and increasingly it is possible to see a shift of patients requiring chronic disease management and terminal care into the retirement village. The tendency of doctors and laboratories to cluster around hospitals impedes this natural shifting together. If doctors shift their offices and are allowed a choice, laboratories and x-rays will soon follow them. Before Medicare, the center of care was found near the high-rent districts of cities. In London it was Harley Street, in Philadelphia it was Spruce Street. As reimbursement changed, it shifted toward the hospital campus, where the parking problem is also solved. Nowadays, early discharge and reimbursement shifts have made it unattractive for a primary care physician to visit his patients in the hospital, so hospitalist and emergency room specialties are flourishing, with computerization feebly bridging interruptions to the continuity of care. The primary care physician would find the retirement village solves the parking problem; pharmacies and laboratory pick-up are often already in place, and non-surgical specialists would soon follow primary care physicians. Patient transportation, at present crippled by expensive municipal monopolies, would be greatly eased by such shifts of medical interaction. The ultimate shift of the center of care would be for the more mobile younger population of suburbs to shift allegiances toward the retirement village location, a change mostly affecting pediatricians. It would take some time, and it would always be a partial migration. However, the infirmaries of retirement villages offer convenience and comfort near home.
The most effective force maintaining standards for this level of care, have no doubt of it, is the ease with which friends within the community drop in for visits. They have time for it, especially to and from the dining room, and all of them keep a watchful eye on how they would likely be treated there themselves when their turn comes. In retirement communities, client consensus is a powerful force. What is lacking is a willing sharing of reimbursement with acute care hospitals. Therefore, the idea of brief hospitalization followed by longer recovery near home is now only realistically available to the affluent. But their choices show the way, as they always did before third-party insurance dominated the scene. For a while, little children may think it is funny to get their shots at the old folks home, but they will soon get over it.
Migrating to Retirement Villages

|
| Retirement Villages |
Institutions choose their locations for their own reasons, chief among which is cheap land, but the location near public transportation is another factor. They want to be near a source of employees but they also want to have cheap construction costs. Quite obviously, they are responding to cost pressures. Whatever the thought process underlying it, nursing homes and retirement villages usually get built in the far suburbs, often near the end of a public transportation route. A resulting problem is a vexing difficulty for a center-city hospital to find a nearby nursing home for convalescents. In time, suburbs grow up around these new institutions. A frequent consequence is a community of elderly people who need bus service to the doctor, surrounded by a community of young parents who must chauffeur their children to the doctor downtown. In typical American fashion, it eventually straightens itself out, but only after a lot of unnecessary inconvenience.
What is proposed here is that ways be found to encourage doctors to establish their offices on the campus of retirement villages. Doctors certainly like the idea of being near a cluster of people who see doctors a lot, while old folks like the idea of putting on a bathrobe and walking to the doctor's office. It would be hard to entice surgeons to locate anywhere except close to the hospital where they operate, so the natural first movers would be internists, geriatricians, pediatricians. If enough of them locate somewhere, a laboratory, pharmacy, and an x-ray department are sure to follow quickly.
That initial medical cluster would be enough to attract the local townspeople since there is almost always a surplus of parking space. The rehabilitation and physiotherapy units which are often already in place would get more activity, and the doctors would make rounds among their patients in a somewhat expanded infirmary. A regular jitney bus service would take people to one or more hospitals for surgery and major illnesses. In time, the center of medical care would move away from hospital office buildings, out into the suburban community. Acute care hospitals might not welcome the concept, but they would enjoy higher income from filling their beds with greater intensity of care, and the reduced costs of somewhat constraining their scope of service. Medical care would be more diffusely distributed within a metropolitan region, which is generally a good thing, and educational interaction with other doctors would grow, but in different locations. Almost all of these changes should tend to reduce costs and improve productivity.
The simplest definition of the center of care is not the medical center but the location of primary physician offices and the most important step would be to discourage contractual links between referring physicians and a specific acute care hospital. Doctors left to themselves will locate offices where the patients are, and increasingly it is possible to see a shift of patients requiring chronic disease management and terminal care, into the retirement village. The tendency of doctors and laboratories to cluster around hospitals impedes this more natural shifting together. If doctors shift their offices and are allowed a choice, laboratories and x-rays will soon follow them. Before Medicare, the center of care was found near the high-rent districts of cities. In London it was Harley Street, in Philadelphia it was Spruce Street. As reimbursement changed, it shifted toward the hospital campus, where the parking problem is also solved. Nowadays, early discharge and reimbursement shifts have made it unattractive for a primary care physician to visit his patients in the hospital, so hospitalist and emergency room specialties are flourishing, with computerization feebly bridging interruptions to the continuity of care. The primary care physician would find the retirement village also solves the parking problem; pharmacies and laboratory pick-up are often already in place, and non-surgical specialists would soon follow primary care physicians. Patient transportation, at present crippled by expensive municipal monopolies, would be greatly eased by such shifts of medical interaction. Moreover, expanded infirmaries of retirement villages offer convenience and comfort near home.
As for the effect on the retirement community itself, the most effective force elevating standards for nursing care, have no doubt of it, is the ease with which friends within the community drop in for visits. They have time for it, especially to and from the dining room, and all of them keep a watchful eye on how they would likely be treated there themselves when their turn comes. In retirement communities, client consensus is a powerful force. What is lacking is a willing sharing of reimbursement with acute care hospitals. Therefore, the idea of brief hospitalization followed by longer recovery near home is now only realistically available to the affluent. But the choices of those who can afford them show the way, as they always did before third-party insurance dominated the scene. For a while, little children may think it is funny to get their shots at the old folks home, but they will soon get over it.
It's harder to say what the effect on teaching hospitals would be. No doubt an unfortunate amount of isolation already exists between town and gown, which the profession at large tends to blame on the Ivory Tower pulling up its skirts. But anyone who attends conferences at teaching hospitals would have to admit that attendance is already very sparse, sometimes no more than five graduate physicians in attendance out of a faculty member of several hundred. It is likely the main factor at work is an excessive workload, forcing doctors to sacrifice new knowledge for the sake of using somewhat older knowledge in every spare moment. Generally, continuing medical education has moved to several-day national conferences, out of town. The teaching may be better, but it is uncertain whether the learning is as good as it was when teaching was local and informal. The teachers at teaching hospitals may despair at losing what little audience they have, but they must look elsewhere for a cure.
In any event, while Society has a legitimate interest in preserving the quality of care, it does not fulfill that duty by transferring it to reimbursement agencies. During wars, surgery is satisfactorily performed in tents, for an extreme example of how expendable much oversight can be. Another principle would be to ease impediments to overlaps of functions between institutions, particularly including the backward sharing of component services and records toward the lower-level institution. Since such sharing is often observed to occur without objection within vertically integrated institutions, there is every indication it is both desirable and feasible between competitors.
And finally, if this shift of locale seems so desirable, why hasn't it happened already? Some of the answers to that are the prestige of associating with teaching hospitals, which is well deserved. Some of it is inertia and given enough time much of it will happen by itself. But to whatever extent it lies in archaic regulations, protected by those who see themselves as injured by competition, it needs some leadership to change it. And the likeliest bastions of power to resist such change without being noticed, reside in the habits and rules of third-party reimbursement.
Unfair Income Tax Incentives
Now that health insurance has been mandated for everyone, it is an unnecessary irritant that some taxpayers will escape income tax for the amount of their premiums, while others will not, all based on what type of employer they have. While this inequity has been present for a long time, it necessarily changes character when the purchase of universal health insurance becomes a legal requirement. It looks as though some self-employed person will have to take this case of unequal justice under the law, all the way to the U.S. Supreme Court; and it is pretty hard to imagine arguments that would defeat the case.
This particular feature of our national health insurance muddle is now nearly seventy-five years old. It shows no sign of improving, although its solution would be very simple. The story of how Henry Kaiser during World War II enticed steelworkers to his California factories by evading wage and price controls is completely documented, widely understood, thoroughly deplored -- and seemingly impossible to change. When a book called The Decline and Fall of the American Empire is eventually written by a new Edward Gibbon, this situation might well be cited as an example of the inability of Americans to govern themselves.

|
| Henry Kaiser |
For those too young to remember, Kaiser was given a temporary exception to wartime wage and price controls by the War Production Board. He could buy health insurance for his employees, using his gift to entice East Coast steelworkers to move to his California shipyards. His company naturally took a tax deduction itself for the business expense, but somehow it was considered a forgivable ruse to skip withholding taxes for this virtual salary increase, and ultimately to skip income taxes entirely on this "fringe benefit". The maneuver was quickly copied throughout American industry. Although an attempt was made after the war to bring this legalized tax evasion to a halt, Congress discovered one political party supported Union labor, the other political party supported big business, and both of them urged the government to continue the contrivance against the rest of the public. Meanwhile, the war was over, but self-employed or unemployed citizens who asked to share it were denied the same right. Effectively, wages had been made higher for employees of large corporations than for the rest of the country, labor costs were made lower for their employers, and the arrangement was continued after the War had ended. Over the course of seventy subsequent years, there has never been a successful attempt to correct this inequity, which is turned back by the bellicose stance of organized labor to stand by its principle of never giving up any benefit, once it has achieved it. Management is generally more cheerful in defending this anomaly, but no less grim in its determination to retain it. Each of these combatants is happy to have the other side lead the fight and take the blame, but their positions are identical. Their true feelings are displayed in establishing a threshold limit of 7.5% of gross income for the tax deductibility of health care costs for everybody else. When the matter was last debated in Congress, the threshold was defiantly raised to 10%.
|
| US War Production Board |
The importance of the resulting inequity cannot be exaggerated. Subsequent enlargement of this tax beachhead into pensions and related fringe benefits has achieved a rough average of 35% of salaried income in big business, reinforcing the determination to protect it. However, this is probably not the way Big Business primarily looks at it. America has worked itself into a 60% combined state and federal income tax on corporations, consequently driving many corporations to relocate headquarters in countries like Ireland, with 12.5% tax. The Henry Kaiser tax abatement reduces employee costs about 15%, or well over a thousand dollars per employee. Since major employers have thousands of employees, the reduction of their costs brings an aggregate tax abatement to the employer in the many millions. The resistance of large employers to eliminating the Henry Kaiser tax abatement has many sources, but this looks to be the important one, by itself quite sufficient to convince almost any Board of Directors to acquiesce.
And thus, to sustain the employer-based model for health insurance in spite of its Job-lock implications. Congress sees it as too expensive to extend the same tax preference to those who are excluded, and too politically dangerous to take it away from those who have it. In a sense, Congress has a conflict of interest, because it reduces the effective cost of government employees. Two solutions are obviously quite simple: give the deduction to everyone, or else take it away from everyone. Meanwhile, this fraternity of tax-avoiders makes it virtually impossible for big corporations to get out of the employee health insurance business, encourages unhealthy fraternization between Human Resources executives and health insurance salesmen, raises the premiums of health insurance by roughly 30% for those who can least afford that cost, and supports the outlandish incomes of health insurance executives, once they have disposed of their inconvenient non-profit status. It cannot even be said that closing this tax inequity is a side benefit of mandatory insurance since it seems to have survived the enactment of Obamacare.
However, recognition of corporate income tax effects on "inversion", puts the matter as one of national interest in reducing the incentive for major corporations to move abroad, which would be a decisive argument almost anywhere but in a violently divided Congress. One would not blame Congress for studying the other unintended side effects of lowering corporate taxes one way or another, even though they have slid gradually into this situation over seventy years. Nor could one much blame the corporate CEOs from deciding to keep quiet about an issue so much in their present favor. But this is an election-deciding issue under certain circumstances, and it will be no respecter of persons if some candidate decides to make an issue of it.
Since the elimination of tax "loopholes" has become one of the foundations of other proposed tax reforms, there was some hope this parallel reform movement might overlap with healthcare insurance reform, since the "loophole" was really created for circumstances which have long disappeared. Many of the surprising quirks of the health insurance system today can be traced to Henry Kaiser's little scheme of the 1940's. And many quirks would probably inexplicably disappear if this particular tax situation reverted to something equitable. For instance, if you are looking for the explanation for strange behavior by employees, it is called "Job lock", and it is a creature of this tax law. If you lose your job, you lose your health insurance, and if you choose the wrong sort of new employer, you lose the tax deduction. Health insurance remains a one-year term system, and therefore scarcely anyone can envision the potential for permanent lifetime insurance, with internally compounded interest income, such as is seen in whole life insurance. To understand the consequences, just imagine being told you would lose your life insurance if you changed jobs.
The Resentfulness of Rejected Benefactors

|
Employer-based health insurance can be viewed as a lingering vestige of feudalism, or maybe Federalism. Employer-basing evokes images of the mansion on the hill, overlooking the factory and a little village of workers, allowing an eternal debt to the entrepreneur in the mansion who risked life and fortune to make the industry flourish. When a worker in the factory was injured, it really was the duty of the owner to see he was cared for. In fact, about 25% of major businesses are still controlled by the founding family, where notions of paternalism are taken more seriously. At least one mutual fund even specializes in family-owned and controlled businesses and can demonstrate that such attitudes really are an important asset. Unions, of course, sneer at such nonsense, while the owner-entrepreneur, in turn, reacts with fury at the implicit ingratitude. The Roebling family (of the Roebling Steel Company, builders of the Brooklyn Bridge, etc.) is famous for an epic performance with its company town, and there are a thousand such tales, starting with George Washington and his plantation. Although it is now difficult to see the slightest trace of feudal beginnings in the present administration of Blue Cross and other health insurance corporations, benign feudalism was in fact the foundation stone for employer-based health insurance.
And while most of them would deny it, it accounts for some of the vigor with which union leaders insinuate themselves into the board rooms of the present successor health insurance corporations, like schoolboys sitting on a vacant throne. It would go too far to describe the seventy-year struggle for national health care as entirely based on these primeval victories, but something does remain of that idea. In the 1920s, the big problem was to get people to buy health insurance. Civic-minded employers played such a leading early role in promoting this distinctively American solution it was often called an employer-based system. Dominating hospital boards of trustees, businessmen exerted peer pressure to spread the health insurance message. It became the right thing to do if you wanted to be regarded as the right sort, yourself. Even today, healthcare in many cities would suffer considerably if employers suddenly withdrew support.
In their civic role as hospital trustees, businessmen also recognized early that employer insurance mainly eased the cost load for the working population, and became less comfortable for outsiders, while insurer management increasingly recognized employer groups were the most profitable clients. Some of this was the inevitable tendency of all large customers to be more demanding of better treatment and to get it. This recognition became more apparent in scarcely two generations, as workers emerged as the healthiest, least expensive segment of our population. As a consequence, more assertive employer representatives professed uneasiness about employee premiums cross-subsidizing the rest of the population, even though it was always obvious that people with an income are the only ones available to help people without income. There was thus stubborn resistance to the idea that the main function of health insurance was to act as a transfer agent of health costs between age groups, unfortunately without a written contract to do so. There was then a period when the expedient was imagined that employed persons supporting their dependents, children and elderly parents, might cover the need more or less adequately. Eventually, government programs for the elderly and for the poor were recognized to be absolutely essential additions; by 1965, we had Medicare and Medicaid. Taxes were just a redistribution system on a larger scale, but Lyndon Johnson was in a hurry and those Great Society programs went unclarified as potential equivalents for the same goal: working people recycling funds for non-working ones. Unfortunately, 1965 was about the time the American post-war international trade balance turned negative, eventually forcing a recognition that the "pay as you go" financing systems designed for Medicare and Medicaid would be unsustainable until our trade balance turns positive again, which could be the same as saying "forever".
 Current premiums (mostly from healthy people) are used to pay current costs (mostly generated by older, sicker people) on the assumption that new young subscribers will always outnumber sick older ones. Not a safe assumption. 
|
Even benevolent employers had to worry that our international competitiveness could not withstand the strain of it. Although most citizens, businessmen or not, probably did not understand why it was true, attempting to lower worker health costs through Managed Care HMOs proved to be a self-defeating disaster, combining worker antagonism with further upward-leveraging of employee premiums to support it; even so, it never addressed the underlying basis of the problem. Reform of hospital cost-shifting against employee groups was equally futile, as described in later paragraphs because such pushing on the balloon caused it to bulge out among the uninsured, who mostly transformed it into bad debts for the hospital. Unfortunately, cost-shifting which in 2008 generated a proposed solution as dumping the system's growing medical expenses on the backs of those with high premiums but low usage, became translated into a shift onto the backs of those who could not even afford their own costs. It violated the long-established tradition that those with the highest medical costs should pay the highest premiums, without proposing a way to make it politically acceptable. It must be evident that the solution supported here is a benevolent return to the concept of "Each ship on its own bottom," because of alarming signs of class warfare in the concept that one group must support another group against its will. The general concept here advanced as a more palatable substitute is individual lifetime insurance. A short-term concession would be to call for modified individual lifetime policies as a transition step. The success of even this proposal must frankly depend on the hope that interest rates will return to normal, and that cures for cancer and Alzheimer's disease are on some future scientist's horizon. No solution to this problem should be presented as free of problems, but it is equally unproductive to throw things against a wall, just to see what sticks.
 To repeat an inconvenient truth: "service benefits" means cost is not a responsibility of the patient or his employer. It has been transferred to the hospital and the insurance company to "work it out", which they mainly do by raising prices or shifting them to outsiders. 
|
 Many problems will prove to be non-problems, while unanticipated problems are inevitable. 
|
 Obamacare designers probably expected most of its problems to come from small business; they seem to have forgotten about ERISA, which presents some health insurance alternatives. Taking nearly a decade to design, ERISA is likely to withstand most attempts to change it. 
|
The mundane but ultimate downside of employer involvement is that top management of major companies seldom give healthcare a high enough priority on their time, thus allowing unions and human resources departments (their philosophical successors on the company payroll), to speak for the company in important forums, with the effect of appreciably softening price concerns. When top management was again drawn into a visible role by the Managed Care ("HMO") fiasco, the business-school approach did not distinguish itself, so government and academia have become less deferential, perhaps even hostile, to business. The final word on the role of employers in the transformation of an employer-based system by the Affordable Care Act has yet to emerge. Much will depend on how gracefully the transition is managed.
Evolving Employer Attitudes About Employee Privacy

|
| Health Insurance is Everyone's Business |
Employer-based Health Insurance. From an employer's viewpoint, a sick employee is an expensive employee, but there are special employer twists to employee illness. The most effective comment a former employer can volunteer in a letter of recommendation is to say that over several years, the employee was "never late and never missed a day of work". It's hard to predict medical costs in advance, but the identification of someone as "accident prone" is the kiss of death for hiring or promotion, because the difference between a devastating injury and a trivial one, is about half an inch. Disabled persons are identified as being unable to do the job, and may include less visible issues, such as being so attached to local health providers they become unwilling to accept a transfer to another city. Some of this affects health insurance premiums, some may not. But the large employers are largely self-insured, so they have more access to individual health cost information, and can longitudinally assess whether their Human Resources departments are doing what is vaguely stated to be a "good job." Some of this is no more than shrewd selection of an agent for administrative services-only. Large self-insured employers almost always have lower health insurance costs, which in the aggregate is likely to mean healthier employees, the cream of the crop.
New or small businesses generally do not have a large enough employee group to justify basing next year's budget on last year's health cost experience. So "small group" insurance tends to reflect the overall higher costs of small-group employees in the whole geographic region, and "individual policies" are the most expensive of all, because they generally have a good idea what they need and want in an insurance policy -- and seek it out. Add to that factor the preferential enjoyment of tax exemption, and the system has gravitated into one which could not have been designed by experts to be so preferential to certain types of business models.
 For the sake of economy of effort, let's first see what we can do about portability and privacy, indirectly, by getting rid of the tax preference. 
|
Participants in sports where a great deal of betting goes on about game outcomes and career records have good reason to fear careless gossip about injuries, illicit drug use or even cataracts. Aging actresses fear their younger competition; almost everyone is uncomfortable about addictions and deviant behavior. The decline of primogeniture and the rise of antibiotics have even undermined the devastating consequences of suspicions about true paternity. Whether the resulting business models are going to lead to a decline in concern about patient privacy in any forum, could well be argued at length. What's more likely is that most people will tire of the subject.
Nevertheless, no one can dispute that employees in a favorable health insurance arrangement are quite reasonably reluctant to change employment to a situation which loses them a tax deduction on 30% of their salaries. The situation is called "Job lock". Portability is a real problem, while privacy is much less consequential, except to some very vocal groups. Even though it seems unrelated, the manifestly unfair design of this tax preference is one of the reasons American politics have become so restless about seemingly unrelated matters. The freedom to go somewhere else has become impaired. For the sake of economy of effort, let's first see what we can do about portability and privacy, indirectly, by getting rid of the tax preference.
Correcting the Co-insurance Blunder
In this chapter we are discussing health insurance problems which the Affordable Care Act did not create, and for which its only blame is that it neglected to address them. The implication must be that a better health care reform bill would indeed address them, or at least give the public the impression that it considered the problems and for sufficient reason had to pass them by. It highlights one more important reason why this book hopes to generate the creation of a Grand Strategy rather than specific legislation.
The Blunder of Co-payment. Let's state that co-insurance sounds like a deductible but isn't, has shown very little deterrence value at its customary 20% level, creates the market for an extra insurance policy, and would never be missed if eliminated in its traditional form. A deductible, by contrast, is a single lump sum imposed at the beginning of an expense period, a so-called "Front-end deductible", whereas co-insurance imposes a sort of tax on every service, ie. a "20% co-pay". Examples: a deductible would be the first five thousand on a twenty-thousand dollar cost, per episode, or per year, and it does not change with the size of the bill. A 20% co-pay, or co-insurance, takes 20% of every charge. As the Affordable Care Act begins implementation, it is reported that the ACA plans to introduce 30%, 40%, and 60% co-payments through its insurance exchanges, in addition to a $5000 deductible, and in addition to tripling the premium. The matter merits considerable discussion, and it will probably receive it but details are presently very scanty. For example, there is already a flourishing market for 20% copay insurance which pays for nothing else, so the insurance companies will enjoy this feature of Obamacare which stimulates twice as many insurances. Congress would find a large co-payment enjoyable, since a 30% copay means the patient somehow pays at least 30% of its cost, out of his own pocket. These are also the numbers which get the businessman's attention in employer-based insurance. They appeared in a two-line notice in the New York Times, just before the Fourth of July holiday, and only chief financial officers have a lot of information about it. That sounds like a trial balloon which could soon be revised, but possibly not. If this is the final word, it will certainly imply the Administration is desperate to find reductions in the cost of the program. Put it in context: premium prices are doubled, a $5000 front-end deductible is imposed, a minimum of 30% of the program eventually lodges in copayment insurance which the patient must himself pay. On top of that, the only reliable evidence for what is going on comes from Chief Financial Officers, who as a group are the most hostile to the program because it involves them in myriads of complexities having nothing to do with their corporation's core business.
The position of this paper is that copayments should be scheduled to be eliminated entirely, but deductibles raised as high as possible, at least to $5000. This is not a small technical issue. Deductibles have proven effectiveness, while co-pay shows no effect on consumer behavior at the traditional 20% level. It is impractical to extend either approach to patients sick enough to deserve hospitalization as an inpatient because a growing proportion of "patient responsibility" charges reappear as bad debts. Alternatively, to raise office and outpatient price levels much above the minimum cost of hospitalization is not only unrelated but futile. It creates a substantial incentive to admit patients to the hospital in borderline cases, especially from emergency rooms and captive satellite clinics, recently enlarged to take advantage of artificially low-interest rates. Hospital administrators already complain that unpaid co-insurance is their biggest financial drain. The fact is, co-payments have already approached a practical upper limit, without any sign of affecting patient attitudes. Unpaid patient coinsurance is a sensitive indicator of dissatisfaction; there should be more feedback about it between the hospital and accrediting agencies. Since most insurance has a deductible less than $5000, there is probably some room left to increase deductibles, but public outcry can be expected unless something like a Health Savings Account is provided to ease the pain. Insurance companies will rush to be first with a new and improved "supplemental policy", another expensive blot on the landscape, designed to eliminate cost consciousness on the part of those who can afford it. The contradictory message sent by supplemental insurance is that reducing patient cost consciousness is a good thing.
A much better inpatient solution is available in the DRG system, even though it could use some improvement. And there is the potential of using credit cards attached to Health Savings Accounts as a source of data for improving DRG (Diagnosis-Related Groups) by capturing outpatient market costs and using them for market-based hospital cost accounting rather than hospital cost reports, which contain massive distortions from several levels of cost-shifting. Patient cost sharing, in general, is already approaching its limits and cannot be relied upon to produce the order of savings suggested by 50% co-pay. Other, more sophisticated, approaches are needed. To become convinced of this, it helps to understand its history and politics.
 The way to cut hospital costs is to cut the indirect overhead costs. 
|
Doesn't all that make it sound more attractive to look for new sources of revenue? The traditional sources are pretty well exhausted.
Hospitals' Ratio of Charges to Actual Costs

|
| Apple vs. Apple Corp |
Recently it was announced that Apple Corp., the largest corporation in the world, enjoys a 50% profit margin. By contrast, an American hospital seldom makes more than a 5% profit, and many lose money. Even at both extremes, individual products have differing ratios of individual prices to individual costs. Only in the aggregate do they produce a company-wide profit of 50% and 5%, respectively. It is on this aggregate profit and loss that the company is judged, its officers promoted, dividends declared for the stockholders, taxes get assessed, and the value of the company measured by the stock market.
A for-profit company is judged by its profitability, and while most hospitals are run as not-for-profit organizations, the accounting convention for nonprofits is to judge "profitability" by the annual increase (or decrease) in its net assets, essentially the same thing as profits and losses. It is not necessary to examine the little quirks introduced by such things as the ownership of fine art. While a not-for-profit corporation is judged by its profitability rather than its profits, that's also really the same thing. It has been said that fewer than a thousand people in America understand nonprofit accounting, and while it is an important subject, it is just not the one we are discussing.
It is also important for even a layman to understand that government accounting while resembling nonprofit accounting, differs in one important feature: departmental accounting regards money from the general taxpayer fund as an asset, not a liability. Therefore, what we would normally regard as a loss for a government department has two components: any reduction in its assets, and any money from general taxpayer funds. The sum of the two is the loss from operations, and in the case of Medicare, it is about $550 billion a year, plus the decline in assets (in the Medicare Reserve Fund) of another $19 billion. Thus, if Medicare were a business, it would be said it lost $569 billion a year, or about half of its expenditures. If a nonprofit hospital were considered with the same numbers, it would be said to have lost $19 billion, because it has no transfers from general tax revenues.
The only present point is that it is difficult to discuss hospital economics in anything but the same aggregate form which is natural to for-profit entities, so you must look to the increase or decrease in its assets instead of profit and loss. If that premise is accepted, it must also be accepted that internal cost-shifting is not merely a permissible but an essential feature of their accounting. There are no dividends to dispose of excess profits; excess profits must be transferred somewhere and justify the costs of something else. Sometimes, just sometimes, a large vaporous cloud called "indirect overhead" floats around justifying expenditures. And weakening price resistance to them, so it's doubly important to concentrate on indirect costs. Triple, because the accountant has very little idea of the relevance of the indirect cost to the main business of the organization, which in this case is medical care. As soon as you start calling it healthcare, its relevance is even more difficult to define.
 A large vaporous cloud called "indirect overhead" floats around justifying expenditures. And weakening price resistance to them. 
|
It is disconcerting to consider that the Affordable Care Act may have upset a minute of healthcare regulations, originally finely balanced on the need to run a hospital with reasonable business latitude. After all, it is impossible to follow society's mission if a hospital cannot itself determine some indirect costs. Once a hospital reaches even moderate size of two hundred beds, almost any product of a hardware store, department store, or supermarket could plausibly be required to run it. Business supplies, school supplies, parking, and building maintenance are required, as are architects, lawyers, and electricians. Once you go down this list, you might constrain approval to buy supplies and equipment that sound as though they belong in a hospital, but one hospital reported its largest single expense was heating oil, closely followed by ice cream. Somehow, every item must be connected in some way to a service which can be charged for, which is an accountant's trick for establishing what is a legitimate expense. Sometimes this is pretty hard to do; a hospital needs a hammer, but how do you assign the cost of the hammer to some item which is legitimately charged for? It soon becomes evident that the assignment of indirect costs is always going to be a little questionable, but always absolutely essential. In the early days of hospital cost accounting, it was reasonable to aggregate the indirect costs of each department and assign them to the direct costs of that department.
From this evolves the concept of a cost-to-charge ratio. Reasonable uniformity in the ratio of charges to costs within departments, or between various departments, assures that cross-subsidy between insurance companies and patient classes is fairly uniform. Without that check, complaints between competitors would be immediate. Essentially, this sort of system depends on equal justice being applied, at least in a general sense. When equal justice is impossible, the accounting department can only rely on intuition and overall balance. Outside regulatory agencies can compare the cost/charge ratio in one hospital's operating room with that of some comparable institution. The first step in such comparisons is to compare the institution-wide ratio with its peer group. If that doesn't produce a reasonable result, the analysis can go down to individual departments to individual tests and procedures, until the source of a wide discrepancy can be isolated. At that point, questions can be asked, and a reasonable conclusion reached. But that was forty years ago. When charges are submitted for an electrocardiogram totaling several hundred dollars, and drugs at several times the retail price in a neighboring pharmacy, this sort of analysis is fruitless because it leads to ridiculous results. It is time to agree that a reasonable pattern of only direct costs can be typically and quickly laid out. On the whole, it can be judged that it is indirect costs which become very hard to follow by the usual step-down process. Therefore, it seems reasonable to pass over direct costs quickly, and go straight to the indirect costs, judging them on their separate merits. Apparently, It really does not matter what charge they have been assigned to; what matters is whether they are legitimate. Outliers can be dealt with individually. What is important is for community representatives to assess, is whether the bulk of general overhead costs can be justified for a community, whether the bulk of CEO salaries suits community expectations, or whether landscaping costs unsettle community opinion.
 The main reason for having health insurance is to protect yourself from being fleeced. 
|
| Jonathan E. Rhoads, M.D. |
Unfortunately, it is just this sort of needed commentary which is most questionable on a constitutional or political science level. It is not at all certain that consumer groups or third-party insurance groups have a right to be dictating salary levels, or whether an institution needs a new HVAC system. It is far from clear that a government of limited federal powers has any right at all to be dictating local hospital indirect expenditures. When Medicare was only one of several dominant payers in a hospital, they did acquire a sort of legitimacy when they insisted on equal treatment with other payers. Now that Federal Laws of uncertain shape, mandate universal coverage of uncertain form, it becomes legitimate to ask whether the format of filling in the coverage gaps can stretch the Constitution into assuming the total administrative control which the Constitution seems to prohibit. As these new regulations get actual implementation, more and more people will acquire "standing" by sustaining a provable personal injury. It remains to be seen, where that will lead.
Utilization Review
When medical care was entirely a private two-party arrangement, the patient and doctor negotiated what was to be done, and often the price; if the patient could not pay, some embarrassed workaround was figured into the equation, including a vague promise to pay the doctor when he could. A surprising number of patients did pay later, and because the doctor's bill contained very little overhead, even partially paying it off created an unspoken promise that the patient would now be welcomed back.
It was the appearance of insurance forms which created secretarial overhead, even though of course it also brought along some revenue. Skeptics may doubt the extent of this, but at my advanced age as a patient I now visit four doctors of different specialties. Collectively, they seem to have fourteen assistants and fourteen computers I can count. That remains the situation even if a patient delegates decision-making to members of the family, or a hospital wants to know what is being given away to charity patients, or a bewildered patient seeks a second opinion. It changed abruptly when third-party payment seemed to entitle a government or an insurance company to be reassured that claims were legitimate. This uneasy and often resented intrusion into a private matter began to cause friction even in the 1920s, soon after third-party reimbursement made an American appearance, and as physicians gradually recognized that "utilization review" generated more overhead cost than simple claims submission. At first, health insurance companies were restrained from brisk business-like behavior, by the realistic possibility that the patient might switch back to paying bills in cash. Somehow that possibility now seems so remote that when the owner of a Korean auto manufacturing company tried to pay his hospital bill with hundred-dollar bills, the hospital simply had no procedure for handling such an unexpected request.
As long as a secretary was sitting there filling out forms, she might as well answer the phone for appointments. In this way, appointment systems became routine, including hidden extra revenue loss generated by broken appointments. Insurance pre-payment is always complicated by the realities of emergency care, where considerable expense must sometimes be incurred before the third-party has a chance to review the facts; in this lies the origin of the term "reimbursement". The third-party acquired the ability de facto to delay or deny reimbursement, an action immediately regarded as high-handed, since expenditures had already been made in good faith and could not be recovered. The right to deny such claims was implicit, and at first it was used gingerly by insurance companies trying to establish themselves. Now that insurance is considered normal, any incurred costs must be handled in some way, so other subscribers are charged extra to keep the hospital solvent. The cost to the system is exactly the same this way, but no other way has been suggested to maintain the credibility of insurance oversight. When I once told the owner of a department store that I had 2% bad debts in 1955 (ten years before Medicare) he replied that my bad debts were less than his and my bookkeeping was far more elaborate. True, some hospitals could not survive without the insurance system, but if others in better locations examined their experience extensively, they might discover their accident rooms are net losers for the insurance. Third-parties slowly retreated, hospital prices crept upward and the system readjusted, but no one is entirely satisfied with this showmanship masquerading as a balance of terror. When you see a sick or injured person turned away from an emergency department for lack of insurance proof, you can be sure there is either not enough slack in the system, or not enough administrative imagination.

|
| Senator Wallace Bennett |
Early in the 1970s, Senator Wallace Bennett of Utah devised a solution to this problem, and persuaded the rest of Congress to endorse a nation-wide system of Professional Review Organizations (PSRO), run by the medical profession but paid for by Medicare. Although many physicians muttered about the "creation of new elites", and hospitals were particularly uneasy about the migration of power, the new system worked reasonably well. If the physicians in the local PSRO approved a service, it was paid for. If payment was denied by a local PSRO, an appeal to a state-wide body of physicians was provided. In that way, prevailing local standards were respected, while appeal to distant physician judges was also provided, to guard against local vendettas ganging up on someone they disliked. Inevitably, a few localities would elect an unsatisfactory PSRO, so a voluntary national organization was formed to educate, inform and defend the process, and better able to discipline it with peer pressure than might be supposed. The national organization was pleasingly benevolent, sometimes apologizing for its role as a necessary one to weed out constituent PSROs whose bad behavior might discredit the others and start up the usual chatter about professional self-government: The foxes were guarding the hen house, and must be replaced by wolves. The PSRO gradually adhered to an unspoken rule of rarely boasting of success; it saw its role as redirecting unsatisfactory behavior, not vanquishing wrong-doers. It soon became evident that successful PSROs were of two types, rural and urban. In localities where a single hospital served a county or more, physicians were of all types mixed together, and the need was to strengthen the emergence of the natural leaders, often by placing them on the PSRO board. In large cities, however, a sorting-out process had usually resulted in strong hospitals and weak ones; birds of a feather flew together. The weaker hospitals were soon identified and urged to elect stronger leadership; sometimes it was necessary to suggest that the institution might serve better as a nursing home. Throughout the process ran the threat of exposure; successful PSROs usually relied far more on peer pressure than the threat of withholding payment.
What ultimately defeated the PSRO was its success, not its failures. Many pre-existing elites were content to see a new governance structure fumble, but felt highly threatened by a successful one. Moreover, the AMA leadership seemed particularly concerned about the direction of "regulatory capture", and was not completely certain whether the PSRO was beginning to dominate the Washington bureaucracy, or the AMA House of Delegates, or a little of both. The PSRO fraternity was definitely a large national organization of doctors who knew and respected each other, and many of its leaders were in the AMA House. Matters finally came to a head in a famous vote opposing the PSRO, by 105 to 100. The opinion of organized medicine meant a great deal to Congress. When representatives of the PSRO next testified before the Senate Finance Committee, the Chairman of the Committee wryly announced the next speaker from the AMA was one who was "presumably here to explain to us the difference between 105 and 100." The PSRO law was soon amended, and insurance review took its place.
|
| AMA House of Delegates |
For the time being, utilization review in the future is apparently currently limited to Medicare, under the Medicare Accountable Care Act. With the foregoing bit of history to warn the Accountable Care Organizations about what they are getting into, a simple set of principles can be stated. Utilization review encounters two components of cost: the volume of care, and the price of the services. Doctors control the volume, hospital administrators control the prices. Determining the proper volume of services is a job for practicing physicians, alone and unhampered. To some extent, under the new law an incentive to keep it that way was created by sharing with the provider members a portion of any cost savings associated with the patient group. But the ability to change the sharing will probably be a a one-sided government decision unless the physicians fiercely insist that it remain negotiable. Agreeing that the physician voice should be dominant in the issue of service volume should not imply agreement to exclude their inspection of the prices of services. When physician income becomes linked to their choosing less expensive alternatives, physicians must not continue to be blinded to what the true cost of components truly is. While it remains conceded that hospitals and vendors must retain some flexibility in adjusting the ratio of charges to costs, any deviation from a standard bandwidth must be negotiated with the physicians affected. Past experience should be ample proof of the fairness of this demand.
The volume of most medical services at present is about right, but prices will keep rising when they bear little relation to the underlying direct costs. Furthermore, the Medicare (or similar) Cost Report of every hospital must annually report the ratio of cost to charges, probably by item rather than department. And this ratio must be monitored. Complexity is no argument against doing so; the Chargemaster system has never been resisted because of its complexity. It has been no secret for thirty years that a twenty-dollar aspirin tablet has a very high ratio of charges to its actual cost. Other items are provided at a loss, and the mixtures are highly variable between hospitals. Everyone concerned knows this situation is unsustainable, but everyone recognizes that total denial of reimbursement is entirely too destructive if no slack remains in the system. If it is successful an appeal mechanism will become necessary, because new treatments can be resisted by old treatments, but the optimum rate of change will vary by local situation.
Rather than overcomplicate matters, the goal should be total denial of reimbursement for denied services, because the public will demand it. It must however, be coupled with an adequate profit margin on approved services, to service the costs of retrospective review. Designation of the optimum ratio of cost to charges is a critical decision, much like the function entrusted to the Federal Reserve, of picking the best average interest rates for the national economy. If the agencies selected by Obamacare get this point very wrong, very often, the public must quickly be in a position to let everyone know of its displeasure.
The other source of circumvention is the hospital system of enforcing a physician hierarchy reporting to a physician chieftain, but insisting that the chieftain himself be financially beholden to the hospital administration. In that way, financial health of the institution sometimes dominates the health of the third parties, who then find a way to retaliate. if this issue is neglected a deadlock could affect the health of the patients. Since a three-way balance must be preserved, governance must be fairly shared three ways. Those who believe this is a minor issue because the third party obviously has final power, have a great deal to learn.
Loud and Clear: Health Savings Accounts
Health Savings Accounts. Medical Savings Accounts must be distinguished from Medical Spending Accounts, which unfortunately include an annual "use it or lose it" feature. These spending accounts recently styled themselves Flexible Spending Accounts, while Medical Savings Accounts became Health Savings Accounts. In time the confusion may subside, but the distinction remains important. There has recently been an employer initiative to make the payments of Spending Accounts tax-exempt, apparently intending to equalize them with Savings Accounts, but tip-toeing around the larger issue of failing to include individually purchased health insurance in the tax exemption.That would be an unfortunate splitting of political forces.
Health Saving Accounts (HSA), or Medical Savings Accounts (same thing) supplement other IRA (Individual Retirement Accounts) or 401 (k), but address medical expenses .
Tax-deductible, Health Savings Accounts do indeed accumulate unspent balances from year to year, gathering income for a future rainy day as they go, while allowing funds to be spent immediately if the rainy day comes early. If wisely invested and left untouched, they can accumulate a surprisingly large amount of money over a lifetime. They don't quite make everybody a millionaire but that isn't completely impossible if you don't get seriously sick, and pay small routine medical expenses in cash. Just why employer groups have failed to seek ways to convert their use-it-or-lose-it plans into Health Savings Accounts -- which wouldn't lose it -- is not entirely clear. But it is highly recommended that this be explored, if for no better reason than to put a stop to wasteful spending at the end of the year, just to use the money up. This book proposes to put that money to work pre-paying medical expenses in the far future with the investment income, which is a goal you would suppose is in the employer's interest. Almost enough has already been said here about this idea, so some attention needs to be devoted to those people who have HSA plans and do get sick, and can't afford their medical costs without invading the fund. If such a person does get sick, the money to pay for it is available. This feature responds to the fact that some people have major illness early in life, while some other people stay well for decades before they have a serious illness; for most people, it is a toss-up which it will be. It isn't very common for someone to be very sick for six decades, by the way, but stop-loss insurance would even cover this contingency, and it isn't very expensive because that sort of casualty is uncommon.
Because we all get tangled in this sickness lottery, the Health Savings Account is intended to be linked to a high-deductible health insurance policy. The higher the deductible, the cheaper the insurance premium will be, so progressively more money is left over to add to the Health Savings Account, compared with buying ordinary health insurance. At the moment, the best level of deductible is at least $5000, varying with inflation. The person who buys this package is on the hook for $5000 until the Health Savings Account builds up to $5000, which usually takes about three years. Those who don't already have that much savings or reserves are taking a chance for three years. That's one of several reasons why this package is most appropriate for young, healthy people.
These two linked promises are meant to discourage unwise spending, even for health, but it's your choice. What induces you to contribute annually, and discourages early withdrawal, is the income tax deduction. That's all there is to it, and it's already quite legal. From its very beginning, an HSA was intended to be linked to a high-deductible health insurance policy bought independently. The pre-funded last year of life was an afterthought for what you would do with the money if you enjoyed good health, and the accordion is provided just in case we get a cure for cancer, or some other wonderful development.
There are problems to be tinkered with. Nowadays, it usually goes the other way; the Health Savings Account is suggested and explained to customers by salesmen for high-deductible ("Catastrophic") health insurance, who could also suggest a bank with a debit card to make claims and payments both convenient and smoothly integrated, but often don't do so because there is no commission for added features. Brokers earn commissions on the insurance part, but not on the HSA part, and that's probably a flaw. Some brokers suggest the whole package, but pressuring individual banks to waive fees for maintaining them, is just asking too much. Providing for sales commissions might improve public adoption. Technically, that's all there is to HSA. The only known opponents to high-deductible insurance are a few labor unions who fought to pass state laws mandating specific small-expense items into all insurance policies in their state. Somehow they imagine circumventing those victories (by HSAs making them unnecessary) would diminish their own stature. In any event, these small-expense state mandates ought to be repealed or pre-empted. They eat into the fund which might need money later for a more serious sickness, and they inhibit the sales of high-deductible. Hospitals are very little affected by this approach, except in the reform of the ratio of charges to costs. Therefore, most of the external supervision of the program should come from physician representatives, who will be the first to notice when changes are needed.
The real value of Health Savings Accounts is not what they provide, but what they make possible. One immediate consequence is to silence knee-jerk objections to a high deductible. By implication, deductibles discourage the co-pay approach by competing with it for the premium dollar, and we have earlier discussed why that would be desirable. On first learning about HSA the first reaction of many people is that no matter how small the deductible is, some poor patients could not afford it. A high deductible sounds even worse. However, under the Affordable Care Act, everyone must now carry some form of health insurance, so a high deductible makes it cheaper to finance and to buy. For some poor people, a subsidy is required, so Constitutional equal justice is, so far, in doubt here. Health Savings Accounts merely aspire to receive equal subsidies for poor people compared with other insurance, but meanwhile, provide a tax-exempt incentive for working people to accumulate funds internally to cover a deductible. With HSAs, money to cover the deductible is in the fund after about three years, and sooner if it is subsidized. In any event, subsidies would mostly be temporary, because those who do not get sick would see annual increases in the Savings Account, soon making further subsidy unnecessary. Anyone with tight finances might be advised to start with the catastrophic insurance, adding the HSA component when they can, and resulting cost savings would not be negligible, even during the present episode of abnormally low-interest rates, because the contributions themselves are tax-deductible. The temptation to delay or deplete the fund should be resisted, particularly by governmental payers of last resort, because the expense is so likely to reappear as a bad debt when indigent patients get sick. Temporary front-end subsidies for HSA, while initially objectionable to conservatives, are a far better solution than the present unsustainable expedient of cost-shifting. The first function of a high deductible is to make insurance cheaper, in this case, cheaper than simply enrolling through an insurance exchange. Because of current low-interest rates, a few banks currently charge a small fee for debit cards with a low balance, but many banks do not. Young people are apt to incur small medical expenses, not covered by the high deductible, but they can all look forward to higher expenses when they will be glad they had set the money aside. Starting out with buying both features should squeeze major financial health risks permanently out of consideration after two or three years of good health. Existing health insurance companies may thoughtlessly resist such a change, but the impending startup turmoil about the Affordable Care Act should soften them up considerably.
Speaking of fairness, HSA finally catches up with the Henry Kaiser World War II provision (see above) by extending healthcare tax exemptions to all working people, not merely salaried employees. It now could readily match a temporary subsidy for the poor to whatever permanent subsidy the government provides under the Affordable Care Act, whenever that gets untangled from the conflicting provisions of ERISA. Those are decisions independent of insurance design; if Congress changes either the subsidy or the tax exemption, the insurance can adjust correspondingly. A future budget search for smaller subsidy costs would not cripple Health Savings Accounts, as it might well cripple Obamacare. A few conservatives are so antagonized by Obamacare they would not mind crippling it, but their long-run interests are better served by creating a more workable system. That point may not be obvious, revolving around the difference between indemnity and service benefits. An indemnity (or the patient) states in advance what is affordable and hopes to negotiate the rest, whereas a service benefit describes what services it will pay for, regardless of cost. If you were a healthcare provider, how do you suppose you would react to that proposal? Indemnity is designed for ambulatory adults to bargain with but is largely inappropriate for sicker people in a hospital bed. In the HSA system, the distinction between ambulatory and bedridden appears at the level a Health Savings Account stops paying, and the deductible health insurance starts paying. That is, it depends on a shrewd choice of the size of the deductible. For this reason, Health Savings Accounts have always attempted to match the size of the deductible to the average cost of fairly inexpensive hospital admission. And for this reason it should not be tinkered by other considerations; if the deductible is raised above the level of the median hospital entry, it should apply to a separate stop-loss policy for hospital outliers.
In a well-designed system using debit cards, a transition between the two types of treatment venue could almost be imperceptible, but that also creates a hazard of changing it carelessly. As mentioned, it is in the interest of everyone to maintain the amount of the deductible below the great majority of hospital inpatient bills, while remaining above the average annual cost of office care. If that is unachievable, only the hospitalization cost should be matched. To forestall gaming of the insurance by cost-shifting, hospital outpatient costs should be treated as office visits, and Emergency Room costs as well, provided the patient is not subsequently admitted.
The Health Savings Account is thus tax-exempt and accumulates from year to year, together with the interest it earns; its sources are a portion of wages, or tax credits, or possibly in time government subsidies, varying between individuals. To prevent gaming, expenditures might be limited to health care, but there is no earthly reason to limit contributions to a system which is starved for revenue. In practice, the account is used primarily to pay for outpatient (office) services; assuring the ability to pay the deductible of a linked catastrophic insurance policy is very important, but much less frequent. It is not contemplated that it will have any co-pay or coinsurance (see above). It also might contribute to an optional pool (or reinsurance) for the less frequent risk of paying for the second instance of an annual deductible, providing sufficient funds have not re-accumulated in the Savings Account. Its essential point is to distinguish between small negotiable costs and large unnegotiable ones, not between paying hospitals or doctors, as Medicare and others do. The internal accumulation of compound interest income matches another unspoken reality; young people have few medical costs and can accumulate, while older people are mostly spending. This somewhat answers the common grievance of young people that they are subsidizing old people; they are in fact subsidizing themselves for when they are the old ones. The degree to which unmentioned problems fall into place is a great testimony to a system whose most attractive feature is simplicity. In practice, it does employ an essentially different insurance methodology between most office doctors, and hospitals, and between most young and old. It just doesn't specify it.
Marketplace Presumptive Costs (MPC). Payment by diagnosis rather than itemized bills (beginning in 1982) was a great improvement for patients too sick to pay much attention to finances, which generally describes hospital patients who need to be there. Since Canadian hospitals demonstrated (by eliminating them) that itemized bills were the main information system for cost-effective management, they are still produced in American hospitals. Although such posted charges are largely useless because of the 500% disconnect between prices and their underlying cost, the volume of individual services is depicted accurately, and could be used to link marketplace prices (reported by aggregated regional Health Savings Accounts), to the item volume within the Diagnosis Related Groups (DRG), as well as the particular patient's item volume (his bill). The result would be a new cost figure not previously available, which we will here call the Marketplace Presumptive Cost (MPC). If that is added the unique surcharges for administration, teaching, charity, and research and development, the evaluation of what these costs are all about could be brought into the open. Compared with that step forward, the relatively trivial costs of wasted paper in bills-no-one-can understand, can be ignored. Until some such transition can be accomplished, itemized bills must not be abolished in the name of efficiency, or any other motive. With the MPC, doctors would finally have a meaningful speedometer to guide their cost decisions. No sentient doctor now pays the slightest attention to the hospital bill, because it reflects nothing approaching the true cost of the service or the true cost of individual physician performance. The underlying cause of this disconnect is the enormous amount of cost-shifting taking place, but a certain amount of cost-shifting is nevertheless essential to running a hospital. The issue is to detect when it has become excessive, without necessarily changing it. The present reliance on direct costs and the present rhetoric about posted charges are both futile. A cost-to-charges ratio is therefore doubly useless. The need is to examine indirect costs, make comparisons among competitors, and decide what is necessary, what is excessive. It's fairly clear in advance that will demand some definition to indirect costs.
The Clash between Mandatory Coverage and Marketplace Benchmarks. Insurance was never meant to be universal, and the closest thing to it, mandatory auto insurance in no-fault states, gives a widely familiar example of what happens when insurance is overextended; the insurance adjuster rules but prices go up anyway. At least in auto repair, an extended market for metal workers, painters, electricians, and mechanics exists to create some basis for argument. By contrast, if every patient carries insurance, how can the price of almost any service be determined? How about a new operation to transplant brains, or an ingenious repair of someone who fell off a cliff? How about a badly needed distinction in compensation between doing your first operation and doing your thousandth one? Or, just sitting at the bedside, comforting the dying. Everywhere you see a disturbance of the marketplace you see a disturbance in prices, and if prices are forcibly constrained, then candy bars well known to shrink in size. Eventually, shortages appear, as they recently have with generic drugs driven off-shore, creating a monopoly for irresponsible manufacturers. The only feasible way to retain a vigorous marketplace in health care costs is to allow the market free play under a large deductible. A sufficiently large co-pay might be thought to do it, but Gresham's Law shows it is impossible to maintain two prices for two halves of a service. Since many services performed in the hospital are also performed in doctor's offices, a considerable base for determining the price of DRGs (diagnosis-related groups) is readily established, and adjusted for local and regional differences. That will be automatic if the market is allowed to adjust to costs in nearby offices, and the necessary data links are created. A blood count is a blood count, an EKG is an EKG, whether inside the hospital or inside a tent. Hospital administrators complain they have high overhead, but that's just the point, isn't it? A high deductible is the only imaginable way to preserve a marketplace within a totally insured world, and it will be a tragedy if Obamacare fails to recognize it.
The catastrophic insurance policy is thus included by the Affordable Care Act only in the sense that some kind of health insurance is mandated. Used as part of a package with Health Savings Accounts, its split usefulness in two venues relies on health costs jumping sharply as soon as a patient is sick enough to go in a hospital. We also discuss in another place, the advantage of employing internal interest build-up in the Last Year of Life proposal. At this late point in the discussion, it is only useful to mention the fortuitous advantage that indemnity plans fit together, creating a strange ability to offset outpatient health costs against terminal care costs.
In any event, politicians must note that boundaries somehow have to remain flexible enough to adjust to changes. Service benefits are so flexible they could bankrupt us, so any replacement must not go that far. In the crudest brief description, Medical Savings Accounts seek to take advantage of the cost restraints of high-deductible ("catastrophic") health insurance, while easing the necessary pain by providing some patients with the money to do it with. It probably can cover all patients only if there is some temporary subsidy for the poorest. Some may need charitable assistance, and none can expect to enjoy the benefits of compound interest until interest rates return to normal. The pooling of investments in order to have professional management seems highly desirable if investment diversification is contemplated. Experience with these plans has shown that paying the money out of a tax-exempt fund has almost as much spending restraint as paying bills fully with cash, so costs are reduced by about 30% in actual experience. There might also be a reinsurance pool to pay for the occasional patient who exceeds the money in his account repeatedly, but the medical perception is that once you start going into the hospital, you either soon get better or you don't. Either way, there are few chronic diseases left; cancer and Alzheimer's disease, and that's about it. The strategy of giving poor people the three-to-five thousand dollars was originally envisioned to level the tax playing field with employer-based insurance, which still only provides tax avoidance for salaried employees. In recent years, a number of other ways to give away money by another name (especially funded tax credits) have been devised. They are not discussed further. HSA progress has been resisted for thirty years, but one consolation is that during the interval dozens of examples have been tried out, medical costs have regularly declined for workers, and both doctors and patients are satisfied with the arrangement. These savings come disproportionately from the outpatient arena since reimbursement of hospital inpatient costs often depends on negotiations between the insurer and the hospital. The use of market-based out-patient costs (MPC) as a basis for guiding physician decisions to cost-effective diagnosis and treatment, allows indirect hospital costs to be negotiated separately with third parties without fanciful allusions to linkages to billable services. Some hospitals could withstand this type of review, others could not. But it is certainly past time to have the discussion.
The Billing Mess No reimbursement system can be entirely satisfactory until provider accounting and billing are reformed. Health Savings Accounts were once resisted by those outsiders who benefited from unique tax exempted coverage, but the current climate is now favorable to deductibles almost everywhere. At least this much has been accomplished. Progress since 1980 has been retarded, not by lack of success, but by abnormally low-interest rates at banks imposed by the Federal Reserve, and by state laws mandating coverage of specific low-cost services. It is possible that the latter is motivated by a desire to exert indirect price control, and thus provide an opportunity for negotiations. It is also unwise to mandate coverage for birth control pills, cough medicine and like because experience in nations with nationalized health systems shows a tendency to be generous with low-cost items so as to conceal appalling harshness about expensive care. Doing so also brings to the fore such contraptions as the widespread three-insurance system for paying your bills. One policy now pays about 80%, another policy pays about 20%, while a major medical policy cleans up loopholes. This costly contrivance is even used to bill for individual refills in a drug store. The resulting chaos means most medical bills are not finally settled for several months, generating mountains of paperwork beyond average comprehension. With a Health Savings Account, the patient generally pays cash and gets a receipt for it, although the use of debit cards smooths that, and adding inpatient payments to the debit card would smooth it further. Useless itemized hospital bills should be revised to substitute market-based prices for inpatient items, thus restoring their usefulness for physician and patient cost guidance. Indirect hospital costs need not be shown on the bill at all; rather, they could be subjects for negotiation with third-party payers alone. Combining direct costs and indirect ones serves no identifiable purpose, since actual payments are now DRG or diagnosis-based rather than item-based, and indirect costs have become so large and cost-shifted that the combined figure is totally misleading for the analysis of cost-effectiveness. Periodically, the item composition of DRGs does need to be re-compiled, but this can be produced on demand for monitoring purposes, and would often be more useful if aggregates were examined rather than individual cases. The "grouping" of items in the DRG with similar costs rather than medical characteristics may have convenience for the billers and payers, but the process is highly approximated, at best, for any other use. For serious analysis, the entire ICD coding system needs to be abandoned, and to revert to an updated version of the original Standard Nomenclature system, now mainly in use by pathologists (SNOMED3). Many of these small reforms may seem technical and obscure, so a sentence needs repeating: No reimbursement system can be entirely satisfactory until provider accounting and billing are intensively reformed.
Summary of Improvements useful to integrating Obamacare with Health Savings Accounts.
- Enable commissions for salesmen of high-deductible health insurance to bundle their product with HSAs, debit cards, and reinsurance. This would not merely encourage this product, but assist the primary sales adviser in discouraging opportunistic fees and costs from banks who manage accounts..
- Encourage state governments to eliminate small-cost coverage mandates, which conflict with the high-deductible approach.
- Discourage co-pay coinsurance, which has shown little cost-restraining effect, but tends to encourage multiple claims costs.
- Charge some agency with monitoring inpatient charges, for the sole purpose of suggesting needed changes in the deductible amount of insurance to match them.
- Provide a system for subsidizing unpaid deductibles for poor people, which phases out when HSA accounts build up to the deductible amount but does not contain a disincentive to contribute to the Account.
- Study the need and cost of a reinsurance system or pooling arrangement, for those who exhaust their HSA balance, and thus require additional subsidy. Combining this with item 5. would be ideal.
- Establish a mechanism for using HSA (or other) information to establish the publication of national (and possibly regional) marketplace prices for medical items outside of institutional care.
- Charge a commission with determining relative pricing for items unique to hospital inpatients, building on values relative to outpatient charges..
- Re-cast DRG prices to conform to 7. and 8, with indirect institutional costs to be subject to unrelated audit and negotiation.
- Recast hospital bills to reflect 7, 8, and 9. in an easily intelligible way, including amounts actually paid by third parties.
- For DRG purposes, phase out the ICD diagnostic coding system, replacing it with SNOMED3 (formerly SNODO), or else use two codes for two dissimilar purposes.
- Charge some Committee of Congress to determine in advance what the rules should be for unspent surpluses of HSA accounts, at the death of the owner.
Co-Insurance (2)
New blog 2013-07-01 16:26:04 contentsIt's a convenience for the insurance company perhaps since it reduces the insurance cost by 20% and is easily figured on the back of a salesman's envelope. Therefore it helps in the three-way negotiation between the employer, the insurance company, and the union. The union calculates how much income tax the employees save by how much income is split between the "fringe benefits" (non-taxable) and the "pay packet" (taxable), and the negotiations shift around these offsets, usually at the end of grueling collective bargaining.
It was once explained to me that Co-pay was very popular with negotiators for unions and management because it was easy to calculate the total cost of it for an entire self-insured corporation. If a proposed budget for the employees was known, and the budget for health benefits was agreed, the arithmetic was easy. If the company has a 20% co-pay, it can reduce the company's total insurance cost by 20%, and if it doesn't come out right, you can negotiate 18% or 22% or whatever. Late at night when these negotiations characteristically get serious, the cost of the offer and counter-offer can be quickly calculated. By contrast, if a deductible is proposed, you have to know how many people use the program, how often they would get sick per year, and even so the calculation is difficult, requiring actuaries or at least accountants. So, the explanation ran, everybody, likes co-pay, and everybody hates deductibles. The insurance people present especially like co-pay, because there will soon be a demand to add it to the package as second insurance, and the premiums for that are also easily quoted, up or down as the negotiations proceed. When it got to involve Medicare and Medicaid, the Congressmen were in essentially the same position of only wanting to know what bulk costs of the whole program would be. In short, co-pay is easy to "score". But the best that can be said for it is, it's just another short-term benefit for which long-term costs are increased because there are diminished incentives for the third-party to hold them back. Just kick the can down the road.
It has never seemed completely credible that anyone would base expensive decisions on considerations so trivial, but you never know. Having invented Medical Savings Accounts with John McClaughry in 1980, for me the mysterious resistance to high deductibles has never seemed adequately explained. Negotiators must easily see that two (or three) insurance policies will be more expensive to administer than just one. They must immediately acknowledge that being 100% insured will increase costs by making the beneficiary ignore the cost, and they are probably willing to accept (off the record) the American Actuary Association's estimate that costs are thereby increased 30%. That much alone would free up about 5% of the Gross Domestic Product since we are currently spending 18% of GDP on Health care. There has almost seemed no point to go on that wages could be increased by diverting this wasted money to the pay packet, to say nothing of the frustration many doctors feel at having no idea of the true cost of what they order, and hence little interest in making the number smaller. Obviously, if true costs are concealed, they go up. This blinding of the doctor to true costs is what makes cost-shifting easy to do without criticism. The absence of a pool of deductibles makes it impossible to generate compound interest, and that in turn makes it less practical to consider "portability" of health insurance from one employer to the next. It is at the very root of fictitious costs for medical care of all sorts, which somehow seem to the advantage of many participants in the health field. Eliminating co-pay would result in a small saving, and it probably would result in a big saving in healthcare costs. The aggregate national savings would be astonishing. Health Savings Accounts are slow to be adopted, not because they fail to save money, but because state laws have imposed mandatory insurance benefits for small-cost items, apparently passed for the main purpose of undermining deductibles.
Most people initially resist the idea of a high deductible on the ground that poor people can't afford it. When it is explained that what is intended is basically to give the poor the money to pay for it, most resistance disappears. A more correct description is that some method is constructed to give them the money, but in a way that allows them to spend money left over from healthcare, for something else they want to buy. The ability to buy something else is not the same as wasting it, and safeguards are only prudent. Retirement is the use most commonly considered. Because interest rates are being suppressed by the Federal Reserve, this proposal may be somewhat retarded for a year or two, until interest rates return to normal levels. Addition of an inflation-protection feature (like TIPS) might well enhance its attractiveness. Ultimately, the first step would be to eliminate Co-pays. Completely and permanently.
Cost to Charge Ratio (2)
of the community when all is said and done, this system is designed to keep indirect costs within reasonable boundaries. If that aggregate is spoken of as a single product, its costs can be grouped together as company-wide costs. In the case of Apple, the main costs outside direct production costs are research and development, marketing and administration. In the case of hospitals, in addition to direct production costs, there is usually less marketing cost than a manufacturer would experience and considerably more charity. By calculating the variation of prices to costs among different products, it is possible to see which particular product is carrying the burden, and which product is being subsidized. In the case of hospitals, this analysis would permit an outside opinion to form about the fairness of such cross-subsidy, which is most commonly motivated by local competition. The neighbor hospital has some expensive gizmo and we don't; we buy a gizmo to keep up with them and subsidize its cost by overcharging for everything else. Decades ago there was a rage for establishing planning commissions to determine how many gizmos a community needs, but it was largely dropped because of bickering about what is normal business flexibility in every industry. It is now generally agreed that hospitals should have the business latitude to make these choices themselves, and suffer the consequences if unrelated prices get pushed out of line by cross-subsidies of excessive expansion.Indirect costs are a much harder matter to judge. Some administrators are paid too much, some renovations are excessive, some charity is really poor debt collection; but if these things are passed off to insurance companies, who pass them off to the public, they can unduly escalate. Direct costs are whatever they are, but indirect costs are more a matter of opinion. Some insight can be gained by measuring the ratios of direct to indirect costs, and then making a national comparison of those ratios with peer institutions, a process that is hampered by the traditional regulation by states instead of nationally. Since the cost of health care has long been rising faster than the cost of living, the suspicion is fostered that insurance companies put up less price resistance than a marketplace without them would. Since the cost of major illness is often beyond the means of its victims, insurance does seem to be called for, and the higher the cost the more that is true. For more than seventy-five years, health insurance has been in the middle, between the party who wants lower prices, and the party who wants higher ones. That may well have been a bad decision, requiring some experimentation with a return toward "indemnity insurance" and away from "service benefits". That is, the insurance pays money to the patient, and the patient then pays the bill. An indemnity system protects the insurance company from cost overruns, and this at least removes the pressure for the insurance company and the hospital to collude against the patients' financial interest. Once a suspicion arises that there could be some degree of collusion between the two, it is possible to see that using insurers to police a hospital's indirect costs may be something to discourage. Alternatively, it might be possible to apply patient copayment to the indirect, but not the direct, hospital costs. At the moment, copayments have little or no effect on patient utilization, but the selective application of them might be worth at least a pilot study, to see if they could dampen prices better than they affect service volume. A copayment of 20% of the indirect cost component of a patient's bill would certainly draw attention. Even a 1% copayment would dramatize the point.
Hospital prices have been inflated far too much, and far too irregularly, to serve as cost signals. In order to minimize the true cost of charity care, the services more heavily used by the indigent have had their indirect costs minimized by cost-shifting them away to better-reimbursed departments; it is a perfectly natural thing to do. Poorly utilized departments are subsidized by better-reimbursed ones; so what else is new? To assign a fixed ratio of charges to costs would greatly hamper the flexibility needed to keep the institution from failing. But without some understood relationship between the posted, stated price and its true cost, the hospital doctors are quite unable to design a cost-effective treatment strategy. Knowing very well the lack of relationship between prices and costs, the doctors freely admit they disregard the prices entirely. While allegiance to what is scientifically best is not completely bad, it is not necessary to be so blind to the economics of the various alternatives. In time, it will lead to the design of model treatment strategies by committees. That is not itself a bad thing, except for the way it undermines individual thinking by the professional who is closest to the specifics of a case. That is a debilitating thing; a bad thing if you wish. It certainly lessens the potential for minimizing the cost of care, which is the flag it is flying. Some way must be found to improve the usefulness of prices as a guide to costs, an imperative which is otherwise certain to lead to the use of some degree of force to achieve it. And that would be a really bad thing.
from the for the Hospitals tend to be either for-profit corporations like Apple or nonprofit corporations with a different accounting system. It may help a little to know that for-profit corporations are measured by their profitability, while nonprofits are measured by the increase (or decrease) in their assets compared with last year. Items enclosed on a balance sheet with parentheses have always gone in an (unfavorable) direction. Increases (or decreases) in assets are intended to include gifts and variations in stock market prices. However, increases (or decreases) in assets like fine art don't count at all. Sometimes that can be highly misleading, as when the Barnes Art Collection increased in value by billions of dollars. Other assets, like buildings and equipment, are measured by depreciation, which is not always parallel to market prices. There is a movement favoring "mark-to-market", but investment firms are particularly opposed to marking to market, because temporary drops in market price are sometimes unrealistic, only requiring a little time to recover, a phenomenon sometimes seen in endowment funds, as well. Conventional measures of success, like the profit margin and the increase in net assets for nonprofits, are generally useful. But they can also conceal many traps. The most prominent one is to introduce these concepts when someone questions why everything costs so much as if to imply that it is unlikely that a hospital could be overcharging when it is only generating a 2% profit.
The ten dollar aspirin tablet is usually introduced at this point in the discussion, balanced by descriptions of accident room patients who try to pay nothing at all. The discussion is now one of cost-shifting. It must be obvious that the cost to charge ratio is well over a thousand percent for the aspirin, whereas Apple probably is less than a hundred percent for everything they sell you. Perhaps not, perhaps it is over a thousand percent for a number of retail items. In any event, the problem for the hospital customer is he has no way of telling what is being given free to bring the overall cost to charges down to 5%. That is, he is given no role in choosing the charity he is supporting, but he knows it varies widely between hospitals. He has to have some trust that the institution is behaving in a responsible way, which is difficult when he sees new and glistening hospital interiors or reads of seven-figure executives. Perhaps it is a little unfair to blame the trustees for avoiding embarrassing questions with no particular justification, but it does not seem unfair to ask that the hospital cost accountant prepare meaningful reports to both the management and the trustees. To the management first, to allow them time to look into oddities in the reports before having to answer for them. But no matter how it is handled, the cost accountant should be made more central than he usually is.
Every item ought to be assigned a cost to charge ratio, both inclusive and exclusive of overhead costs. It is usual to include overhead by a so-called step-down process since overhead must be paid and it generates no charges at all, only costs. But to include it in the net cost to charge ratio is potentially to bury one of the things you are trying to discover: is the overhead excessive? Having determined that point, it may be legitimate to re-include overhead in the "net" calculation of the cost to charges. Hence the suggestion of reporting it both ways. No one doubts the books balance; the items of expenditure include most of the costs. The essential issue is whether this is all pretty expedient, whether too much frivolous expenditure is being permitted by shifting its cost to certain profit centers. When this cost to charge system is compared among other hospitals or other years in the same hospital, it is possible to recognize the unusual items or departments quickly. However, the beginning trustee or utilization reviewer may need to have the costs and charges stripped out and aggregated, to highlight the highly deviant figures for ready appraisal. Consequently, it may be necessary for the insurance company to require reports of certain items, structured in that way. Other such reports may be needed to identify overpaid employees, or overstaffed departments, usually as patients and dollars per employee, compared with other institutions. Ultimately, it may even be necessary to establish norms, but that begins to resemble micromanaged cost control, when peer pressure may be all that is required.
Obamacare's Constitutionality

|
| President Barack Obama |
Any idea of a smoothly orchestrated introduction of the new law was jarringly interrupted by the U. S. Supreme Court, which granted a hearing to a complaint by 26 State Attorney Generals, that the ACA Act was unconstitutional. It was big news that the whole Affordable Care Act might be set aside without selling a single policy of insurance. The timing (before the Act had actually been implemented) served to guarantee that the constitutional issue, and only that issue, would be discussed at this Supreme Court hearing. By implication, there might be more than one episode to these hearings.
While many could have declaimed for an hour without notes, about difficult issues perceived in the Obama health plan, questioning its constitutionality had scarcely entered most minds. Then of a sudden, near the end of March 2012, a case testing the constitutionality of mandatory health insurance was granted certiorari and very promptly argued for three full days before the U.S. Supreme Court. Twenty-six state attorneys general brought that case, so it was not trivial. In jest, one Justice quipped he would rather throw out the whole case than being forced to spend a year just reading 2500 pages of it. But Justices are practiced in the art of quickly getting to the heart of a matter; it soon boiled down to one issue: was it constitutional for Congress to force the whole nation to purchase health insurance? Is there no limit in the Constitution about what the federal government can force all citizens to do, even though the federal government itself is severely limited in scope? Even though the Tenth Amendment states that anything not specifically granted to the federal becomes the province of the states? Would a people who fought an armed revolution for eight years over a 2-cent tax on tea, now consent to a much larger requirement which it was not constitutionally authorized to impose? Most people finally wrapped their heads around some formulation of this non-medical concept to a point where they vaguely understood what the Judges were arguing about. This was beginning to look like a topic where We The People made a covenant with our elected leaders, and reserve the sole right to change it.
 The powers not delegated to the United States by the Constitution, nor prohibited by it to the States, are reserved to the States respectively, or to the people. 
|
| Tenth Amendment |
The Constitution describes a Federal system in which, a few enumerated powers are granted to the national government but every other power is reserved to the state legislatures. The Constitution had to be ratified by the states to go into effect, and the states had such strong reservations about the surrender of more than a handful of powers that they would not ratify the document unless the concept of enumeration was restated by the Tenth Amendment. If states could not be persuaded of the need for a particular power to be national, they might refuse to ratify a document which enabled permanent quarrels about the issue. That wariness explains why The Bill of Rights goes to the extra trouble of declaring certain powers are forbidden to any level of government.
Separation of powers further explains why Mr. Romney's mandatory health insurance plan might be legal for the Massachusetts legislature but prohibited to Congress. After Chief Justice Roberts got through with it, whether that truly remains the case will now depend on whether it is described as a tax, a penalty, a cost, or whatever, and only if the U.S. Supreme Court later agrees that was a proper definition. Because -- to be considered a tax it must be too small to be considered coercion. The law itself apparently does not underline this distinction in a way the Justices felt they could approve. Indeed, while Mr. Obama in his speeches firmly declared it was not a tax, later White House "officials" declared it might be. There was agreement the Federal government could tax, but no acknowledgment that taxes might have any purpose other than revenue.
Under circumstances widely visible on television, however, it was clear that the House of Representatives had been offered no opportunity to comment on this and many other points in this legislation. To a layman, that fact itself seems as clear a violation of constitutional intent as almost any other issue, since the Constitution indicates no idea was ever contemplated that any President might construct laws, nor like the courts, interpret their meaning. The first three Presidents repeatedly raised the question of whether they had the authority to do certain things we now take for granted. And Thomas Jefferson was similarly boxed in by a clever Chief Justice, who said, in effect, Agree to This Decision, or be Prepared to Get a Worse One. The Constitution says it is the function of the Executive branch to enforce the law, "faithfully". Presumably, all of the thousands of regulations issued by the Executive Branch under this law must meet the same test.
Given that the Justices now hold it constitutional for the federal Congress to mandate universal health insurance, based on some authority within taxation, the immediate next issue is paying for it. Millions of citizens, usually young and healthy but sometimes for religious reasons, do not want to buy health insurance and would be forced to do so by this law because the only available alternative is to pay a revenue tax. The purpose of including them is to overcharge people who will predictably under-use community-rated insurance, and thus enable the surplus to reduce costs for those who do want to buy health insurance. (Here, the Court had the pleasure of reducing an unusually opaque law to an unusually succinct summary.) To avoid the charge of a "taking", the Administration must either surrender on the universal mandatory point or else surrender the level premiums of community rating. The lawyers for the complaining attorneys general laid great stress on this particular issue in their arguments, and it occasioned much of the discussion from the bench. However, until the law is in action there is as yet no cause for damages.
Here it will depend on whether you call it a permissible activity for Massachusetts or for the Federal government. The Constitutional point seems to be that it is a legitimate Federal power to tax for the "general welfare", so it now becomes essential to know if the taxes for noncompliance in Obamacare are really a penalty. The Justices seemed to be questioning whether the whole scheme would collapse with the forced subsidy eliminated, and because of that be deemed to have been a "general welfare purpose" adequate to meet the constitutional requirement of a permissible enumerated purpose. Lawyers can generally find such a defined purpose in the words of the Constitution, even if they have to dip into the penumbras and emanations of the words. So the question might just devolve into whether a majority of the Justices wish to declare the penumbra to be within the enumerated powers of Congress. To all of this, the lawyers for the attorneys' general reply that such an enumerated power is impossible because there is no limit to what could be done by this method. Congress would then be allowed to mandate that everyone eat broccoli for dinner, or buy a General Motors car in order to pay for the deficits of rescuing that company from bankruptcy. Almost anything could be mandated by establishing a penalty called a tax; including a mandate that everyone buys a product in order to pay for the deficits of mandating it, illustrates there exists at least one circularity of enumerating something like a power of Congress. According to this reasoning, mandated health insurance cannot, therefore, be an enumerated power of Congress, either now or at any time in the future. The sort of speculative law outlined in this paragraph is exactly the sort of thing the Supreme Court dislikes and shows the utility of denying access to the courts to anyone who cannot claim "standing", defined as a claim of actual injury from a law.
The Justices undoubtedly had to weigh the fact that the American public has a strong distaste for this sort of convoluted reasoning, which sounds like a convention of Jesuit priests having fun. On many other occasions, however, the public has accepted the judgment of people it hired to understand this sort of thing; that's called respect for the law. Eighty years ago in the Roosevelt court-packing case, there was the same sort of collision between the Court and the President, and the Court knuckled under even though the public supported the Court. In both cases, the Court seemed to be yielding to the President, with the unspoken compromise that the President would not pursue his earlier course with quite so much vigor. Since the really central 1937 question of overturning the Interstate Commerce clause ("Commerce among the several states") was left unaddressed, the velvet glove might yet contain an iron fist.
Roberts the Second

President George W. Bush nominated John Roberts to be Chief Justice of the U.S. Supreme Court in 2005. Since then, the Chief's administrative changes to the court and the whole court system have been slow but methodical. To the extent the Chief Justice has control of the matter, Roberts has been taking steps which make the Court into a more thoughtful branch of the Federal Government, ultimately making it more powerful. His first step was to reduce the number of cases considered each year, constraining them to conflicts between lower jurisdictions, unless otherwise mandated. This year, the number of cases heard is about eighty, or only half of the previous numbers. The policy lets unconflicting Appellate judgments stand. A second court must disagree with the first one, for the Supreme Court to enter the case.
The so-called Obamacare case, (NFIB v. Sebelius), meets this conflict-between-jurisdictions standard, but is notable for other innovations. The case was nationally broadcast as a live slide show. It heard arguments lasting three days instead of the usual single hour, and of course, it broke new substantive ground in a case of national interest. The decisions will now get more press attention; but this relatively rapid evolution toward a national debating contest, through modified Court procedure, is more important than it looks. It would be saying too much to claim the whole nation now fully understands its Constitution of enumerated powers, but surely the citizens who have only recently learned something about it must number in the millions. Before this case, many law school graduates might have had difficulty describing the design of the federalized system in a plausible dinner-table conversation. It's not yet clear where John Roberts is going, but he is surely trying to bring the public along with him.
During the semi-televised arguments, I was at first impressed with the rapid-fire exchanges between Justices and litigators about the operation of health insurance. Some people are born with high-speed brains and high-speed speech apparatus; no doubt, such people are sought after to represent others in court. But after practicing Medicine for sixty years and writing books about health insurance, I recognized that several rapid-fire responses by the attorneys were confident but off-target. Frankly, if you only have a few minutes but many points to make, and have to say them before someone interrupts, you would almost have to be a circus freak to manage. This is quite unnecessary, no matter how entertaining it may be to other lawyers. There seems no reason why the questions cannot be submitted in writing, sometimes employing experts on the specific points, and allowing enough time without interruption to devise a thoughtful answer. At present, it seems to matter more what the litigating attorney will agree to, than what is the fact. The outcome of cutting a litigant off after he says, "Yes, your honor, but.." is now only to establish whether both sides agree on a point; just why they agree or disagree is not even sought, let alone disregarded. It would seem useful to know Justice Thomas' reasons for abstaining from questions during oral arguments, for a different sort of example. So, it is easy to imagine that John Roberts has some thoughtful goals in modifying Supreme Court traditions, and equally understandable if jurists of this distinction become irritated by suggestions from the peanut gallery. It is thus fitting that we all hold back and first watch where the varsity means to take us. But allowing the public to express an opinion, is not the same as lobbying for it.
The Obamacare Act was about 2600 pages long, and two years after the President signed the bill, more than half of the necessary regulations remain to be written. The Law is "not severable", which is to say individual pieces of it cannot be attacked in court, without potentially upsetting decisions made on other portions. As a consequence, both the good and bad parts could endure for a long time to come. Or, the whole thing could suddenly sink from sight, relatively quickly. If the Justices can tolerate it, this legislation with many "moving parts" could be in the courts for a long time to come. So, Justices will then find the rule Roberts has made, of only accepting conflicts between the jurisdictions, protects their time and patience. But in doing so it will shift most final judgments into the hands of the lower, appellate courts. The legal profession will like this quite a lot. It will be like the gratifying situation said to prevail when a commanding General decides to retire -- everybody down the line could get promoted one notch.
By artfully selecting cases to argue, there were here four points open to the decision. Only two of them eventually had bearing on the final outcome of this case, but the whole issue is not necessarily concluded. The first decision got the most attention, deciding that the penalty for not having health insurance could be read as just a tax, and therefore was legal for Congress to use as a Constitutional basis for making health insurance mandatory, as Roberts declared the "Commerce clause" was not. The distinguishing feature of a Congressional exaction which is "just a tax" appears to be whether it exceeds the expenditure intended; if it exceeds the expenditure it would presumably be punitive. Nothing had seemed more important to the Founding Fathers than to expand the ability of the national government to impose taxes to service war debts. To truncate this wish of George Washington and Robert Morris into a short-cut, "Congress has the right to tax", or conversely to expand its confining language into "Congress has the right to tax in order to make private health insurance compulsory" just points up that the only real purpose of taxes in Washington's day was to wage war, and that the purpose of allowable taxes probably would have been defined if other purposes had been foreseen. Someone could usefully point out that what the Constitution really means is that Congress has the right to tax for "defense and the general welfare", and challenge anyone to argue otherwise. One sees the clever hand of Gouverneur Morris fuzzing up that argument; are we to ignore the fungibility of money and ask whether Congress may spend money on the general welfare only if it is general? How about earmarks, for example, are they all for the general welfare?
However, to turn a blind eye toward interesting issues is apparently a price that must be paid for obtaining the right for the Chief Justice to write the majority opinion, which eventually slips in some language (in legal language, an obiter dictum) to the effect that , of course, you couldn't use the Commerce Clause to do that. Getting Justice Ruth Ginsburg to sign that will eventually sound like the box John Marshall constructed in Marbury v. Madison. If that obiter dictum is as heat-resistant as the opinions of the first Justice Roberts in Franklin Roosevelt's court-packing effort, then the Commerce Clause is likely to be off-limits for a long time. Of course, if Chief Justice Roberts had joined the other four conservatives he would still have been able to write the majority opinion, but in the opposite direction. Except of course for that inevitable political accusation: There you go again, you 5-4 conservatives.
The second decision, in this case, is the sleeper. Congressional managers in charge of writing the bill had finally decided they had no way to cover 40 million uninsured people, except by diverting fifteen million of them into what is acknowledged to be the absolutely worst part of the American medical system, the state Medicaid programs. And because many States Rights advocates were in charge of state Governor's offices, the Congressional bill-writers added what is now a fairly familiar prod to cooperation. That is, if a state refuses to take the extra Medicaid patients, it will lose all federal funds for existing clients of state Medicaid. This sort of coercive provision has become so standard in highway bills and other federal programs operating at the state level, that it was largely unnoticed in the 48 hours the Congress was given to examine 2600 pages of legislative provisions. This, however, is blackmail, said John Roberts, quite unallowable under the defined separation of powers of the Constitution, between the state and federal levels of government. Furthermore, if some state decides to accept the penalty, it could close the existing program for the poor and accept the subsidy for the middle class, thus enhancing their revenues and reducing their obligations to the poor. Congress must now devise new strategies for suggesting federal programs to the states, and probably will do so. But the financial blackmail strategy now has a permanent black eye, with a skeptical public eye on the alert for it. The ironic conclusion of all this comes from the Congressional Budget Office, which predicts we will end up with 30 million uninsured persons, anyway.
What's awkward about this was immediately pointed out by attorney Richard Epstein: it ignores the century-old precedent set by Chief Justice Taft. Writing about a Child Labor law, Taft created a Supreme Court precedent that the Constitutional taxing power of the national government may not be used to implement what cannot be implemented directly. We can now see an example within the borders of a single case, where the Constitutional taxing power provision is used to indicate an otherwise impermissible Obamacare, and a few pages later its use is forbidden in the case of Medicaid in order to accomplish a forbidden coercion. Locating the two issues in the same case decision helps make the distinction between using the taxing power for revenue, and using it to coerce obedience; the distinction grows as the magnitude of the tax grows, particularly after it exceeds the intended government expenditure. What is not emphasized is the basis for Chief Justice Roberts reversing the precedent set by Chief Justice Taft on the same topic a century earlier. He did it with the Obiter dictum, and yet he didn't exactly do it. The four liberal Justices who co-signed the decision are not in a position to dispute it, while the four conservative Justices may not wish to. In either direction, however, the vote of the current Chief Justice appears to be both decisive and subtle.
It remains to be seen whether the 'tax, not commerce' strategy was clever. If the tax approach proves to be durable, it presumably extends to a wide range of legislation since Roosevelt's New Deal. Already, its awkward features have emerged in renaming portions of Obamacare into Chapter 48 of Subtitle D of the Internal Revenue Code of 1986 (!). Any law student who tries to look that up is going to have a frustrating time. But on the other hand, sometimes you win by losing. If it should somehow not be a tax, it has already been excluded from the Commerce Clause, so it has no hook left in the Constitution on which to hang it. There's something in this whole wrangle which resembles the position of Germany and Japan after the Second World War. In spite of losing that war, those two nations seem to have prospered better than England and Russia, who lost their empires but are said to have won the war .
A Government of Limited Powers

|
| U.S. Supreme Court |
The Canadian nationalized health system was organized in 1984 as a collection of provincial health systems under national control, and American visitors frequently asked how such a hybrid had been put together. Very simple, replied those who approved; very sly and tricky, replied those who disapproved. Canadian provinces were all taxed for the costs of the healthcare system, but the only provinces to receive benefits were those who agreed to the Federal plan. Effectively, a province had to pay for it no matter what but only got some benefits if it agreed to the rules. So one by one, even in the oil-rich western provinces, they reluctantly agreed. Obamacare seemed to be following the same pattern when the Affordable Care Act specified that only States with State-organized insurance exchanges would receive subsidies for the expanded State Medicaid programs needed to supply coverage, but of course, the citizens of all states would have to pay for it. The law provided that if a state declined to set up an exchange, the Federal Government would set one up in their state. But states with such federal exchanges would receive no subsidy. The states which rejected the establishment of state insurance exchanges immediately found themselves in the same position as the Canadian Provinces in 1984 -- assigned the costs but denied the subsidies -- unless they complied with the dictates of the Federal Government, which in this case found it convenient to describe itself as helpless to challenge the declared will of Congress. As it turned out, 36 states unexpectedly rejected state exchanges and so were given federal ones. It made it all a little awkward to run someone else's program without funding. Their rejection hardened decisively when, shortly afterward, the U.S. Supreme Court disapproved this whole arrangement, calling it "blackmail."

The response of the Administration, which by then couldn't change the law because the 2010 elections had revolted and elected a Republican House of Representatives, was to change the regulations to be in conflict with the law which created them. In these days of televising the meetings of Congressional committees, the nation was treated to the spectacle of watching Chairman Issa's jaw drop. The lawyer who was defending the Administration's position repeated several times that she "could find no evidence" that the law had been written the way it was in order to pressure states into forming exchanges, and she would scarcely go a word beyond that. Apparently, she expected Congress to believe that the Affordable Care Act had really been written by Congress when earlier televised hearings had allowed the public to watch how the Administration dumped it on the desks of Congress with no time even to read it. The reason for this later change of heart would seem pretty obvious in view of the Supreme Court decision, but to misrepresent it before the same congressmen who had been manhandled by it, was apparently more than Chairman Issa could find words to express. Issa quickly adjourned the hearings, and no doubt he and everyone else retreated to the lawbooks for help in deciding what in the world to do next.
If so, they undoubtedly encountered the McCarran Ferguson Act of 1945, which provides."No Act of Congress shall be construed to invalidate, impair, or supersede any law enacted by any State for the purpose of regulating the business of insurance". The McCarran Act had the purpose and effect of retaining the regulation of the insurance industry -- alone among major industries -- in the hands of state governments. This regulatory shift, in turn, responded to the Roosevelt Court-packing fracas of 1937, which was firmly centered on the "Commerce clause" of the Constitution, which states "Congress shall have the power...To regulate Commerce with foreign Nations, and among the several States, and with the Indian Tribes". Essentially, the Roosevelt Administration by insisting that the word "interstate" be effectively removed from common usage and understanding of the power of the Federal Government to regulate commerce and commerce, was amending the Constitution in an unconstitutional way. As matters turned out, insurance was the only industry to be excepted. In spite of a recent popular landslide in 1936 re-electing FDR, the Supreme Court had initially refused to agree to re-interpreting the Constitution even with Roosevelt's threat to keep appointing new Justices until he got a majority. Ever since, the word "interstate" has disappeared from language about the Constitution, by a process which certainly does not resemble the methods specified for amendments. Since for nearly seventy years, insurance regulation has been in the hands of state governments, it will be interesting to see how the meaning is interpreted of "No Act of Congress shall be construed". In a nice reminder of this whole absolutely focal point in Judicial history, the Justice who switched his vote and made it all possible was also named Roberts. Justice Owen Roberts of Philadelphia.
Void for Vagueness?
The three branches of government have become unbalanced. Obamacare and the Dodd-Frank Bill were almost entirely written outside of the Legislative branch, and their ensuing regulations will also be written in the Executive branch. The founding fathers certainly never envisioned such sweeping modifications would be made in the medical and financial industries, against the wishes of these industries, and in any event, without convincing demonstration, the public either understood or was in favor. This is what is fundamentally wrong about taking such important decisions out of the hands of Congress; it leaves the public wondering who makes these puzzling laws.
|
| Justice George Sutherland |
There is no need to go further than this, harsh words will only inflame the reaction more than necessary to justify a pull-back. And yet, the Supreme Court would certainly do us mercy if it doused these flames; perhaps the Supreme Court needs a legal pretext. May we suggest that Justice George Sutherland, who sat on the court seventy years ago, may have sensed a similar direction to things, short of using a particular word. Justice Sutherland recognized that although it is impractical to waver from the principle that ignorance of the law is no excuse, it is nowadays entirely possible for a person of ordinary understanding to read a law in its entirety and still remain confused as to its overall intent. Sutherland thus created a legal principle that a law may be void if it is too vague to be understood. We might also add "too carelessly written", and/or "too obscurely constructed". In particular, said Sutherland, a common criminal may be even less able to make a serious analysis of the case against him. Therefore, at least in criminal cases, a law may well be void for vagueness. In this case, we are not speaking of criminals as defendants or civil cases of alleged damage of another party by a defendant. Here, it is the law itself which gives offense by its vagueness, and Congress which created the vagueness is the defendant. Since we have just gone to considerable length to describe the manner in which Congress is itself ultimately the main victim, this situation may be one of the few remaining ones where a Court of Equity is needed. That is, an obvious wrong needs to be corrected, but no statute seems to cover the matter. The Supreme Court might give some thought to convening itself as a special Court of Equity, on the special point of whether this legislation is void for vagueness.
We indicated earlier that one word was missing in this bill of particulars. That would be needed, to expand the charge to void for intentional vagueness, an assessment which is unflinchingly direct. It suggests that somewhere in at least this year's contentious processes, either the Executive Branch or the officers of the congressional majority party, or both, intended to achieve the latitude of imprecision, that is, to do as it pleased. Anyone who supposes the general run of congressmen voluntarily surrendered such latitude in the Health or Finance legislation, has not been watching much television. Given the present vast quantity of annually proposed legislation, roughly 25,000 bills each session, the passage of a small amount of vague legislation might only justify voiding individual laws, whereas an undue amount of it might additionally justify a reprimand. However, engineering laws which are deliberately vague, might rise to the level of impeachment.
The following final rule of the regulations of the Affordable Care Act, is reproduced Verbatum in order to illustrate the nature of the problem. It might not be the best instance to select for a lawsuit, but it is a handy example of how turgid regulatory language can completely baffle the people compelled to obey, and therefore gives regulators a freer hand to act as they please without challenge. Without implying this particular lack of clarity is deliberate, at the very least it illustrates how little effort was devoted to making it clear. If ignorance of the law is no excuse, a person who actually reads it has a diminished excuse for not understanding it while remaining no wiser. In view of this injury, its authors equitably should be subject to discipline for careless composition.
Final Rule: Outpatient Reimbursement Regulations
Political Parties, Absent and Unmentionable

|
| King George III |
BECAUSE America had recently revolted to rid itself of King George III, the Constitutional framers of 1787 sought to construct a government forever free from one-man rule. Inefficiency could be accepted but central dictatorial power, never. It is unrealistic however to expect a wind-up toy to keep working forever, and our Constitution creates the same worry. After two centuries, some chinks have appeared.
|
| Founding Fathers |
Political parties existed in 18th Century England and Europe, but the American founding fathers seem not to have worried about them much. Within ten years of Constitutional ratification, however, Thomas Jefferson had created a really partisan party which naturally provoked the creation of its partisan opposite. James Madison was slowly won over to the idea this was inevitable, but George Washington never budged. Although they were once firm friends, when Madison's partisan position became clear to him, Washington essentially never spoke to him again. Andrew Jackson, with the guidance of Martin van Buren, carried the partisan idea much further toward its modern characteristics, but it was the two Roosevelts who most fully tested the U.S. Supreme Court's tolerance for concentrating new powers in the Presidency, and Obama who recognized that the quickest way to strengthen the Presidency was to weaken the Legislative branch.
Dramatic episodes of this history are not central to present concerns, which focuses more on the largely unnoticed accumulations of small changes which bring us to our present position. Wars and economic crises induced several presidents, nearly as many Republicans as Democrats, to encourage migrations of power advantage which never quite returned to baseline after each crisis. Primary among these migrations was the erosion of the original assumption of perfect equality among individual members of Congress. A new member of Congress today may tell his constituents he will represent them ably, but when he arrives for work he is figuratively given an office in the basement and allowed to sit on empty packing cases. This is not accidental; the slights are intentional warnings from the true masters of power to bumptious new egotists, they will get nothing in their new environment unless they earn it. Not a bad idea? This schoolyard bullying is a very bad idea. If your elected representative is less powerful, you are less powerful.

|
| Houses of Congress |
Partisan politics begins with vote-swapping, evolves into a system of concentrating the votes of the members into the hands of party leaders, and ultimately creates the potential for declaring betrayal if the member votes his own mind in defiance of the leader. The rules of the "body" are adopted within moments of the first opening gavel, but they took centuries to evolve and will only significantly change direction on those few occasions when newcomers overpower the old-timers, and only then if some rebel among the old timers takes the considerable trouble to help organize them. In the vast majority of cases, after adoption, the opportunity to change the rules is then effectively lost for two years. Even the Senate, with six-year staggered terms, has argued that it is a "continuing body" and need not reconsider its rules except in the face of a serious uprising on some particular point. Both houses of Congress place great weight on seniority, for the very good purpose of training unfamiliar newcomers in obscure topics, and for the very bad purpose of concentrating power in "safe" districts where party leaders are able to exercise iron control of the nominating process. Those invisible bosses back home in the district, able to control nominations in safe districts, are the real powers in Congress. They indirectly control the offices and chairmanships which accumulate seniority in Congress; anyone who desires to control Congress must control the local political bosses, few of whom ever stand for election to any office if they can avoid it. In most states, the number of safe districts is a function of controlling the gerrymandering process, which takes place every ten years after a census. Therefore, in most states, it is possible to predict the politics of the whole state for a decade, by merely knowing the outcome of the redistricting. The rules for selecting members of the redistricting committee in the state legislatures are quite arcane and almost unbelievably subtle. An inquiring newsman who tries to compile a fifty-state table of the redistricting rules would spend several months doing it, and miss the essential points in a significant number of cases. The newspapers who attempt to pry out the facts of gerrymandering are easily gulled into the misleading belief that a good district is one which is round and compact, leading to a front-page picture showing all districts to be the same physical size. In fact, a good district is one where both parties have a reasonable chance to win, depending for a change, on the quality of their nominee.
So that's how the "Will of Congress" is supposed to work, but the process recently has been far less commendable, and in fact, calls into dispute the whole idea of a balance of power between the three branches of government. We here concentrate on the Health Reform Bill ("Obamacare") and the Financial Reform Bill ("Dodd-Frank"), which send the same procedural message even though they differ widely in their central topic. At the moment, neither of these important pieces of legislation has been fully subject to judicial review, so the U.S. Supreme Court has not yet encumbered itself with stare decisis of its own creation.
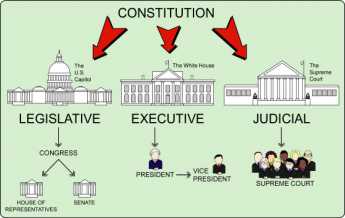
|
| Three branches of government |
In both cases, bills of several thousand pages each were first written by persons who if not unknown, are largely unidentified. It is thus not yet possible to determine whether the authors were affiliated with the Executive Branch or the Legislative one; it is not even possible to be sure they were either elected or appointed to their positions. From all appearances, however, they met and organized their work fairly exclusively within the oversight of the Executive Branch. Some weighty members of the majority party in Congress must have had some involvement, but it seems a near certainty that no members of the minority party were included, and even comparatively few members of highly contested districts, the so-called "Blue Dogs" of the majority party. It seems safe to conjecture that a substantial number either represent special interest affiliates or else party faithful from safe districts with seniority. The construction of the massive legislation was conducted in such secrecy that even the sympathetic members of the press were excluded, and it would not be surprising to learn that no person alive had read the whole bill carefully before it was "sent" to Congress. It's fair to surmise that no member of Congress except a few limited members of the power elite of the majority party were allowed to read more than scattered fragments of the pending legislation in time to make meaningful changes.
The next step was probably more carefully managed. No matter who wrote it or what it said, a majority of the relevant committees of both houses of Congress had to sign their names as responsible for approving it. Because of the relatively new phenomenon of live national televising of committee procedure, the nation was treated to the sight of congressmen of both parties howling that they were only given a single day to read several thousand pages of previously secret material -- before being forced to sign approval of it by application of unmentioned pressures enabled by the rules of "the body". When party members in contested districts protested that they would be dis-elected for doing so, it does not take much imagination to surmise that they were offered various appointive offices within the bureaucracy as a consolation. As it turned out, the legislation was only passed narrowly on a straight-party vote, so there can be a considerable possibility of its likely failure if the corruptions of politics had been set aside, with members voting on the merits. Nevertheless, since this degree of political hammering did result in a straight-party vote, it leaves the minority party free to overturn the legislation when it can. The prospect of preventing an overturn in succeeding congresses seems to be premised on "fixing" flaws in the legislation through the issuance of regulations before elections can open the way to overturn of the underlying authorization. Legislative overturn, however, is very likely to encounter filibuster in the Senate, which presently requires 40 votes. Even that conventional pathway is booby-trapped in the case of the Dodd-Frank Law. The Economist magazine of London assigned a reporter to read the entire act, and relates that almost every page of it mandates that the Executive Branch ("The Secretary shall") must take rather vague instructions to write regulations five or ten times as long as the Congressional authorization, giving the specifics of the law. The prospect looms of vast numbers of regulations with the force of law but written by the executive branch, emerging long after the Supreme Court considers the central points, years after the authorizing congressmen have had a chance to read it, and well after the public has rendered final judgment with a presidential election. The underlying principle of this legislation is the hope that it will later seem too disruptive to change a law, even though most of it was never considered by the public or its representatives.
|
| Bill become a Law |
The "regulatory process" takes place entirely within the Executive branch. Congress passes what it terms "enabling" legislation, containing language to the effect that the Cabinet Secretary shall investigate as needed, decide as needed, and implement as needed, such regulations as shall be needed to carry out the "Will" of Congress. Since the regulations for two-thousand-page bills will almost certainly run to twenty thousand pages of regulations with the force of law, the enabling committee of Congress will be confronted with an impossible task of oversight, and thus will offer few objections. The Appropriations Committees of Congress, on the other hand, are charged with reviewing every government program every year and have the power to throttle what they disapprove of, by the simple mechanism of cutting off the program's funds. Members of the coveted Appropriations Committees are appointed by seniority, come from safe districts, and are attracted to the work by the associated ability to bestow plums on their home districts. By the nature of their appointment process, unworried by the folks back home but entirely beholden to the party bosses, they have the latitude to throttle anything the leadership of their party wants to throttle badly enough. The outcome of such take-no-prisoners warfare is not likely to improve the welfare of the nation, and therefore it is rare that partisan politics are allowed to go so far.
The three branches of government have become unbalanced. These bills were almost entirely written outside of the Legislative branch, and the ensuing regulations will be written in the Executive branch. The founding fathers certainly never envisioned that sweeping modification will be made in the medical industry and the financial industry, against the wishes of these industries, and in any event without convincing proof that the public is in favor. This is what is fundamentally wrong about taking such important decisions out of the hands of Congress; it threatens to put the public at odds with its government.
|
| Justice George Sutherland |
There is no need to go further than this, harsher words will only inflame the reaction further than necessary to justify a pull-back. And yet, the Supreme Court would do us mercy if it doused these flames; the Supreme Court needs a legal pretext. May we suggest that Justice George Sutherland, who sat on the court seventy years ago, may have sensed the direction of things, short of using a particular word. Justice Sutherland recognized that although it is impractical to waver from the principle that ignorance of the law is no excuse, it is entirely possible for a person of ordinary understanding to read law in its entirety and still be confused as to its intent. He thus created a legal principle that a law may be void if it is too vague to be understood. In particular, a common criminal may be even less able to make a serious analysis. Therefore, at least in criminal cases, a lawyer may well be void for vagueness. In this case, we are not speaking of criminals as defendants or civil cases of alleged damage of one party by a defendant. Here, it is the law itself which gives offense by its vagueness, and Congress which created the vagueness is the defendant. Since we have just gone to considerable length to describe the manner in which Congress is possibly the main victim, this situation may be one of the few remaining ones where a Court of Equity is needed. That is, an obvious wrong needs to be corrected, but no statute seems to cover the matter. The Supreme Court might give some thought to convening itself as a special Court of Equity, on the special point of whether this legislation is void for vagueness.
We indicated earlier that one word was missing in this bill of particulars. That would be needed, to expand the charge to void for intentional vagueness, an assessment which is unflinchingly direct. It suggests that somewhere in at least this year's contentious processes, either the Executive Branch or the officers of the congressional majority party, or both, intended to achieve the latitude of imprecision, that is, to do as it pleased. Anyone who supposes the general run of congressmen voluntarily surrendered such latitude in the Health and Finance legislation, has not been watching much television. Given the present vast quantity of annually proposed legislation, roughly 25,000 bills each session, the passage of a small amount of vague legislation might only justify voiding individual laws, whereas an undue amount of it might additionally justify a reprimand. However, engineering laws which are deliberately vague might rise to the level of impeachment.
Chicago Sauce on an Arkansas Turkey
Presumably, the proposers of affordable health coverage considered the approach of making it affordable through making it cheaper. Unfortunately, "affordable for every American" is so expansive that some people, somewhere, would require extra subsidy no matter how much prices were cut. Obamacare's supporters would be bitter to discover a two-class system, with them in second class. It did not take long to see how unpopular cutting existing programs would be, first with providers and then with provides. And then Obama advisors must have developed a greater understanding that existing internal hospital cost-shifting meant: Medicare was already subsidizing Medicaid, while the private sector had really been subsidizing the indigent care that Medicaid excluded. The savings to government costs (of universal coverage) were not going to be nearly as much as had been imagined.
So, a subsidy program was required. In addition, ensuring illegal immigrants during high unemployment was seriously unpopular, particularly in border states like Texas, where uncompensated care was already hard to manage. So we can easily imagine how the proposal emerged as: "Affordable health coverage for all Americans (legal residents only) achieved by giving cash subsidies ("refundable tax credits") to lower income groups, and expanding Medicaid coverage above its former income threshold". That wouldn't be a catchy political slogan, but it would be precise.
Such patchwork necessarily made it harder to comprehend. Somewhere in its evolution someone also seems to have determined to rescue Medicare from its impending bankruptcy -- while we are at it, let's fix Medicare. However both ideas, universal coverage and restructuring Medicare solvency, would be expensive; combining them might make the package unsupportably expensive in a recession, but it might also create more opportunity for major progress.
 Affordable health coverage for all Americans (legal residents only) was to be achieved by giving cash subsidies ("refundable tax credits") to lower income groups while expanding Medicaid coverage limits to include them. A universal mandate for coverage, (but only our way, or the highway.) 
|
| Obamacare Capsulized |
The Obama administration seemed to follow the same path. Modifying the pathway to a Budget Reconciliation Committee added the novel advantage of avoiding the Senate's 60-vote anti-filibuster rule, thus requiring only a simple majority to pass the Senate when it returned. It still needed 60 votes in the Senate to prevent a filibuster on the initial round, so the original Senate contribution to the conference committee had to contain a lot of goodies, just to get to the conference committee -- in order to be dropped.
In the flurries of lobbying activity, hospital advocates have suggested uninsured patients just appeared at hospital accident rooms, effectively causing other patients to subsidize them. That was somewhat true, but extending the idea to a claim the government was already paying for all indigent care, was a stretch because hospital cost-shifting was laying most of the cost on the private sector. To go further and proclaim that including indigent care under the insurance coverage umbrella would thus be cost-free, did really strain the facts. How could it be cost-free and still cost a zillion dollars? Right from the start, this proposal was making itself hard to defend.
 The sound-bite is: the Obama health reform proposal of 2009 will extend affordable health insurance to poor Americans (citizen), and save Medicare from ruin by cutting costs. Because this still won't pay the bill, the rest of the nation must get less coverage for more cost. 
|
So, at the end of September 2009, the country confronted multiple thousand-page bills from the House of Representatives containing wide assortments of liberal ideas, and a more conservative Senate proposal from Senator Baucus (D, Montana) representing the views of the Democratic caucus within the Senate Finance Committee. The British magazine The Economist promptly snorted; Senator Baucus' bill was "Half a loaf, half-baked." Since laws passed by strict party votes are in danger of prompt reversal when the other party next gains majority control, Senator Baucus had been struggling to achieve some Republican support but apparently decided bipartisanship was not worth the delay. In any event, the Senate's assignment was to get past a filibuster; the real zingers could come from Nancy Pelosi's House bill. Andy Stern the labor leader, had appeared on a television show offering no arguments at all, merely demanding a vote be taken instantly, presumably before public support eroded. Moderate House Representatives are characteristically most concerned with being turned out of office after passing a controversial proposal because they face election every two years. The much more liberal leadership of the House, with seniority because of their safe gerrymandered seats, are however more likely to honor extreme partisan demands. With a safe Democratic majority of the House, a few moderates could be spared to "vote their conscience".
Because the Senate thinks of itself as the sensible, deliberative body, oversight of law remains with its originating committee, to preserve the connection to the "intent of Congress". Because Medicare and Medicaid are amendments to the Social Security Act, the Senate Finance Committee has maintained jurisdiction over these three social benefit programs. A "unified budget" made it easier to shift one program's surplus to cover another's deficit. In the House, with turnover every two years, continuing oversight is mostly assumed by the Appropriations Committee, on the grounds that this is the only committee which reviews every ongoing program, every session. But the realities of the program mix with the quirks of the Senate, and for over forty years whatever the Finance Committee says about Medicare, pretty much goes. During the fall of 2009, this group of old colleagues could be seen on C-Span, gently joshing each other, and even more genially suggesting their disagreements. Each member of Finance belongs to several other committees, but on Medicare, they know their stuff and have a loyal staff to remind them of what they have forgotten. They considered 550 amendments to Obamacare, and stubbornly defended the right of each committee member of either party to be heard courteously, in spite of what must have been a wild frenzy of pressure by unions and other partisans, to be done with it. Their patient labors turned up one issue that party leaders -- especially the Governors -- probably wish they had left alone.
 Blow away the smoke. Obamacare is about fixing Medicaid without admitting who, or what, caused it to need fixing. 
|
| The nut of the matter. |
The fifty Medicaid programs are a big mess. They are run by state governments with Federal provision of at least 57% of the funds, and in some cases over 80%. Some states offer eligibility to those with incomes at only half of the poverty level, others go to several times the poverty level. Their tendency is to use the HMO model of healthcare delivery, but it is an individual state option. Minority groups absolutely hate HMO. The fraud level in Medicaid is by far the largest in the whole government. The quality of care is uneven, but it is always going to be somewhat substandard since it pays well below cost and deals with high-crime populations, amid uncomprehending chronic poverty. It attempts to deal with the deplorable psychiatric inpatient problem, which is in its present condition because of bungled regulation. Medicaid under-reimbursement is the main cause of hospital cost shifting, which causes still other distortions. And so on. If you search for an explanation of the bizarre statistics on infant mortality, the ranking of U.S. "health care quality" as 19th in the world, etc, the explanation is to be found right here. To the extent that statistics are not rigged in order to make certain countries look good, the poor rank of American healthcare reflects the sadly underfunded Medicaid programs.
Even the medical profession is largely unaware of Medicaid issues because most members of mainstream medicine have long stopped accepting membership in the program, in part because of its laughable reimbursement, but more importantly, the HMO organizational model makes it impractical to treat an occasional poor person free of charge and skip the paperwork. It, therefore, is sometimes true that some Medicaid physicians see nothing else. And finally, hear this: Senator Grassley muttered that 90% of the cost of Obamacare is aimed at fixing Medicaid, and no Democrat on the committee corrected him. When you get down to it, Obamacare is a very expensive program for making Medicaid what it ought to be, and definitely isn't. Originally confined to Maternal and Infant Care, its money is largely spent on nursing homes. This would make a perfectly plausible explanation for why it has been so hard to see what the new proposal is all about -- it's about fixing the old mess which state and federal governments created, while at the same time hoping to extend a similar program to the rest of the country later, as a "single payer" system. Senate Finance has a difficult tap dance with this one, but they have put their heads down and are plodding on.
 Eighty percent of the cost is devoted to fixing the flaws of Medicaid. 
|
| Senator Grassley |
Many unexpected developments are still possible in an on-going debate, but it seems timely to examine the Obama proposal as presently visible at half time, so to speak. What is so far proposed of consequence, and what problems would be cured?
Employer Mandates. First, nearly universal health coverage hopes to be achieved by mandates, making it illegal not to be covered, imposing fines for non-compliance. It does not seem extreme to predict a rise in the fines to a level where they support the rise in costs they provoke. That would serve the initial problem of pacifying the public during the early going, but ultimately justifying the Supreme Court assessment that it was a tax, not a penalty. Unfortunately for this idea, Justice Roberts stated in his opinion that the fact that the penalty was so low proved it was a tax. If the penalty tax was raised enough, it would prove it was not a tax, and therefore the universal mandate would become unconstitutional because the rest of the Court had already agreed that the Commerce Clause did not support it. Chief Justice Marshall once opined that "The power to tax is the power to destroy" which generates the justification that only a small tax is safely small enough to be a tax and not a penalty. It follows that while the Constitution permits the Federal Government to tax for revenue, it is not an enumerated power to tax in order to coerce or destroy. Justice Roberts may have been tipped off, but if not it was a shrewd guess.
Obamacare closes the safety valve that just about every poor person has long been eligible for Medicaid, but few of them actually join it until they get into a hospital and the social worker signs them up. The true antagonism of poor people to "Welfare medical treatment" has yet to surface into public view. Mandates are always unpopular, but back in Washington two competing ideas for mandates once headed for a conference committee. Because of the tax preference for the purchase of health insurance by employers, we still have a largely employer-based system, defining for poor people what normal health care looks like. As hospitals (responding to the shift of Medicaid costs to Medicare which they are forced to make) have increasingly shifted the costs of indigent care onto employer-based insurance, those employers who participate are increasingly anxious to make their competitors stop evading "their share". Unfortunately for this proposition, the non-participating employers never agreed to subsidize someone else, and do not feel bound by any moral strictures surrounding the demand of big business that their competitors are obliged to share a burden which big business decided to assume for its income tax benefit. If you doubt that small business and big business are competitors, just ask yourself what small retail businesses probably think of Amazon and Walmart. Then ask yourself whether very many small businesses benefit from ERISA.
Since almost all interstate employers already buy insurance for their employees under the coverage of the ERISA law, representatives of large employer groups want their competitors, especially foreign-owned, to experience equal expense. Big employers would thus be pleased with an employer mandate: employers who do not provide employee health benefits would be fined. Big employers are not so much threatened by little ones, as anxious to avoid government regulations which ultimately favor smallness as a preferred business model. By contrast, small employers are resistant to the employer mandate, amplifying the political perspective that increased cost would particularly hurt new employment in the present recession. Small employers enjoy and would hate to lose, the reputation of being the largest source of new jobs in our economy. Employer mandate might indeed ensure some uninsured people but the remaining uninsured would be unaffected. An employer mandate solves some purposes of big business but probably injures small business to a degree offsetting the cost-shifting argument. So, although an employer mandate was on the table, Senator Baucus proposed the individual mandate which Representative Pete Stark of Berkely, California had been advocating for years. That is, every person found without health insurance would be fined. Recall now, that Chief Justice Roberts introduced the qualification that the fine must remain small to be called a tax. Presumably, compliance would be even less than the widely-evaded mandate for automobile liability insurance.
One cannot leave the subject of mandates without the impression that there is some poorly understood connection with the Henry Kaiser income tax preference for employers who provide employee health insurance. Almost nothing can illustrate the intensity of warfare between big business and small business than this. Large employers definitely do not want to share this benefit with their smaller competitors, and definitely, do not want to say so in public. To the rest of the public, big business is taking the wrong side of the fairness argument, to say nothing of the Constitutional argument about equal treatment. But there is no other source visible for the seventy-year defense of the indefensible which has long convinced Congress that the tax inequity is politically impregnable, and cui bono will have to suffice. As long as this remains the case, there is some hope that some Congressman will be willing to fight it out.Individual mandate creates a somewhat different political problem of what to do about recalcitrants who are both sick and uninsured, who must now fear punishment as much as their illness when they appear for treatment. They are unlikely to forget which congressman voted to create the vexing outcome of fearing-to-seek-treatment. The Congressional Budget Office summed it all up: we started with forty million uninsureds, but it is most likely we will be left with thirty million uninsured (and now resentful) persons, including 7 million who are in jail, an equal number of mentally retarded or disturbed, and 11 million illegal immigrants. The very vocal remainder is hard to classify and hard to count. But the CBO is probably right, it's hard to see how insurance reform of any description will get the number much below 30 million.
 Give the tax exemption to everyone, or give it to no one. 
|
A second difficulty with the individual mandate is that it exposes the long-standing inequity in the Henry Kaiser tax law. The main reason we continue a largely employer-based system is that purchase cost is effectively reduced by the tax discount when an employer buys it for an employee. Self-employed or unemployed persons do not now receive this tax-discount. For seventy years it has been desirable to extend this tax exemption to everyone equally, both for fairness, and to create portability mitigating the pain of pre-existing condition exclusions. Pre-existing condition exclusion always existed, but it is the linkage to portability between jobs that makes it such a wide-spread issue. But the employer-based system might lose its main reason to continue, so that particular consequence has yet to be addressed. Inverting the traditional relationship between being sickly and paying higher insurance premiums has never sounded completely plausible, but we are now going to see what happens if we try it that way. Additionally, the political consequence of not equalizing the tax preference would get worse. Compelling millions to buy individual insurance, while at the same time denying them everyone else's tax exemption for it -- is not likely to survive long once it gets public attention.
Give tax exemption to everyone or give it to no one, or give it for a lesser amount, but give the same thing to everyone if you hope for re-election. While tax equity is not in the current legislation, it might as well be, and the CBO should be asked to score it as part of the eventual cost. And finally, no mandate in sight during a recession would insure illegal immigrants, who are a large part of the uninsured problem in certain regions. It is reported that sixty percent of uninsured persons are concentrated in Florida and the four states bordering Hispanic America, a fact that ten senators and several dozen congressmen are sure to notice. Proponents of amnesty for illegals have undoubtedly thought about this matter. Opponents of amnesty are apt to see immigration reform as just a way to cloak the costs of Obamacare as an unrelated issue.
Now turn to the other main objective of reform legislation, to reduce the high costs of medical care. The poster child of this objective, possibly the central issue agitating many politicians, is the approaching bankruptcy of Medicare. To skip over technicalities, accumulated subsidies of fifty years of Medicare recipients have created unfunded liabilities that make Medicare the largest single debtor on the planet, unless someone wants to compete with $250 billion a year. If you think about it, Medicare would have no debts at all if it were self-supporting. Until something is changed, the fifty percent subsidy of Medicare by borrowing from general tax revenues is steadily making the problem worse. The understanding of the public is just beginning to realize that Medicare is so heavily subsidized, and this is probably the main source of its popularity. Ignoring how this growing debt was created, it is accompanied by fifty years of promises to every citizen about what they are entitled to. Perhaps it was believed that an uproar over reducing Medicare benefits could be softened by burying it in a nationwide reduction of all healthcare costs, but half the cost of Medicare is a pretty big nut to bury, and fifty years of accumulated debt is just about impossible to hide.
In fact, such expansiveness provokes more suspicion that something is being slipped in by the back door. In angry town meetings which frightened congressmen, held during the August 2009 recess, one speaker after another went to the microphone and said something like, "I have excellent health insurance and I wish everybody else had it, too." Following which, something was immediately said equivalent to, "But don't you dare take my good coverage away from me to give it to someone else!" And not invariably, but often enough to make it emphatic, some would add, "I voted for you in the past, but I'd never vote for you, again." No doubt, every one of those congressmen was asking himself how the party leaders could have got him into such a fix. Why don't we try something else? Senator Baucus offered to pay for reform by putting a tax on health care providers, but every worried citizen quickly saw that taxing providers will raise costs, not lower them. Credibility is waning.
 The Affordable Care Act would cost a trillion dollars, and still, leave 5% of the population without insurance. 
|
| The Congressional Budget Office |
An adage is getting hardened: Increasing access to subsidized health care is not compatible with cutting costs, and won't even produce universal coverage. It is increasingly difficult for presidential oratory to reverse that opinion. The Congressional Budget Office has not pronounced the Obama plan to be an unachievable goal, but after examining an enormous pile of studies, it amounts to that. They simply said it would cost a trillion dollars, and would still leave 5% of the population uninsured. In one sentence, the CBO probably killed a lot of strategies.
Still, the Obama administration gamely plunges ahead, seemingly forgetting that defeat of the Clinton health plan was followed by a mass eviction of incumbent congressmen; by their analysis it wasn't a bad plan that made trouble, it was failure to pass the bad plan, which it must be recalled was a universal HMO system. The Clintons avoided public defeat by pulling that legislation away without a floor vote. But at least they did escape the backlash against what would then have been a ruinously unpopular program. It is not unrealistic to surmise that Obama would never have been elected to a first term if Clinton had not backed away from his version of healthcare reform. Right or wrong, some Democratic congressmen are certainly toying with that heretical idea.
For one thing, the public has always been bewildered by the need for such a rush, such a collision. We are now fighting wars and struggling with the worst depression since 1930. All of those major projects are going poorly. Why in the world would we believe that reforming health care is our major priority, right now?
The following section closes the discussion of the main features of the Obama plan and ignores thousands of pages of legislation not yet implemented. The law is mainly made up of earmarks, boondoggles, and in consequence -- the usual contents of an annual budget reconciliation act produced at Thanksgiving or the day before Christmas. We hear nothing about tort reform, which at most will produce a study or a pilot program. Nor the public option, which Senator Baucus said cannot pass the Senate, and about which former Senator Dole said he heard, but scarcely would believe, that the Public Option was just a smokescreen intended to distract the public while the rest of the bill slipped past the uproar of Public Option getting defeated. The fate of the expensive but inconsequential computerized medical record would once have depended on the precarious health of Senator Byrd of Virginia, who had long held a stranglehold on government computer procurements, but which now mainly perplexes us as to what to do with it. Blue-sky yarns about the value of the Electronic Medical Record abound. But except for large group practices which do seem to need it, most doctors see EMR as an expensive way to add two hours a day to their already overloaded workload and badly compromise patient privacy in the process.
Picking Out the Raisins From the Pudding
There appears no better blueprint for the 1993 healthcare reform legislation (commonly called "Clintoncare") than Jacob Hacker's 1999 book The Road to Nowhere. If President Obama did not use this same roadmap for the "Obamacare" health program, it still remains quite a good description of what he did do. His following this earlier playbook would plausibly explain much that is otherwise mysterious.
The Hacker book was originally an academic thesis written several years after the (Hillary) Clinton Health Plan experienced ignominious disappearance in the halls of Congress. By then, the Clinton episode of 1993-94 was quiet and forgotten, so participants probably felt it was safe to describe big-shot politics to a college kid writing a thesis. The resulting book was easy to follow, had a ring of authenticity, and advanced the author's career. Advanced it so much the same Jacob Hacker later became visible near Democratic policy circles, even seemingly advising political deals, even though strangely quiet, lately. The similarities between the Obama initiative and Clinton's earlier strategy in Hacker's book, are striking. However, a judgment must be suspended whether to frame it as a cautionary tale, or a guidebook. In fact, the possibility that Mrs. Clinton plans to use the blueprint a third time produces a strange fascination among even her enemies.
 1. Pad anything into Senate and House bills. 2. Send the padded bills to a conference committee. 3. Delete all but your own ideas. 4. Ram it through. 
|
| The Clinton Strategy |
Boiling it down, the (Bill) Clinton strategy was to confront a House-Senate conference committee with a vast pile of often conflicting proposals, sent to a conference committee for a proposal to reconcile inconsistencies. In fact, a coherent proposal could not emerge from a Clinton bill, until the President sent his list of proposed deletions to that conference committee. After trimming to its essentials, the conference committee reconciliation would then return for House and Senate approval, probably against some holiday deadline to quash objections. The process would resemble picking out the raisins from a pudding, combined with the nuisance of buying off a few soreheads, except for one thing. The Executive Branch deftly acquires more power over legislation than the Founding Fathers ever contemplated. Michelangelo's remark, that carving statues is just a matter of throwing away what you don't want, is bitterly appropriate here, especially from the viewpoint of those who thought they were elected to write laws, not follow orders. On the other hand, this approach favors a party with safe seats from concentrated urban districts, tending to be more compliant to party bosses .
In a technical sense, this process is more equivalent to a line-item veto. (A line-item veto, by the way, is something Congress repeatedly refuses to grant). It's hard to oppose an omnibus bill until its outline appears, and this Michelangelo process tends to obscure the tone and central theme of legislation until the last possible moment. From the point of Conference Committee forward, passing it back for ratification becomes a matter of rushing it ahead of criticism, and indirectly lessens the power of public opinion. Nor would be the first time a few little extra zingers, never discussed by either the House or the Senate, got slipped into a conference bill, which is typically several hundred pages in length. And the timing for the release of the omnibus legislation could be selected, quite likely the day before Thanksgiving or Christmas when newsmedia was away from work. Or else after a long series of preparatory news events, building public expectations before a spectacular revelation day. But it is a mistake to focus on the press as being hoodwinked. It is the other Congressmen, the ones who ultimately don't get what they were promised.
And finally, unexpected events can intervene, as Scott Brown's Senatorial election did in this Obamacare instance. A clever scheme got suspended in mid-air by the death of Senator Edward Kennedy. The bill had been passed by the Senate, but not the House. The House bill was so different it would require reconciliation with what by then would be a different composition of the Senate, and therefore could not pass the Senate a second time. So, a bill identical to the Senate version was jammed through the Democrat-dominated House, no amendments permitted, no conference committee needed to reconcile two differing bills. Unfortunately, the original plan was to include some provisions purely for the purpose of obtaining a Senate vote or two. The original plan was to be that "deficiencies" would be remedied by some raisins tucked in the House bill, which of course never came up for a vote. Thus the resulting legislation is the pure Senate version (with all its undesirable features remaining) and we may never know what was in the unpassed House bill that might have repaired unspecified Senate flaws. After all, this trickiness, does anyone wonder why so many Congressmen are dissatisfied with the result?
Looking back, it is hard to prove how much of the Clintons' original strategy was adopted by Obama, or how much influence Hacker and Hacker's book had, until someone on the inside writes another book and tells us about it. But the congressional strategy of the Obama Health Plan proposals does sound very similar to what we should probably give the name of "The Arkansas Strategy". That strategy would certainly explain a great deal of what happened; it scarcely matters how much the similarities were accidental and how much they were following the same playbook. Except, of course, if some of the participants decide to run for office in the near future, and try to do it all, a third time.

|
| Senator Edward Kennedy |
Senator Edward Kennedy's impending death, Senator Byrd's incapacity, and the contentiousness of the health reform topic always made it uncertain a 59-vote Democratic Senate leadership could assemble 60 filibuster-proof votes in favor of any healthcare proposal; one betrayal and you've lost. The Democratic Massachusetts legislature took away the right for Republican Governor Romney to fill a vacant Senate seat and restored it for a subsequent Democrat governor. In circumstances like this, every single Democratic senator can hold a proposal for ransom, while every single Republican senator will unite in opposition. When the majority shifts Republican, which could be rather soon, the roles will be reversed in an almost certain effort to repeal whatever passed. The public was left wondering whether healthcare legislation was worth hampering our interests in Iraq, Iran, Afghanistan, Syria, immigration reform and the national debt. The Democratic Congress had to worry it was not worth the political damage from hammering it through. They might also worry that the Supreme Court might be drawn in, expressing some unwelcome Constitutional viewpoints. It's really hard to know what to wish for.
|
| Bob Dole |
Along the way, former Senate Majority Leader Bob Dole appeared on television and revealed a different insight about Senate behavior. Senator Baucus told the press that something called a Public Option could not pass the Senate, so he was not including it in his proposal. Extreme left-wing members of the Democratic party said they would "take a walk" if the Public Option was dropped. But although it was dropped, it was included in the House version and might thus have been restored in the conference committee. This "Montana" maneuver removed Public Option from Senate debate, still hoping to preserve those 60 votes. Under the circumstances, it isn't even necessary to remember what the Public Option was, but essentially, Public Option was a proposal for the Government to go into the health insurance business itself, in order to put overwhelming pressure on the insurance industry. In 1965 this was impossible, in 1992 it was unprepared for, in 2009 it was merely chaotic.
It is widely rumored the Public Option was a punishment for the reluctance of the health insurance industry to cooperate more fully with the President, or at least a threat of what could happen if they didn't soon cooperate. Indeed, you have to question what the attitude of the Insurance Industry really was, in a proposal which would greatly diminish their control of insurance. Karin Ingaglio, the chief lobbyist for private health insurance companies, admitted to the National Journal that her group had contributed millions of dollars to the Tea Party, leaving it unclear whether she was playing both sides of the street, or else hoping to defeat the Republicans with a third-party, Tea Party, distraction. Bob Dole was a gracious, gentle old man, musing about what might be going on. You don't suppose, he mused, the Public Option might be nothing more than a red flag in front of a bull, to be surrendered with a great show of disappointment. But actually, just a feint creating an uproar, to divert attention from the real zingers in the rest of the bill, which can then pass through unnoticed. But, no, Bob Dole didn't really imagine such a thing. It was just a wild thought he happened to have.
Political observers agree that presently rancorous Congressional partisanship is the worst in a century, and it is not shared by the public. Just about everyone in the political class sees gerrymandering as the main cause. Changes in the ways voter redistricting is conducted, some say the use of computers, has made gerrymandering much more effective. When numerous safe seats arise in this way, it is only a matter of time before the Legislative seats are filled with heedless, reckless partisans, beholden to no one. But it is just as bad, if the seats are filled with party hacks, forever obedient to the unelected rulers of urban political machines (leaders of party machines seldom run for office.) The seniority system takes over, and safe-seat partisans get control over Congressional committees and party discipline. This happens to both parties because incumbents from both sides unite to achieve it. But urban districts are harder to split into party lines, so states containing large cities tend to present a permanent disadvantage in numbers for Democrats, although uniform composition makes for much greater partisanship. Contestants for the dwindling number of uncertain districts are thus forced to act more cautiously, thus tending to seem more competent by the press and the public. But even if elected, they are powerless in the face of the more unrestrained partisans who control internal power plays, and who also tend to be long-term incumbents from safe seats. As a consequence, moderates are more likely to be singled out for sacrifice in the following election.
Scientific gerrymandering has certainly coarsened and hardened the political atmosphere, considerably reducing public control of its representatives. It should also be noted that Senate seats cannot be gerrymandered, but state legislative seats definitely can be, leading to a coalition between state legislators who are almost always party hacks, and U.S. Representatives, who are increasingly so. It is said that in New Jersey and Florida, it is possible to predict the next ten years of politics with precision if you only know how the gerrymandering was arranged. The Senate could probably devise a Constitutional amendment to fix this problem, with no chance of passing the House or getting ratified by the States. Therefore, the present main hope for representative government lies in the national party leadership of some party, intervening into the party nominations for safe seats. Even that, would take extraordinary luck and agility. It remains to be pointed out that 2020 is the upcoming year for a census, 2022 for redistricting.
"They Don't Make That, Anymore"
They Don't Make That, Anymore These words from the nice young lady in the drug store, left me astonished, baffled, bewildered, and angry.
Although I am retired from the practice of medicine, my limited license permits me to prescribe ethical drugs for myself. I had not realized, until that very moment, that to some extent it also isolated me from the experiences of my fellow patients. Let me explain.
The drug involved was tetracycline, which I had surely prescribed a thousand times, and to which I had a sort of loyalty growing out of the fact that I took it myself. In the days when I was a college student, I came down with a form of pneumonia that involved a lot of coughing, like whooping cough. It was then called virus pneumonia because it was somewhat different from ordinary pneumonia, even though it was called Primary Atypical Pneumonia in polite academic circles. Eventually, we learned that its cause was neither a virus nor a bacterium, but rather something in between in size, called Mycoplasma. All of this is important to know, because it tends to appear as a question on a certification examination, but the fact of the matter is, it was a disease for which there was no effective treatment. We could cheer up a little to know that of four hundred recruits at an Alabama training center who came down with it, only one died. On the other hand, Legionnaire's Disease is also caused by a Clamydia and lots of them died, probably because most of them were older. But no matter, in 1944 there was no treatment, and I can tell you it is very unpleasant for a very long time, no matter how young you are.

|
| CAT Scan |
In 1950 I got it again, but this time I was a doctor and knew there was a good treatment. It sounds strange to say so, but I was sort of happy to be able to try out the new medicine, which was then called Aureomycin because the powder was golden yellow. Aureomycin was a trading name, with a patent, and when the patent expired the generic form was called Tetracycline. It worked just fine, and in three or four days I was out of the hospital, perhaps a little weak and shaken, but cured. Incidentally, I discovered an interesting feature of the disease which I believe has not been previously reported. It had long been observed that the chest x-ray showed pneumonia while the stethoscope perceived very little abnormality, a feature which disconcerted those of us who were concerned with the cost of medical care, particularly members of a generation who felt sniffy about the dependence younger physicians displayed for x-rays, and nowadays for CAT scans and MRIs. Unfortunately, in this particular instance, x-rays are clearly superior to stethoscopes.
My third time around for "viral" pneumonia was a few years later; I was sitting on a park bench near the hospital when I recognized the old symptoms were coming back again, so I went straight to the x-ray department and had a chest x-ray less than an hour after the symptoms appeared. I planned to have an x-ray to prove it, go get some tetracycline and be all better over the weekend, with a rollicking anecdote to tell doctor friends about. Unfortunately, the x-ray was normal, so I was admitted into the hospital to see what was wrong. The next morning the x-ray showed a densely consolidated lung, so it had been viral pneumonia all along. And so my old prejudices were vindicated; it was possible to be too quick to order x-rays after all. Unfortunately, the extra twelve hours without treatment allowed me to get a lot sicker than I had to be. I think I know this because, doggone it, I developed the same disease several decades later, took no shortcuts to the drug store, and was fine in a couple of days after I immediately started taking tetracycline. You could say this strange recurrence of Mycoplasma pneumonia over one-lifetime sort of illustrates how medical care of the disease has become progressively cheaper. Instead of a month in the hospital with no treatment, it was now a matter of skipping the stethoscope, skipping the x-ray, skipping the hospital, and just swallowing some cheap tetracycline capsules. You have to have the nerve to do it, of course, and ethically you probably only have a right to do it to yourself, knowing the risks and being willing to accept them. There is, however, one flaw in this story.
When Aureomycin first emerged from the clutches of the FDA (and well before that accursed Kefauver Amendment), it seemed astonishingly expensive. Because I knew what it weighed (250 milligrams per capsule), and I knew what gold cost ($35 an ounce), it was easy for an idle mind to calculate that Aureomycin cost more than gold. Gold now sells for $1700 per troy ounce, so you could take this story in the direction of inflation. I rather prefer to take it in the direction of nominal dollar amounts, because Aureomycin retailed for $5 a capsule the third time I had the disease, and $1 per capsule when it lost its patent and became tetracycline. The fourth time I had the disease, I bought a container of fifty capsules for 76 cents. But as you have already heard, by the fifth time I couldn't buy it for any price, because everybody had stopped making it. Since my view of the economics of useful commodities is that low prices will only cause shortages if there is artificial market interference, the usual cause of shortages is rationing. Somebody who understands the 2500 pages of Obamacare better than I do will have to tease out the way rationing has caused shortages of tetracycline. And when they are done confusing the public, let them explain why you also can't buy KMnO4 crystals (potassium permanganate), which has cured more cases of athlete's foot for twenty cents, than all those cans of stuff in spray canisters.
An Unending Capacity to Generate New Problems
There is a fair amount of seemingly unrelated detail until we reach the point of this article, where we conclude it really is possible to design and pay for lifetime health costs with the tools we already have, using individually owned lifetime policies. As a part of that, it really should be possible to substitute cost shifting between the youth and the old age of one person, rather than the present kind of cost shifting from one person or group to somebody else. People don't mind taking from one of their pockets and putting into a different one. But fierce possessiveness appears when you shift from my pocket to your pocket, and the health system is riddled with it. "Riddled with cost-shifting" seems to imply underhandedness. In fact, only the simplest businesses could survive without such flexibility. The problem with cost-shifting in medical care is there is so much it, even carried to the extreme of performing carefree, with blithe indifference about how to pay for it. Just review how accustomed we have become to cost shifting as the only possible thing to do.
From the outset, Blue plans announced their business model: patients in the private rooms supporting the care of indigent patients on the wards, up to then entirely supported by the charity. Plus a third, intermediate class of say ministers and school teachers, called semi-private, who were financed on a strict break-even basis. Summary: rich people supported poor people, and the semi-privates broke even. At first, there was just a handful of semiprivate, but after a decade or so, just about everybody was semiprivate, defined as two strangers in a room. Blue Cross had an enormous unintended effect on hospital architecture. When Medicare and Medicaid adopted the same philosophy, the semiprivate room became the standard. If the rooms were small (and cramped) the nurses didn't have to walk so far, but the main driver was the insurance reimbursement formula, which was based on square feet of floor space. A square foot of such space was used as a cost basis for non-patient space in the overhead formula. Eventually, hospital architects were receiving demands for bizarre room sizes, in order to affect the reimbursement formula. The tail was beginning to wag the dog.
t During that era, charities were payers of last resort, unless creditors were stripped by bankruptcy. Furthermore, to provide a full range of services, some services lost money, subsidized by other departments which generated a profit. Any corporate executive could tell you what came next: the profit centers start to boss the losers around. In group practices, surgeons generally still subsidize primary care ("the feeders"); state Medicaid is roughly 50% subsidized by federal Medicare, and after hospitals are paid, underpayment by Medicaid is balanced by the hospital from other sources, once again mainly from Medicare until payment by diagnosis (DRG) came along. It is when one insurance competitor is forced by internal hospital cost-shifting to subsidize its rival, that most of the outcry is heard. Employer-basing leads to different subsidies between insurances, and by a two-step process, one competitive business subsidizes its fiercest competitor. Generally, a business does not care what things cost, so long as competitors must pay the same price. In the eyes of business, trouble comes from unequal cost-shifting. Its mere suspicion is almost as bad. Working-age people subsidize the generations too young or too old to work. That is obviously what must happen indirectly and unofficially, anyway. Cost-shifting is a normal business practice, an absolutely necessary one, but the cost shifting of hospital costs is almost beyond belief. Because now, no one can tell what anything costs, and because patients who are business employees will reflect the attitude that the absolute amount doesn't matter, only that competitors must pay the same. In short, cost rises meet little resistance.
What brings the matter to a crisis is payment by diagnosis, where it doesn't matter how long a patient stays or how many tests he has, the insurance payment to the hospital is the same. Added to a determination by Medicare to cut costs, the result is that the profit margin for inpatients is around 2%. From the payment designers' point of view, it's an excellent rationing system. But it isn't, because hospital architects are directed to shift their lavishness to service areas with greater profit margins, like emergency rooms and satellite outpatient clinics. The next time you see a building crane at your local hospital, just ask them what kind of building they are putting up. Having spent a fortune twisting hospitals into one kind of shape, the reimbursement system is twisting a new shape, and rather oblivious about it. At the same time, two-bedrooms are being converted to one-bedrooms to attract a carriage trade and justify a higher price. Maybe, just maybe, the bed capacity is somewhat smaller at the end of responding to a pitiful profit margin for inpatients. Changing demographics are also a factor. Trends toward unsustainable cross subsidies grow steadily larger because the contribution of working people is certain to get proportionately smaller. Extended longevity increases the proportion of young and old dependents, boosting the costs of working people by the fact that their shrinking proportion must ultimately pay for all of it. Ultimately, all hospital revenue originates with the working segment of the population. Parents pay for their children, and payroll deductions pay for the elderly grandparents. Working people are supporting it all. Let's not overstate: disappearing infectious diseases reduced the mortality and hospitalization of working people, too. The elimination of polio and tuberculosis was a dramatic godsend but made it harder to finance a general hospital, because of the shrinking client base of employed people. The way things are going, health costs should eventually concentrate in the first and last years of life, with hardly any serious illnesses for the people in the middle years of life who ultimately pay for every bit. Hospital cost-shifting can not indefinitely support its own system because working people will have so few medical expenses it becomes impossible to hide very much within them. If you want to know why payment by diagnosis was welcomed, just reread the last three paragraphs. Unfortunately, if payment is based on diagnosis, it doesn't matter how many x-rays you have, or whether all the door handles are polished brass. We badly need a new way to charge inpatients, and just about every system has been tried. Unfortunately, it took a long time to get rid of payment by the square foot, and it will take a long time to get rid of payment by two hundred very approximate diagnosis groups, or DRG. The very least that could be done is to substitute a better diagnosis code, like SNOMed, for the private ICDA, so that payments are seen to be driven by the right diagnosis, which might tell planners something useful.
 How could we have created individual policies that failed to reward customer loyalty with guaranteed renewal? Or monopoly status, to companies without guaranteed issue? 
|
| Lost Opportunity |
 Medicare would pay terminal costs as before, but be reimbursed by the escrow fund. 
|
| Transfer Vehicle |
 Malpractice costs are disproportionately concentrated in Obstetrics. 
|
| Who is doing the suing? |
The second redirection of attention would be to campaign to lower the age at which American women have their first child, greatly reducing neonatal problems, including infertility measures and congenital malformations. Absorbing the cost of having a baby ought to assist this effort, otherwise highly desirable on purely medical grounds. Unfortunately, our system of graduate education and career advancement will incentivize timing conflicts with biologic goals. Society will have to work these conflicts out in its own way, but at least we can adjust health insurance timing to be more in keeping with societal trends.
Finally, it should be said that the Health Savings Accounts are a vastly simpler way of paying for health care than using the service benefits approach, and the payment system greatly needs simplification. Using a high deductible has the potential to preserve market benchmarks for prices which are otherwise going to induce unworkable price controls, permanently. The system of "first dollar coverage" was accelerated by a wish to include as much as possible under the Henry Kaiser income tax evasion, and it will return if we neglect to correct that flaw. Experience with Health Savings Accounts has demonstrated as much as a 30% reduction in claims costs. Linking market-set outpatient costs to the same services when provided to inpatients should be an adequate price control for helpless sick people since an improved system of diagnosis-related groups should accomplish most of it. But the main advantage is to reduce these fund transfers to money without health attachments, to make unification and substitution more plausible. That is, to eliminate "service benefits" and not replace them with "diagnosis benefits" except for helpless bed patients. A return to dollar indemnity is greatly needed, although perhaps not totally.
To a considerable degree, service benefits are in conflict with indemnity benefits, in a manner resembling the conflict between debt and equity in the financial sphere. At some point, there must be a reconciliation between these two ways of paying for things, especially by keeping indemnity consistent with market prices. The best one can hope for is to shift the location of the interface between service benefits and indemnity, bringing the friction out into public view, and equalizing the power of the sponsors. Therefore, the best place to hold the debate is to treat diagnosis groups as inpatient service benefits, and outpatient costs as indemnity. With reasonable exceptions, of course. One of the main mistakes of the DRG system was to extend it to every inpatient. Inpatient psychiatry should be paid for as if it were an outpatient service, and chronic diseases such as Alzheimer's disease should also be excluded from DRG as well. Emergency room visits should be separated into two groups as well (admitted to hospital and discharged home), with reimbursement slanted to reduce the incentives for unnecessary use of the Emergency room, not the other way around as it is at present. The whole trick here is to see the double reimbursement situation as an opportunity for constantly rebalancing the two approaches, rather than allowing it to be pounced upon as a loophole.
We started by saying these issues should be chipped away, during the period when more important issues are being addressed head-on. But the list of small issues is a long one, providing ample opportunity for trade-offs in ambiguous opportunities. More than anything else, the endless capacity to develop new problems demonstrates the need for careful construction of an institution to serve as an informed and trustworthy umpire.
Classical Health Savings Accounts (C-HSA)
Reconstructing the Reconstruction
In a new system involving three hundred million personal situations, some difficulties take time to come to the surface. Other crises can be anticipated in advance. It's like the Salvation Army or the Red Cross: mostly, you get an appeal for donations just before Christmas, but sometimes there's an emergency that comes unexpectedly. Three months before implementation, Obamacare's first crisis seemed somehow steered at small business, since compulsory health insurance for big business was postponed for a year, whereas individuals and small groups were relentlessly ordered to implement on time. Which was it? A rebellion by big business to be pacified, a rebelliousness by small business to be whipped into submission, or a need to have the two separated in time? In 2013 there are only two important elections, for Governor in New Jersey and Virginia, whereas 2014 will have many elections. An administration which seemingly puts politics ahead of every other consideration, undoubtedly takes the calendar into account. The thought suddenly occurs: is this what we can expect in constant succession for the next three years? Are tidbits of information to be timed with current events, while the great mass of information is withheld about the true scope and direction of some new proposal? Even worse, is health insurance regulation to be played off against a similar game in financial regulation, using the issue of Dodd-Frank regulations as a foil? By the way, what happens to our national attention when Syria, China, North Korea or Iran act up? And finally where do we go if the bond market gets fed up with its tormentors, and runs away with interest rates? To be sure, politics ain't beanbag, but does it have to be played like a children's game?
Community rating is a term of art for everybody to pay the same premium, regardless of previous health status. People in bad health get a big bargain, people in good health pay more than their share, and squashing it all together leads to a community rate. Not for everybody in the community, but for every member of an employer group, working for the same company or bargaining unit. By definition, these are healthier people because they were selected for it when they were hired, and for the most part they remained healthier than average just because they were able to work. Inevitably, industries with many women employees had more pregnancies, heavy industry had more accidents than white collar businesses, so community rating worked best in large corporations, while small businesses knew their employees personally and could manipulate the policy benefits to get the best rates for a small minority. Stated broadly, big white collar businesses got the cheapest community rates, heavy industry got higher rates, small businesses got still higher rates, and individual policies had the very highest community rates. When you squash a lot of communities together you might get a real community rate, but competition between insurers soon forced a graded outcome. The Affordable Care Act anticipated that it might at least achieve regional community rates, and still be able to absorb the differences caused by pre-existing condition exclusions, age and gender rate differences, and other purely insurance responses to public demand for truly uniform rates. Actuaries have computers and lots of data at their disposal, so presumably they advised the politicians it was possible to design a system with close-enough-to uniform premiums that any remaining flaws would be excused at the next election. The arithmetic is not so hard, it is the assumptions you have to make.
Whether you are an actuary or a politician, you have to make the assumption that the people who must pay more, will be willing to pay enough more. For that calculation, certain benchmarks are available. There are 42 states which require that the premiums for the subscribers who pay the most, may not exceed five times the premium paid by subscribers who pay the least. State insurance commissioners are charged with protecting the public against insurer bankruptcies, and apparently it is the collective judgment of such officers that companies which allow much greater premium disparities are in risk of consumer rebellion, potentially leading to collapse of the insurance system even for those who are willing to pay more than a 500% premium for it. The term in common use is "unsustainable". Perhaps the nation is fortunate to have had the example of a state which actually attempted to run a system of absolute community premiums.
New York, New York The Mario Cuomo administration of New York attempted such a system in 1992. Premiums rose by more than 30% the first year, enrollment fell by 38% in three years, and among individual subscribers the number fell from 1.2 million to 31,000. For some types of policies, every single insurer in the state abandoned the business.
To return to the present situation, it would appear that individual and small group subscribers were facing premiums much higher than they were willing to pay, and alarming numbers of them indicated they would rather pay the fine than accept the overcharge. At present, these people are being told to take it or leave it, presumably counting on political sympathy plus subsidies to hold them there. They would have to wait at least a year, and very likely longer, to be able to compare their "community rate" with the "community rate" for big business. Even then, there is considerable possibility for creative accounting measures to obscure a fair comparison.
In addition, there is the possibility of U.S. Supreme Court action, questioning the right of the Executive Branch to change a law signed by the Legislative Branch. Even beyond that point, there is a question of equal justice under the law for doing so. In view of the likelihood that it is far easier to implement a few large groups than many small ones, the reasons given for partial postponement seem to require considerable argument to be convincing. The number of instances in which a Constitutional challenge to some feature of the Affordable Care Act is possible, seems to grow regularly. The Court won't hear a case until someone files it, so the Judicial option appears to lie with the opposition.
Only Three Things Wrong With American Healthcare

|
| American Healthcare |
Although Congress is offering several thousand pages of proposals for healthcare "reform", none of them even mentions the three main difficulties, to say nothing of fixing them. Let's be terse about this:
1. Health insurance is fine, but if you make it universal, there is no impartial way to determine fair prices. Somebody must haggle with the vendor in order to introduce the issue of what is the service worth? The customer doesn't care what it costs to make, or whether the vendors are being paid fairly. If everyone is insured, no one cares what it costs. Not only do all costs rise, but they rise without coordination, without a sense of what each component is worth, relative to alternatives.
2. Employer-based insurance is fine, but it ends when employment ends. You just can't stretch employment-based insurance because you can't stretch employment.
3. State Medicaid programs are fine, but just about all fifty states are going broke trying to pay for it. Extending it to more people by raising the income limits just makes things worse. Items 2. and 3. are related. Trying to do both -- expand Medicaid as employment shrinks -- during a recession is incomprehensible. Item 1. (price confusion) gets drawn into this because the States try to pay less than it costs, hoping to shift the deficiency through hospital cost-shifting, utterly confounding the information which prices provide. The doctors have no way to tell which is the cheapest approach to a problem, so they don't try. Without control over prices, we can only control volume.
That's really all there is to this mess. Not one word of the current legislation even mentions these problems, so of course the legislation blunders. Even a child can see that compulsory expansion of benefits to universal coverage will fail if you can't pay for what you already have. No one will make sacrifices for a new system if the sacrifices seem futile. They are futile, so leave me alone.
The current administration has been compared with bank robbers who see they are trapped and decide to shoot their way out. Let's see them try to shoot their way past the first Tuesday after the first Monday in November.
What Obamacare Should Say But Doesn't
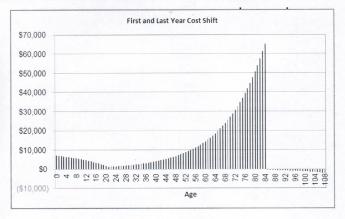
|
1a. TAX EQUITY. All tax exemptions stimulate overuse because they amount to a discount. For example, federal tax exemptions now mainly extend to two consumer purchases: health insurance and home mortgages. We currently have national crises in both at the same time. The tax-subsidized home-mortgage housing bubble played a major role in the 2007 financial panic, while tax-subsidized health care threatens to lead health costs into a second unsupportable bubble. Higher education seems to be going the same way, and it becomes difficult to imagine what would result if two or three of these bubbles merge. The expression "Children playing with matches" comes to mind. Giving a tax advantage to one group but not to its competitors is essentially just a variant, containing the paradoxical advantage that the competitors will object to it if they can't extend it to themselves.
Giving a tax subsidy to employees but not to self-employed or unemployed persons nevertheless created a uniquely American system of employer-based health insurance, and lobbying now perpetuates this rather odd system. Noting the allegedly temporary origins of this tax quirk (as a wartime expedient) merely dramatizes its lack of justification for seventy years afterward. It should not be necessary to describe collateral damage like job lock and internal hospital cost shifting. The issue of equal justice alone should be enough to justify the abolition of this unfairness. To mandate individual coverage but differentially exclude large subpopulations from tax exemption, is to invite a Supreme Court case. And since such a law has been passed, the sooner a damage case is granted certiorari , the better. To achieve equity, it does not matter whether tax exemption is given to everyone, denied to everyone, or limited to part of the cost (reducing the exemption for some, partly extending it to those who do not have it). Any choice between these three would make it equitable, although gradual elimination would be better, still.
 If health insurance is mandated, its tax treatment must be uniform. 
|
| Hidden Cost |
Once the tax is equalized, this proposal clears away the main obstacle to
1b. INDIVIDUAL OWNERSHIP OF HEALTH INSURANCE POLICIES, already proposed in Congress; but seemingly without hope of adoption. Determined opposition from the current owners of "self-insured" groups, the employers, or the unions who have acquired this function from employers. Since most such arrangements are de facto "administrative services only", insurer protests of higher administrative costs for individual ownership are often just relics of ancient combat between Blue Cross and commercial insurers.
Regardless of the internal structuring of incentives, healthcare reform cannot be permanently settled without individual ownership. It must be understood, however, that eliminating the tax preference could be resisted at first by patients who acquire it, because of fear the eliminated tax would in some way be shifted to them. That need not be true if consideration is given to the relative size of the losers and gainers. Since the membership of group policies greatly outnumber individual policyholders, the redistributed revenue cost of tax equity would be considerably smaller than 50/50. The CBO should provide a sliding scale estimate for negotiating purposes.
1c. ENCOURAGE WIDE-SPREAD DIRECT MARKETING OF HEALTH INSURANCE. Since Health Savings Accounts and Catastrophic High-Deductible Health Insurance are libertarian ideas without religious overtones, it is uncomfortable to advocate them as mandatory, even passing laws to that effect. However, the libertarian doctrine does not seem to preclude creating incentives for universal adoption. This doctrinal attitude imposes slower adoption than mandating them, although a better product result from more trial and error as the idea spreads. Therefore, readers may be surprised to see me advocate electronic insurance exchanges as a way to speed up trial and error spread of the idea's adoption. It is a way of preserving the flexibility of deductibles, benefits, alternative uses of surpluses, and vendor arrangements. It is also a way of narrowing the conflict with the Tenth Amendment, combining state regulation with inter-state marketing. If multiple alternative details prove necessary, direct computer marketing would be a quick way to discover what the permissible alternatives would be. Finally, the widespread examples of other interstate marketing can be employed to search out how to convert marketing from intra-state to interstate, rather than assume certain commerce is inherently (and permanently) interstate or inherently within-state.
An accidental feature of Health Savings Accounts is that the account can be growing for a number of years before the re-insurance feature is frequently needed. Indeed, young people may need a certain form of reinsurance protection and a different form as they grow older. The important feature is to have permanently stable savings vehicle in place while different forms of re-insurance are proving themselves. It seems heresy to say so, but we might even discover niches of the marketplace where first-dollar coverage or service benefits have some useful temporary role.
 The States Are in the Road 
|
1d. PRE-EMPT STATE LAWS WHICH INHIBIT CATASTROPHIC COVERAGE. State mandated benefits now severely limit high-deductible insurance in many states, and are the main reason Health Savings Accounts have been slow to spread. The provisions of ERISA shield employer-based health insurance from the unfortunate health coverage mandates in question. ERISA could not have been successful without this pre-emption, so unions and management unite in absolute concern to isolate ERISA from congressional meddling, although for different reasons.
1e. REVISIT McCarran FERGUSON ACT . This act effectively makes the "business" of insurance the only major industry restricted to the state rather than federal control. It should be amended to permit the sale and portability of health insurance policies across state borders and interchangeability of individual policies when people change state residence, thus greatly increasing competition and reducing prices. Once more, present law discriminates in favor of the employees of interstate corporations, who are also exempted by ERISA.
1f. MANDATE DISPLAY OF DIRECT COST MULTIPLES NEXT TO PRICES (FEDERAL PROGRAMS ONLY) (whenever prices are displayed, as in bills, price lists, etc.) FOR ITEMS COVERED BY HEALTH INSURANCE. Some high mark-ups are justified, but the public has a right to criticize them. This would not prohibit, but would considerably hamper, cost-shifting. It should be presented to provider groups as forestalling the prohibition of cost-shifting because of abuse. For this and other reasons, it would enhance provider competition.
1g. REIMBURSE HOSPITALS ONLY ON RECEIPT OF ASSURED POST-DISCHARGE HANDOVER OF MEDICAL RESPONSIBILITY (FEDERAL PROGRAMS ONLY). Unfortunately, hospitals do need increased incentive to improve post-discharge communication, which now increasingly occurs on a Saturday. Payment by diagnosis, otherwise a seemingly attractive idea, results mostly in sequestration of medical charts within the accounting department. That's undesirable at any time, but is most destructive at the vulnerable moment of hand-over.
1h. Similarly, REIMBURSE HOSPITALS FOR LAB WORK ON THE LAST DAY OF HOSPITALIZATION ONLY AFTER DEMONSTRATION IT HAS BEEN REPORTED TO A RESPONSIBLE PHYSICIAN. Such lab work, frequently obtained within hours of discharge, is sometimes overlooked and may even be unobtainable for the previously mentioned reasons, which in this case also apply to the hospital's own physicians.
1i. RESTORE ORIGINAL FORM OF PROFESSIONAL STANDARDS REVIEW ORGANIZATIONS (PSRO). These physician organizations effectively regulated many issues which are now the subject of the complaint. They were lobbied into ineffectiveness in 1980, and together with "Maricopa", essentially turned medical oversight over to insurance companies who thus receive no physician advice except from their own employees.
 Treat liabilities like debts. And transfers from the general fund as liabilities. 
|
| Accounting, for Congressmen |
1j. ENCOURAGE THE ESTABLISHMENT OF REGIONAL BACKUPS FOR AMBULANCES DRAWN OUT OF AREA. At present, ambulances are limited to going to the nearest hospital, rather than to the hospital of patient preference. The main justification for such behavior is the possibility that a second call might come while the ambulance was in a distant area. Fire departments have long solved this problem by shifting reserve vehicles into an overstrained area, to cover that area while the home vehicle is temporarily unavailable. In some areas, a reserve vehicle backup might require additional ambulances, but mostly it requires a mobile phone network. In areas of extreme distances between ambulances, the main need would be to relax regulations which exclude volunteer vehicles from serving that function. In densely settled urban areas, we now have the preposterous situation of mothers in active labor being stranded at the wrong hospital, only a few blocks away from the obstetrician who has their records. When such situations are repeatedly encountered, the current IRS exemption from financial reporting should be rescinded from the ambulance sponsor.
1k. As a general principle, when a service, device or drug is used in both the inpatient area and the outpatient one has its price exposed to regular market forces in the outpatient arena, the same price should be applied to it in the inpatient arena. It would be sensible to add a (separately negotiated) inpatient overhead adjuster reimbursement which generally applies to inpatients, and a second adjuster for the emergency room. There will be some services which are totally unique to inpatients or emergency rooms, which will have to be treated as outliers. In this way, a mutually reinforcing restraint is placed on such dual-use items -- with the market holding down outpatient costs, and the DRG ultimately holding down inpatient/emergency costs including outliers. As a general rule, the overhead cost-multiple established for dual-use should apply to the single-use items of either in-patient or out-patient. The key to all of these balancing limits is to permit open competition between hospital emergency services and private competitors, and an absolute prohibition of linkages between providers and emergency vehicle operators. After a brief trial, all such price constraints should be exposed to re-negotiation with an eye toward establishing transparent regional norms.
 The Supreme Court Needs Help, Too 
|
2. LEGISLATE OVER-RIDE OF 1982 MARICOPA CASE. This unfortunate U.S.Supreme Court 4-3 decision was never tried and upholds only a motion of summary judgment about a per se violation. It prohibits physician groups from agreeing on lower prices and has been taken to mean physicians are excluded from exercising control of HMOs and Managed Care. It also perpetuates the notion of individual competitors in a profession which is rapidly acquiring larger groupings as units of competition. By some quirk, the full tape recording of the 1982 U.S. Supreme Court arguments can be heard on the Internet. It is "above this author's pay grade" to know whether it would be better to ask the Supreme Court to review its earlier decision, or to make legislative changes in the antitrust law which would somehow result in a better outcome.
Looming Early Issues in Obamacare

|
| Obama Care |
The Attitude of Big Business. In order to preserve maximum flexibility as long as possible, many important features of the Affordable Care Act (Obamacare) remain unrevealed, and some are perhaps still unsettled. Furthermore, attitudes change with experience. At the formation of the Obamacare idea, the leaders of big business (at the time) were more concerned about foreign competitors than about employee attitudes. The traditional goal of a "level playing field" led them to favor an employer mandate to provide employee healthcare. It probably was presented to them that they could only have their desires by agreeing to a universal individual mandate for everybody. Although it was uncertain whether the employees would agree, universal was the price to be paid, and they paid it. Whether new leadership supports this compromise or not, it is generally assumed that big business feels obliged to support Pete Stark's universal mandate until it is tested. Only time will tell whether businesses will withdraw their support in the face of events, but fragile beginnings certainly do not assure permanent support. Since it was the withdrawal of this group's support which destroyed the Clinton plan in 1994, a significant issue hangs in the balance. Therefore, when conflicts were discovered with the ERISA laws under which big business works, the inclusion of big businesses in the framework of the Affordable Care Act was postponed for a year. How it will emerge next year or whether the ACA can survive for a year without major business inclusion, both remain to be seen.
The Rising Voice of the Uninsured. A financial recession usually increases the number of health uninsured, but at present unemployment is slowly falling. However, decades of scientific medical advances are not only extending longevity but reducing non-fatal illness among the young and uninsured. Although it is unclear whether youthful perceptions match the actual changes in their morbidity, young healthy people who rebel at paying health insurance premiums may actually increase in number substantially during the coming decade. Although overall inflation has been moderate, discomfort from competing costs of college debts and items such as gasoline have escalated. When the Affordable Care Act is fully implemented, youthful perception may make the first serious test of its usefulness. Those among them who actually get sick may get an opportunity to sample Medicaid and report their experiences to their friends. To some extent, this will be a race between efforts to improve Medicaid in order to forestall complaints, and the tendency of young people to try to get their way by pounding the table with their shoe. If successfully managed, it could promote some badly needed improvements in Medicaid. Handled poorly, however, it could bring the program down.
Cost of the Program. The fact must be squarely faced that insurance almost always increases costs. That is true of all casualty insurance, whether auto, homeowners, or maritime. Correctly applied, it can indeed redistribute costs, but insurance imposes extra administrative expenses, and it produces "moral hazard", so total costs are increased by insurance. Moral hazard is a term of art, signifying that nobody spends someone else's money as carefully as his own. Actuaries calculate the extra cost imposed by present American forms of health insurance to be at least 30% of the total service, and arguments can be made it will be so much more, that level historical costs cannot conceal the appreciably higher premium level. Longevity is improved by reducing the number of brushes with life-threatening illnesses in a lifetime; costs go up because prices go up.
Universal coverage now introduces its own uniquely unwelcome issue, that eliminating non-insurance market benchmarks for medical prices also eliminates the cost guidance they formerly provided. Crippled though it may have been, the partial cash market did set benchmarks, if not prices, which insurers then had to match -- and those benchmarks will possibly soon be seriously diminished. That development will be welcome to those who wish to receive higher prices, but cause dismay among those who have to pay for them. The result is predicted to lead to price controls, which will, in turn, provoke shortages, possibly demonstrations or worse. Matters may not follow that path, but it is hard to see why not. As to any reduced overhead like marketing costs, employer-basing has already reduced them to a small opportunity for streamlining. In the past, a resort to price controls has almost invariably led to shortages. Even in 2013, there have been shortages of cancer drugs, an almost unheard-of event in the past century.
To put it mildly, rationed healthcare is politically disadvantageous for those who attempt to enforce it. The most conservative projections now suggest that Obamacare will increase healthcare costs by 22%. Since the following proposals would by contrast almost surely reduce costs by a conservative 30%, it is not impertinent to suggest that no matter remains closed while a 50% overall cost swing remains credible. That would be particularly true when it concerns 17% of gross domestic product (GDP) during a recession. In fact, no one has even contemplated what it would mean to inject 5% of American GDP back into the world economy, especially by the mechanism of releasing a paralyzed medical system.
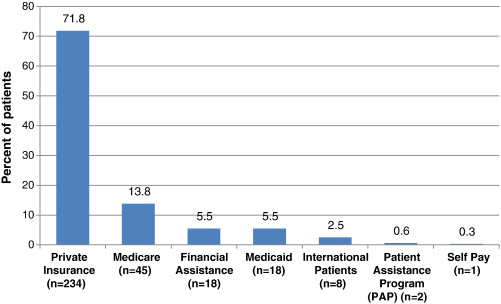
|
| Patient Participation |
Patient Participation in Claims Costs, Generally Speaking. For the insurance industry, this is an old story. Industry survival has depended on success in answering it effectively. In health insurance, the traditional approaches have mainly been 20% co-pay and about $500 annual deductible. The first means 20% of all benefits cost, the second means the first $500 of benefit costs in a year. These figures evolved out of countless negotiations between labor and management, or within legislatures, are now accepted as traditional, and are accepted by the public. These figures also represent how much each side thinks it can afford since they see themselves as ultimately paying the bill. Until recently, however, patient participation at such small levels has not reached a point where it significantly influences patient behavior, which is set by entirely different forces and is now the main long-term cause of healthcare cost inflation. As mentioned above, business negotiators seldom pay much heed to imposed costs, just so long as their major competitors must pay the same costs; in fact, that is one of the flaws in our corporate system. However, governments as third-party payers enjoy no such luxury, and most of the complaining about healthcare cost inflation has originated with governments. Consequently, businesses not infrequently drag governments to higher cost levels, and this must be recognized as a reality of entitlement programs. Furthermore, attempts at raising patient cash contributions have always had political rather than economic origins, usually loudly characterizing any cost constraints at all as crippling the intent of insurance, making false promises, and depriving the poor of humane treatment. If patient contribution ever reaches 50% of costs, the program will likely be called a failure (Insurance exchanges please take note.).
However, it would appear incentives cannot affect overall patient behavior very much until patient payments to reach a much higher point, and we may well see some experiments to test what that level may be. (As it is argued here, this dilemma need not be completely dispositive.) More recently, steadily rising healthcare costs have actually led to employer increases in co-pays and deductibles, and the Obama administration has been giving signs of yielding to the behavior modification argument. However, these approaches cannot be called a success until they seriously reduce long-term healthcare cost inflation, and that remains a doubtful outcome.
In fact, no desperately sick patient should ever be expected to pay much attention to costs. The restraint of partial cash payment should be reserved for lesser conditions, and even provider discipline should be reserved for what are provably individual provider decisions, whether at the institutional level or the professional one. There are certainly broad areas where no patient cost restraint whatever can be justified, and program design should recognize that premise. Nevertheless, much more could be done with patient participation in costs than is done at present.
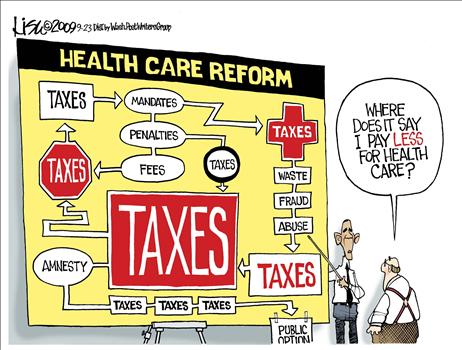
|
| Cost Restraint |
Targets for Cost Restraint Requiring Two Distinctive Approaches. There are two factors in overall medical costs: the item price, and item volume. Above a certain level of sickness severity, only item prices can be legitimately constrained, not the volume of service. Before any of that happens, of course, all published prices should be audited and forced to conform to standard cost-to-price ratios, because cost-shifted indirect costs are so prevalent. For minor conditions and illnesses, volume control on the patient remains legitimate, particularly for conditions where patients are usually responsible for inciting them. Patient cost-sharing is, therefore, a legitimate out-patient approach. Officials given the right to set such boundaries will almost surely be assailed as having a conflict of interest, or untrained for the decisions; it is an unpleasant role, attractive only to unpleasant people.
The healthcare market segments itself into two quite different approaches and successful administration consists of accurately distinguishing the two. As soon as the patient enters a hospital, his control of cost creation is taken away along with his clothes. Therefore, payment by diagnosis is a sensible approach for inpatients and could be even more effective if the diagnosis codes were revised to include greater stratification by the additional use of laboratory and other billing sources as confirmatory evidence. An argument can be made that fee for service to a helpless patient operates without cost resistance. But having removed incentives for abuse, the laboratory data becomes even stronger evidence of underlying diagnostic distinctions. Since Obamacare has apparently not fully examined such distinctions, there remains hope it can be persuaded to see the codes need expansion. At present, DRG codes are very crude and rely heavily on errors on the high side canceling out errors on the low side. Furthermore, they are derived from (ICD), the International Classification of Disease, which identifies individual diseases only if they are common, responding to the needs of medical records librarians who complained that usage did not justify the effort of coding every case. This combination of short cuts and errors is too crude for the advanced use now planned for them and would benefit from substituting the coding system called SNOMED3. A case can be made for both lumping and splitting; perhaps two codes are required, a crude one derived by computer-lumping precise ones of the same average cost -- rather than by similar etiology. As matters now stand, teaching hospitals have no way to assert a need for greater reimbursement for greater case complexity, specialty hospitals are able to select inexpensive cases within expensive categories, and rural hospitals are left without satellite cash cows.
However, this is tinkering around the edges of volume measurement. Much greater savings are immediately possible from attention to prices, through billing for direct and indirect costs separately, recognizing indirect costs as the present main locus of cost-shifting. Some serious thought should be given to the growing shift of profitability to the outpatient area, with inpatient care transformed into a loss-leader. As that is increasingly true, it becomes wiser to shift attention to the prices of outpatient and emergency room services. Going all the way to Health Savings Accounts would be ideal because it enlists patient incentives to the side of prices restraint. HSA also comes inherently segmented, between outpatient and inpatient hospital. Beyond segmenting price and utilization controls, however, consideration should also be given to segmenting health insurance itself, to match natural cost segmentations. Prison inmates, persons mentally impaired, and illegal immigrants account for nearly 30 million persons, and require specific ministrations, not patchwork exceptions to what the rest of the population requires.
Elective Hospital Admissions: Flexible Deductibles
Flexible Deductibles. Front-end deductibles are a long-standing tradition in casualty insurance, mainly popularized to accommodate automobile accident insurance. There features of health insurance, however, which are quite different from fender-benders should be suitable for appendicitis, however. Some things can only happen to a patient once, like appendectomy, or many other "-ectomies" which remove a whole organ. Some things are restricted to women, other things like prostatectomy are overwhelmingly found in old men. Because of a wish to give everybody the same benefits, particularly in industrial groups but also in other situations, these factors are ignored in setting a premium. Some subscribers are therefore deliberately and permanently overcharged. The insurance premiums could remain level (a process called "community rating") however, but some feelings of persecution could be reduced by adjusting the deductible downward for the first instance of an appendectomy, cholecystectomy or whatever. It could be seen as a reward for never coming back for that sort of thing, and therefore reducing the future costs of the program, as other diseases like pneumonia or broken legs do not. In fact, certain inherited features or a history of heavy smoking can predict increased risk for pneumonia, while "accident proneness" is well recognized in industrial circles. The spreading use of computers could make it relatively easy to see how much difference these indicators at different deductible levels actually make for future costs. If a changed deductible alters behavior, that would be fine; if not, at least the risk of a particular client group can be more accurately predicted. The result would eventually be a greater willingness to transfer insurance carriers. At the moment, there is a hidden reluctance among some patients, not unlike the other causes of "Job lock", in which beneficiaries must weigh the consequences of switching. It could also affect the pricing of secondary insurance.
|
| IDC-10 Codes |
Earlier it was stated, deductibles should apply to outpatient services, but are essentially useless to restrain inpatient costs, over which the patient has no control. That is true but misleading. If appendectomies represent 5% of all health care costs, someone's health insurance should be 5% cheaper if he has already had his appendix removed. If a hernia repair is considerably more comfortable in the hospital, someone who prefers to be in the hospital ought to pay more than someone who has it performed as an outpatient. From time to time, we read of a rich old lady who lives for several years in a hospital because she likes it there. If she is willing to pay for it, why not? She just should not be permitted to use insurance to pay for it. If the same procedure is sometimes performed for an outpatient, but occasionally requires hospitalization, that distinction can seldom be made by the diagnosis alone. Most probably, the submission of certain items of laboratory work will justify it. This point is both more subtle and more complicated than it sounds. Traditionally, insurance rules concerning elective admissions are based on diagnosis codes so insurance utilization clerks can approve them; much friction results when such decisions prove inappropriate. The diagnosis code for "status post-appendectomy" is seldom used at present, but it would make a simple vehicle for appropriate pricing incentives. The process of challenging peculiar-looking diagnoses then becomes a major cost in time and money for everyone concerned, even though deductibles purport to generate cost savings. Finally, a flood of elective admissions may itself suggest a need for all deductible amounts to be increased. It is, of course, possible to go too far with such a process, which needs to be perfected on a diagnosis level before it is extended any further. Best of all, the size and applicability of deductibles might be left to the various competing insurance firms as a competitive tool; some would do it, some wouldn't, and the customers could choose.
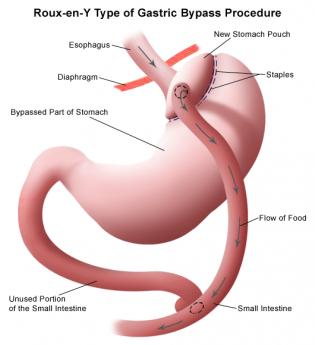
|
| gastric surgery |
Perhaps a further useful example lies in the evolving use of gastric surgery to treat obesity. The procedure is presently characterized as more effective than any other available approach to morbid obesity of the six-hundred-pound variety. And yet patients with advanced degrees of disability from obesity often confront the surgeon with considerable extra difficulty and risk. Under those circumstances, it can be both hazardous and expensive. At the opposite end of the spectrum are neurotic patients with only minor degrees of obesity, sometimes trivial degrees, who demand what amounts to cosmetic major surgery masquerading as a treatment for gastric reflux. A fairly high deductible, particularly one buffered by a Health Savings Account, could usefully have two or three deductible plateaus matching specified features of advancement. The proposal is roughly this: the more obese the patient, the lower the deductible. The surgical treatment of obesity is a particularly illustrative example at present because recent evidence is starting to identify the avoidance or reduced cost of diabetes when it is already present. Some insurance companies may wish to take a chance on this promising development, so making a large deductible and discounting it as evidence accumulates would provide a mechanism for accomplishing that goal. The managers of other groups may offer traditional reasons for retaining community rating practices; both options can be retained by adjusting prices at the level of the deductible.
But to repeat the central point, deductibles need to be larger than they have traditionally been, to be able to leave room for the incentive of discounting them.
The Pharmacy Example.

|
| Pharmacy |
The Pharmacy Example. It would seem, a natural place to introduce computing to medical care delivery would be the drug store. Almost everyone is familiar with the process of the doctor writing out a prescription and giving it it the patient. And it's likewise familiar how a patient takes the prescription to the store, gets the bottle of pills, and pays for it. The drugstore seems to be a single link in the chain between doctor and patient, with only the prescription adding input, only the bottle of pills generated as output. So let's begin there, watching an example of how simple things rapidly become complicated. The pills are standard, the inventory is already digitized, insurance can be made to enforce a standard number of pills in a refill, the pharmacist can then be replaced by a high school girl. You give the patient 30 pills, and 30 days later he needs another 30, right? Well, not exactly.
The computers are in the drugstore all right; usually five or six of them. What's missing is the professional latitude of the former owner-pharmacist, replaced by an automated assembly line. Druggists, as we knew them, began to disappear around 1970, and computers probably had a lot to do with that first step of moving from corner drugstore toward pharmaceutical ATMs. Prior to World War II, most pharmacists could even compound capsules from powders, and mix various-colored liquids in a bottle. That is to emphasize, the corner drugstore and its friendly owner-operator were well on the way to disappearance, quite a while before outpatient prescribing was overwhelmed by health insurance. It must not be imagined that disentangling insurance from outpatient prescribing would automatically take us back to a system which allows more professional latitude between ancient professions. That might well be desirable, but opportunity is fading fast.
The drug stores by 1970 had already automated most of their process to a point where insurance designers could easily imagine substituting insurance billing for patient billing; and linking that combined payment system to a pill fulfillment system. If only a way could be found to substitute bottles of pills for twenty-dollar bills, the drugstore would already be on its way to becoming a cash-dispenser, or at the very least, a candy-dispensing machine. Technology had only been waiting for someone to pass a law.
Shortages. Very probably the concepts of centralized control began with the Pharmacopeia. Originally, this term referred to a list of drugs the store kept in stock; an inventory list. When supplies got low, they were re-ordered in an amount judged sufficient until the next delivery. Certain drugs and certain supply houses were preferred, so once a decision has been made, the stores and the suppliers kept themselves ready for business. Hospitals maintained a more elaborate Pharmacopeia, usually with a committee appointed to oversee the list. Until the Second World War, most of the patients were in the indigent wards, so custom evolved into the idea that private patients could have anything the doctor ordered, often ordered from the pharmacy across the street. The Pharmacopeia was for indigent patients, taking the view that the committee was to decide matters of quality, and the hospital pharmacist had the latitude to order the cheapest generic version available. This didn't always suit the doctors with private patients, so there was a tendency to extend it to all drugs, quickly jerked back into line by the private physician giving a prescription to the patient's family, to be filled in the drug store across the street from the hospital. When insurance came along, this sort of thing lost its point, so peace was restored by converting everybody's drugs to the more expensive variety, essentially disbanding the committee. It was an important turning point: the conflict between quality and cost was almost instantly resolved by letting insurance just pay for the best. When the pharmaceutical companies saw what was happening, inclusion on the favored list began to revert to the quiet preferences arranged between the companies and the hospitals. In time, drug prices began to go up, insurance companies noticed, and the committees had to be restored in order to assure that quality was preserved. Around 2012, shortages of vital drugs began to appear; up to that point, shortages were unheard-of. But Philadelphia was somewhat quicker to recognize what was happening because it had all happened in Philadelphia in 1778. Price inflation invariably provokes rationing, and rationing provokes shortages. And shortages soon lead to rioting, when it is discovered that shortages have appeared, in spite of hoarded abundance. American pharmaceutical firms found that generic drugs were unprofitable compared with drugs under patent, so they stopped making generics. Third-world countries continued to make generics, but only when it was profitable and free of probing inspectors. Shortages are a likely sign of government intrusion; shortages in the midst of abundance are a certain sign of it.
Regimentation. Once hospital nursing systems got around to individually recording drug use, it was only a matter of time before someone got the idea of devising a set of "best practices", matching them with what had actually been prescribed, and identifying which doctors complied best with the best practices. That's where reality sets in.
The designers of pharmacy systems have assumed that directing the computer to record what ought to be done, is the same as describing what has actually been done. Unfortunately, in an outpatient environment, the patient is generally acting as his own nurse and is almost always somewhat sick. He is also paying at least a portion of his bill. When the cost of a cheap generic is a penny a pill, slack can be created in the system by throwing in a few extra pills. However, when an expensive brand name drug, say one costing ten dollars a tablet, is authorized by the insurance, great care is taken to dispense precisely 30 tablets every 30 days, regardless of Christmas or Sunday, Hell or high water. When a pill accidentally goes down the drain, or gets forgotten, or wasn't in the bottle to begin with, the situation is exaggerated that the patient is short of the expensive pill, but has a surplus of cheap ones. He tends to wait until they match up, but the computer clock is running and usually won't allow the slack to catch up with itself. At this point, often a relative -- let's say the daughter flew in from California -- discovers that the patient hasn't been taking pills which are fearfully expensive, and therefore vital to survival. It is very likely a fact that the expensive pill being skipped is indeed the one most likely to be critical to his condition. The dilemma almost always reaches crisis proportions at a time when there is no one available to over-ride the computer. The rest of this little scene is best left to the imagination.
Taxes as a Form of Consumption
About half of the American public pays federal income taxes, and among the half who don't, a great many receive a green government payment check, meaning they have negative income taxes. The tax assistance companies, H. and R. Block and the like, had little for their offices and staff to do in January, February and March until someone hit on the idea of processing "fundable tax credits" for a fee. That is, the lower-income segments of the population get the promise of an April tax "rebate" as the consequence of tax-form preparation, so H. and R. Block just loans them the money, discounted for fees and interest. It keeps staff busy, generates revenue. Hardly anyone in the upper income half of the population is aware of all this, so there is little political friction. This whole system of income redistribution quite effectively keeps the two halves of the population sitting in the same chairs at the tax-preparation offices, but in different months of the year; one half getting paid, the other half coughing up the payments.
It thus becomes possible for two inflammatory slogans to bandy about, without starting fistfights or revolutions. The first was overheard at a local bank, one stranger remarking to another, "Has it ever occurred to you that taxes are a form of consumption?" To which the other person replies, "Yes, and taxes are the largest expenditure I make." A nation which once went to war over a two-cent tax on tea is remarkably passive about the ways things have evolved, but this essay is not devoted to unfairness. Prepare to hear how the upper income brackets might reduce their taxes, whether that counts as decreased consumption or not. Whenever you tax something, you get less of it; if you tax public income more, the public will earn less. So, this little essay is serious when it proposes that we all earn less, so we can get taxed less. And being taxed less, we need save less for our retirements.
The general principle is this: income is usually taxed in the year it is earned, with some exceptions, rebates and deferrals. The exceptional situations are often referred to as "loopholes" and therefore live in political jeopardy. However, if a person spends the money or dies while these deferrals continue to exist, the income may escape taxation entirely. In a sense, the largest loophole of all lies in the present fact that nearly half the population pays no income taxes at all, so saving income earned under those circumstances may lead to investment capital, which is later spent during highly taxed periods of that same person's life. Money earned by a child, usually on investments donated by a relative, is an example. Since at present, a child may receive annual gifts of $13,000 tax-free, as much as a half-million dollars can be accumulated in this way, always at the risk that laws may be changed and, further, at risk of spendthrift abuse by a psychopathic child. Whether these are wise risks for a parent to take, depends in large part on what sacrifices are made for the purpose, especially loss of parental restraint of unwise spending. A much more serious argument grows out of the possibility that money in the hands of children who lack experience in deferred gratification may actually provoke recreational drug use, or other sociopathic behavior.
Finally, lack of planning may create opportunities as much as planning does. A person who has paid little attention to financial planning may arrive at an advanced stage where life expectancy is considerably shorter. Savings at that point may be divided into money on which deferred taxes must be paid when you spend it, and money on which taxes have already been paid. More savings will be consumed if the individual triggers deferred tax liabilities, than if he just uses up money on which taxes have already been paid. Therefore, if he ignores lifetime habits and spends after-tax capital first -- the whole nest egg will last longer. But none of this deferred-income tax issue can compare with the problem of income on which taxation has been completely forgiven at the time it was spent, the so-called tax expenditures. The largest such tax expenditures are on the interest of home mortgages, on employer-paid (but not self-paid) health insurance, and employer-paid retirement income. Of these, the least consequential are the retirement income, because the tax is merely deferred, not completely forgiven. The two biggest items are home mortgages, which lie at the root of the 2007 financial crash, and employer-paid health insurance premiums, which triggered the Obama health proposal of 2009. The Obama plan purports to rein in health costs, but is estimated by the Congressional Budget Office to cost the Treasury $100 billion a year.
Extra! In the Fall of 2011, this boring matter suddenly came to the surface, in the form of huge American deficits threatening to bankrupt the country, as they were apparently actually going to do in Greece. As politicians do, many attempts were first made to rename the over-spending issue for partisan advantage. It was, for instance, tax expenditure. It was, possibly, a sovereign debt crisis. In any event, the Congressional Budget Office included such wealth redistribution under the heading of tax expenditure, which totalled a trillion dollars. Since everyone was searching for a painless category to eliminate in order to balance the budget, this term was hard to avoid. As far as Congress is concerned, the national deficit is whatever the CBO says it is, and in this case it lumped a lot of things together which politicians would like to split apart. When you take things in small pieces, it becomes possible to boil the frog by slowly heating it up before it realizes it is cooked. Lumping things together induces the frog to jump out of the pot, but however that may be, it has got lumped together by the referee of such matters, and there is a strong possibility it will stay lumped.The essential point for accountants to focus on, is that tax expenditures are all counted as revenue when any non-accountant can see they are expenses. For political speech-making purposes, this distinction is vital and no opponent will let another politician wiggle out of it. And the beauty part of it is that it also spotlights three of the most besetting evils of modern politics: the tax exclusion of employer-based health insurance, the home mortgage interest tax exclusion, and the "earned" income tax credit. The first of these is responsible for our health insurance mess, and the other is responsible for our home mortgage crisis; the two main political problems of the day are suddenly plopped into the limelight, just when a lot of people are looking for ways to hide them. Furthermore, this bombshell was fired by a panel of the four outstanding tax economists of the nation, each of them roundly denouncing them as unthinkable ideas that never should have been born in the first place. Alan Greenspan, famous for unintelligible speech, simply said all of these tax expenditures, every one of them, should be eliminated immediately. One would hope that is clear enough. Martin Goldstein, formerly chairman of President Reagan's Council of Economic Advisors, agreed. As did former Governor Engler of Michigan, widely acknowledged to have rescued his state from impending bankruptcy. Senator Nelson, a Democrat from Florida and chairman of the committee, positively beamed with pleasure. It was hard to think this was anything but a turning point in history; let some political candidate disagree, and he can expect to have his audience shown a videotape of this succinct epic in the history of Senatorial hearings. These greybeards said, in what was obviously an unrehearsed moment, just eliminate these three terrible ideas in one stroke, and the national deficit will be reduced by a trillion. That's what they said, and it's easily proved that they had said it.
Rationing, No Matter What You Call It.

|
| Arthur L. Caplan |
The Right Angle Club of Philadelphia was recently addressed by Arthur L. Caplan, Director of the Center for Bioethics of the University of Pennsylvania. His topic was Healthcare Rationing. It was interesting to hear the viewpoint of someone who views the 2010 mandatory health insurance system primarily through the lens of its ethics; just like the Tea Party objectors on the other extreme of politics, he sees the new law as merely a rationing system. However, his initial salvo is similar to that of the bill's proponents before it was enacted: "Every system always rations in some way or another." If you expected the outcome to be rationing from the beginning, your focus is naturally fixed on just what sort of rationing you get, perhaps measured by whatever kind of rationing you had formerly hoped for.
Ethics is, after all, a system of constraining native, unconstrained, outcomes into something deemed more suitable. That's a definition which could be equally well applied to the reform of all sorts and repeatedly tends to cast reformers as underdogs fighting the establishment. Since the American healthcare system in 1950 could fairly be described as rationing healthcare with money, and its history from then to now has been one of jumbled similarity to 1950, most discussion accepts a financial rationing description for what Obamacare changed. There is much uneasiness about totally supplanting the marketplace with insurance since universal insurance leaves no room for setting prices -- except by government proclamation, filtered through some sort of insurance bureaucracy. There was a time when many people thought that was better than paying for it yourself, but now that it's here, there are growing doubts.

|
| UPENN |
There's surely going to be a last-ditch effort to overturn Obamacare, whether through Congress or the Courts and failing that, through stalling it until the President can be replaced in 2016. Let's assume for the moment that such efforts fail, and are not followed by armed rebellion. If the central issue is how do we find more acceptable methods of rationing, two proposed methods have begun to seem attractive. The first is proposed by Congressman Ryan of Wisconsin, to the general effect of taking what we now spend, chopping it up, and issuing vouchers for the same amount less net middle-man costs. This approach stops the rise of costs right where they are, and thus pleases Congress. But the thing to be rationed is redefined as well. It rations future cost rises, net of any savings wrung out of the system by competition for voucher money. It's fair to claim this system should not deny the present level of care to almost anyone. It has a price, however. If you want future miracles, you have to pay for them.
A second proposal depends on the observation that most healthcare costs are concentrated in the first year of life, and the last year of life. Strip those costs out, and what is left would almost surely be manageable, particularly in view of how the concentration of costs in those two areas steadily increases. Essentially, this system promises to take generous care of the helpless when they are born and when they die. Healthcare costs during the years of school and employment, however, could more confidently be left to people who are sentient and reasonably healthy, so that's where the inevitable rationing would be concentrated. Once more, the payment system has been modified to avoid such third-rail issues as euthanasia for Grandma or for self-inflicted diseases, or even for abortion. Those would be left to the public to manage during stages of life where there is a reasonable likelihood that the patient's own wishes can be paramount. For now, we pass over the technicalities of last-year-of-life insurance, but it could fairly begin with reliance on reimbursing Medicare after the fact, while traditional first-dollar insurance for pregnancy and newborns, or even mandatory government reimbursement, might seem acceptable even to strong conservatives.
So, what's proposed here is a substitute for both the traditional system and the bewildering command and control system of Obamacare. It shifts the subject matter for rationing away from those areas that frighten the public the most, toward either: rationing future unknown scientific advances, or, rationing healthcare during the years when it is comparatively predictable and involves patient cooperation during the years of reason. That's the summary; other proposals are welcome.
Regrettably, after each November election, we first must potentially endure a lame-duck Congress, followed by two years of White House-Congress gridlock. There will, unfortunately, be scant tolerance for ethicists, during those grievous national experiences.
Merging Insurance Companies with Health Delivery Systems

|
| Geisinger Clinic |
Not long ago, a presentation about payment reform was conducted by the CEO of the Geisinger Clinic, which has been praised as a model for many features of Obamacare. It seemed clear that many of the ideas coming from Geisinger emerged from the circumstance that Geisinger owns and operates a health insurance company, and could, therefore, see both sides of many questions. Listening to this talk was highly reminiscent of the fruitful results which once grew out of the Pennsylvania Medical Society owning and operating a Malpractice Insurance Company. Although that relationship has been dissolved, it exposed practising physicians to many unexpected revelations which continue to be useful. No doubt Geisinger profits from similar insights into the health insurance world, which is in a sense a competitor with physicians for medical domination. Geisinger is definitely a physician-dominated system, so it could gain insights for its physician leaders, similar to what hospitals once learned by starting Blue Cross plans. Following this particular lecture by the doctor from Geisinger, a panel of six eminent commentators was seated on the stage, not one of whom had spent a single day in the practice of medicine. In some circles, this phenomenon is called the "silo effect". Those who are preparing to dominate 17% of the Gross National Product, really should have been expected to have spent more time in the existing system than appeared to be the case. If exceptions to the antitrust laws are required to permit bridging of these coveted information secrets, they should be re-visited immediately.
It is not too late to change, even though it may be too late to rescue Obamacare from a bumpy beginning, if not an implementation train wreck. We have heard testimonials from organizations which have navigated one or two implementation hazards. We will soon see whether the rest of the health industry can safely navigate all of them at once. Teams of practicing physicians, experienced hospital administrators and thoughtful insurance executives should be assembled to design pilot programs for best practices in fixing engines while the motors are running. Clever work-arounds are most likely to grow out of small teams which share effort among veteran warriors in former conspiracies for power. The silos, if you please.
Addressing the Computerized Medical Record Muddle
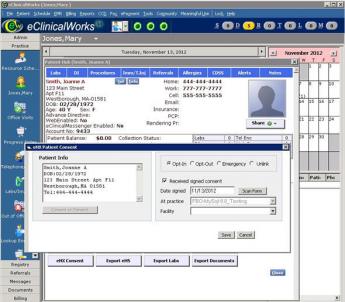
|
| Computerized Medical Record |
Who Should Rule? At first, even physicians were enthusiastic about computers in medicine. The computerized medical record was to have been the smash hit of Obamacare. It promised dozens of efficiencies, vast reductions in cost, and a glittering example of how young minds always see the future clearly while old traditionalists fail to recognize the obvious. However, after the expenditure of millions of dollars of development money, the reaction of doctors to the electronic record now is, "It's a good idea, but it's too much work." What seems to have soured the medical profession most was to discover that the computer designers had cast the model in imitation of the hospital medical record system, largely mirroring the viewpoint of the librarians. Record librarians spend a lot of their time telephoning doctors to come to complete their charts, and have little patience with excuses; they write the stuff, we file it.
Computer designers then brightened up, explaining the wonders of "real time". Compose as you work, let the machine reassemble it, go home at five o'clock. Doctors often wrote a separate composition called Physician Notes, nurses wrote on a different colored paper called Nurses Notes. Nurses notes were usually discarded at discharge until the hospital lawyers forced a stop to suppress evidence. No problem, the computer can easily integrate the two. Unfortunately, the nursing verbiage so heavily outweighed the physician scribble that the dominant emerging discussion consisted of -- what was formerly discarded. The narrative was composed by a couple of dozen people, very few of whom read anything written there except the last entry of his own. It was much like the academic scholar approach, in which a scholar with a new book, first looks in the bibliography to see if his name is there. Otherwise, no one reads bibliographies. When last heard from, this "Progress Notes" approach was headed toward extinction in favor of a "Discharge Summary" written by a single physician, although hospital lawyers still generally insist that the underlying notes be stored indefinitely, as a basis for constructing a legal case against the hospital if the outcome is poor.
All of this was quite bad enough when the system managers started to discover it was easier to get the facts by going straight to the doctor, who promptly labeled the system as "turning the doctor into an input clerk". The famous baseball player Jackie Robinson reached a different conclusion: "Never look back, 'cause something might be gaining on you."
When the computer began to supply a list of medical facts which the doctor had omitted from his recital, refusing to go forward until the missing data got supplied, the situation was getting threatening. One final thing: the medical librarians, naturally seeing the only purpose of filing this data was to retrieve it later, lobbied the reimbursement system that they needed a new code, the International Classification of Diseases (ICD) which reduced a million diagnoses in the Standard Nomenclature of Diseases (SNOMED3) down to no more than ten thousand, with the rest lumped together as "all other" or "not otherwise classified". Very few people understood what librarians were talking about, but when reduced to its essence, they argued that if a disorder wasn't common, it was easier to go the "boneyard" and go through the charts one by one. This transformation took place at the time these codes began to use for reimbursement purposes, resulting in repeated revisions of the code to match the money. It now seems pretty clear that a list of the commonest conditions must eventually revert to a meaningful coding tree if we are ever to escape from using endless high-speed iteration (the underlying process in digital computers) as a basis for finding charts on a shelf.
A brief analysis of user complaints is this: most efficiencies involved some shift of data entry from clerks to physicians, with resulting higher input costs. User-friendliness for patients soon dissolved with the public's awakening they too had expected to be helped, not regimented. Evidently, the designers of the software architecture did not adequately value the points of view of either patient or physician, which seldom match those of the third parties. The design of the computerized medical record evokes memories of the collision between the department store and the housewife in 1978 when only one of the two possessed the terrifying power of an expensive computer and got arrogant about it. In the end, the housewives won that war by fleeing to big box stores in the suburbs. The customer's determination not to deal with a monolithic billing administration under one roof resulted in a redesign of the department store. A subsite two blocks long sold nothing but children's shoes, but at least someone knew something about shoes.
The design of these products should begin, and eventually must finish, with the premise that medical care contains variable degrees of labor intensiveness, each degree following the other in quick succession. In addition, there is the Sherlock Holmes fallacy that a diagnosis is frequently based on a mathematical formula, when in fact most diagnoses are instantaneously recognized by an experienced physician based on what the patient tells him in the first five minutes of an interview. To modify slightly the words of Oliver Wendell Holmes, the life of medicine has not been logic, it has been experienced. The painstaking recording of the features which led to a diagnosis may well assist a beginning medical student studying the case, but they seem like a preposterous waste of time to a busy practitioner. Another clinical maxim for computer design to grapple with is that "More diagnoses are missed because the doctor didn't look, than because the doctor didn't know." Most of the time the doctor does look, and inking a check-block is merely an irritant. In those cases where he doesn't look, the cause is usually that he was either distracted or overworked, but in any case, he doesn't record what he doesn't see. But heaven helps us if he records everything he does see. It's easier to let a computer program recite everything which it is conceivable to see. Take for an example the recent discovery that sleep apnea is caused by the fatness of the tongue, now easily recognized without an MRI. Of what value are a zillion computerized records that the tongue was "normal to inspection"?
The designers should have begun with what is easily automated, like laboratory results, billing, and prescriptions; and only then constructed a useful system around them. A modest system which delights the medical personnel might then have enlarged its sphere when technology caught up to more difficult tasks like summarizing physicians' notes. With doctors of differing levels of personality and experience, little would have been expected until the system offered more in return. It may seem to others that patients will do anything a doctor tells them. But even in that traditional relationship, salesmanship is fine, rigidity is resented. There are many areas where relevant data entry is already automated, so a partial but greatly enhanced medical record is therefore immediately possible. Step by step, the totally digitized medical record could have advanced amidst general applause. This system should therefore re-begin by offering unchallengeable veto power to a large community of physicians, the early adopters, limited additionally to those who have earned the confidence of their colleagues by making a living as practitioners. They must repeatedly defend themselves to colleagues who are not early-adopters, never will be, in order to defend against the accusation they are hobbyists, or secretly nurse conflicts of interest.
That's on the data input side. On the output side, greater respect must be paid to the ability of electronic printers to produce overwhelming masses of reports. They are neat and uniform, but few doctors have time to read them. Doctors must continually devise concise summarizations, paying respect to the rapid obsolescence of relevant information as the case unfolds, rapidly discarding information which only recently was vital to know. At the same time, the system must tolerate a greater repetition of strikingly out-of-bounds reports. Reconciling summarization with redundancy is not an easy task. The ideas for flagging outliers and deleting noise must come from physicians in active practice, who will otherwise resort to adhesive tape, felt pens and alarm clocks. No doubt the requirements of accrediting agencies and the tort industry are in conflict with these notions. If necessary, separate records may be produced for their use and stored in standby locations. No attempt should be made to conceal their acknowledged irrelevance.
The Electronic Medical Record is a fine idea, so long as it limits data entry to material which is already digital, requiring no extra effort to get it into the system. As soon as medical professionals are commanded to touch a keyboard, costs will soar. We have plenty of useful things to do with digital medical data to keep us occupied until medical professional data entry does become feasible, as it must. It might be five years, or it might be ten. But to hurry it up is to cost billions of more dollars, producing very little to show for it. Therefore, the following billion-dollar solution is offered for this multi-billion dollar muddle. It's a Hail, Mary football pass, as would be said in college football.
The Big Data Approach. "Big data" is an unfamiliar term for most readers, but it describes the use of many computers to solve a problem whose data is too large for a single computer to handle. The design reduced itself to a single computer program called Hadoop, itself based on a disarmingly simple idea of splitting a vast amount of data into as many pieces as there are available computers. Soon referred to by non-reverent Google engineers as "Map, shake and merge", the program is free, Amazon will rent 50,000 computers to run a program, taking ten hours to run and costing about $12. Once the approach became feasible, many problems were found which could usefully employ fifty thousand computers at once. Just as happened in a number of computer revolutions of the past fifty years, people in charge of big data projects went wild with enthusiasm. A national Presidential campaign was apparently won by Hadoop. There were spy stories of drones picking out bandits five thousand miles away, and blowing them to pieces (Hollywood, please get busy). One man in Connecticut earned $6 Billion in one year, legally and for himself, and by the report, he was able to make it shake, rattle, and re-emerge. Anyone in charge of huge amounts of data is in a position to produce something pretty astounding with it. However, this sort of thing often ends in tears, and all hard reality lies under a mantle of jovial simplicity.
Beyond a certain point, most of the limiting factors preventing still further use of hundreds of thousands of computers reside in coordinating the symphony. If a computer has one electrical failure every thousand hours of use, fifty thousand will have fifty failures per hour, and just fixing the flaws becomes a new problem to address. Even without failures, the computers get out of synchronization pretty regularly. So although big data gets more powerful with increasing size, it develops new challenges. Nevertheless, it turns the science of statistics inside out, since it is often easier to count the whole thing than to take samples and estimate an aggregate result from them. So to speak, it becomes easier to take a preliminary vote of the whole electorate than to use Gallop Polls. Astronomy, chromosome research, weather prediction, opinions, styles, and tastes are only a small fraction of areas of interest which generate more data that can be readily managed with a single computer. Obviously, the stock market is another area which generates huge volumes of data, but simultaneously increases the incentives for secrecy, and pays its employees more than colleges can pay professors to popularize the techniques. The huge volume of data which can be expected to emerge from computerized medical records universally applied, will, therefore, present a huge opportunity, but one now held back by non-scientific incentives as well as serious privacy issues. We assume there is something of value to be learned by mining this data but we cannot be sure of it in advance. Nor can we be sure whether asking trivial questions, like determining the average square root of the nation's Social Security numbers, will make this enterprise the butt of every joke. Big data is the general approach of certain Wall Street hedge funds who have made astonishing amounts of money, much envied and imitated by other Wall Street firms who have only lost huge amounts of money. It is at the heart of the Google search engine, and rumor has it that Amazon is far advanced in the business of assembling and renting out gigantic computer farms to people who think they have a Big Idea and assemble cash to use a computer farm for ten minutes or so.
It seems perfectly certain the Big Data approach will be explored on this tempting mountain of medical data, which no one will be quite sure how to exploit. Much of the future of the approach will depend on its luck in discovering something strikingly useful during the early stages because the cost of it can be so quickly calculated.
What Purpose is Served? Whether big data techniques have any general utility for medical care is not certain. Big questions, like the distribution of diabetes among people who are overweight, can be answered by occasional investigations, or at most a few institutes committed to the task and reduced to a few sentences in a textbook. Only if utility in everyday use can be personally confirmed by almost every physician, will the original design of the Electronic Medical Record prove to be useful? No doubt, computers will shrink to the size of a walnut, and no doubt enormous surveillance systems can be designed for uses which plaintiff lawyers, consumer complaints, the patent infringement industry, and reimbursement oversight can best describe. No doubt it would detect the practice of medicine without a license, failure to maintain continuing education credits, and probably a dozen other investigations of suspicions. Bur all of these intrusions will be frustrated until someone devises a way to induce physicians to use computers in their everyday practice. For transmitting laboratory reports quickly, that day has already dawned; physicians would be very grateful to see a system created which would notify them of matters needing instant attention no matter where the doctor happens to be, including the toilet. Even the disruptive effect on the family life of being constantly on call can be tolerated if such an important service is created. But the dreams of the electronic record enthusiasts went far beyond that, in two principal ways.
The aspiration to be complete made the doctor into a clerk, cutting out the middleman who happened to be his secretary, nurse or assistant, and furthermore created an easy way to monitor whether he had fallen behind in supervision. And secondly, it created mountains of information which even in summary form, the doctor had no time to read . For doctors practicing in large group practices, addressing these two issues had been a growing necessity for quite a few years and was now seized upon by such organizations as a way to cope with their largest source of inefficiency. Doctors in private practice usually organized their own systems to avoid such issues, but now a solution for group practices is forcing solo practitioners out of business, because of a perceived need to be universal. At the other extreme, solo country doctors once had no need for such archives, and certainly had no time to cope with such demands on his time. Reducing someone else's profession to a vast array of yes-no answers soon taught the lesson that the task was not likely to be generally satisfactory for another decade, so some reformers were unwise enough to suggest the medical profession should be redesigned top to bottom to accommodate the issue. Making suggestions like that in Alaska, Wyoming, Texas, and other far-flung territories only lead to the election of physicians as congressmen in those districts, surely a worrisome thought for progressives. But in other areas, such resistance was seen as a sign that fee-for-service practice was a sign of wickedness. A more reasoned stance would be: Waiting a decade with such suggestions until the doctors in group practices can influence computer re-design, would leave time for the medical profession to adjust to many other urgent matters, first. (The next and final chapter address the direction we might consider if we really are prepared to redesign the whole system).
Physicians Must Dominate Medical Computing Design
Physicians Must Dominate Medical Computing Design. Not many people would dispute that doctors are generally smart, and for present purposes, most of them would not mind being called nerds. I started to use my first computer in 1958 when I was as good a beginner as any other beginner. For these purposes, boasting about math prowess really needs to apply to only 10% of doctors, which it probably already does. From the other 90% can be drawn the politically skillful who will be necessary to wrestle control of medical computing away from those who don't want them to have it.
The accountants who currently control hospital computing want to control the flow of medical information in order to keep the doctors from intruding into the thickets of cost-shifting and reimbursement maximization, but doctors need to be more closely involved in hospital cost accounting for exactly that reason. The main reason to keep others out of your computer is to be able to hide your mistakes. If you think that is so trivial and reprehensible that no one would stoop to it -- well, I pity you. Furthermore, it happens to be cheaper for hospitals to use doctors for data input than to design systems for reducing the clerical burdens of doctors. Cheaper in the short run, of course, because the hospital accountant cannot redesign systems of health delivery, but he can reduce his budget for data entry by shifting the cost to other departments. The accountant knows that if push comes to shove, the doctor can keep him from going home at 5 PM; his solution is to keep doctors out of his equipment. And in the dark.
Consequently, we are now spending billions of dollars on the Electronic Medical Record, and physician members of my family tell me it adds two hours to their workday without any increase in patient care. Obamacare is currently buying physician compliance by offering cash incentives to use useless systems. I speak with such passion because I attempted such a venture in 1966, and abandoned it in 1976 because of excessive data entry costs. It perversely pleases me to know of two large international corporations who have lost their shirts making the same discovery. The Electronic Medical Record is a fine idea, so long as it limits the data entry to material which is already digital. As soon as you command medical professionals to touch a keyboard, costs will soar. We have plenty of useful things to do with digital medical data, enough to keep us occupied until medical professional data entry becomes feasible, as it must. It might take five years, or it might be ten. But to hurry it up is to cost billions of more dollars, with very little to show for it.
Warning: Crowding Out
Warning: Crowd-Out. When Health insurance was still a novelty, sickness and health seemed like a lottery. With time, it became apparent that about half of healthcare costs were routine, particularly if you view the cost of being born and the cost of that dreadful last year of life as 100% certain for everybody. In this book, we gradually evolved a system which is about half insurance, half pre-payment. Bear with a little repetition: medical costs are crowded near the end of life, concentrated in people who are no longer working. That is an advantage when you imagine a method of saving in advance because a considerable cost reduction will result from investment and compound interest coming early, while heavier expenses come late. By instituting a "pay as you go" system at the beginning of a huge scientific reduction in disease, "pay as you go" managed to survive for fifty years. Meanwhile, the pre-paid system we have conjectured would have done much better, because increased longevity compounds investments for a longer period of time. Health pre-funding seems to be the better approach, no matter what happens to the science of medicine. That may not be true if non-medical forces dominate the next century of the environment of health care, but at least this point seems settled.
That's one way of looking at health costs, but it is also possible to see them as part of a huge transfer system between generations, which will endure under any set of circumstances. The really sick people are often unable to pay for themselves out of current earnings; that's the old retired generation. Working people in a younger generation are better able to pay, but they mostly aren't sick. Since there is essentially no one else left, working people must simply face up to paying for sick people, under any system it is possible to devise. To acknowledge those facts isn't a sign of being compassionate, it's a sign of common sense.
And there is one more fact of the matter: most people simply don't trust an implicit promise of repayment "when their turn comes", fifty or more years later. Governments develop more urgent priorities, like national defense, which for thousands of years repeatedly diverted loose cash to new projects. Regardless of motives or promises, experience teaches that governments are unreliable custodians of private wealth. Experience, therefore, suggests it might be best to exclude routine medical costs from a government-run system, thereby enhancing public protectiveness for what is left. If circumstances force routine costs to be included, the long-run strategy should endure: try to transfer such costs back to the private sector, and if possible back to individual responsibility whenever that does become feasible. Don't let government get off cheap when you must ask for its help.
The Medicare Annual Deficit. The present predicament of Medicare offers a particularly vivid example. Medicare is popular with everyone, so popular indeed that many wish to convert the whole medical system to "single payer", which is to say: put everyone on Medicare. Unfortunately, the reason it is so popular is exactly the reason we can't continue it; it's at least fifty percent subsidized, and the government is running out of borrowing power to cover it. In 2011, Medicare spent $550 billion, but its total revenue was $530 billion. That leaves the impression that Medicare debt only increased by $19 billion. Unfortunately, $223 billion of its "revenues" were "transfers from general revenue", which is to say: deficits ten times bigger were made up from general tax revenue. The government borrowed this money, incidentally depleting the so-called trust funds of $19 billion, for a total program deficit of $242 billion. Distributed over the 48 million Medicare beneficiaries, that's an average yearly deficit of over $5000 apiece. The average Medicare subscriber meanwhile shares in Medicare expenditures amounting to about $10,000 a year apiece. (Medicare expenses $10,000 a year per subscriber, program revenue only $5000.) No wonder it is popular. Indeed, since the Department of HHS reports that hospitals across the country routinely surcharge their audited costs by 400% in their claims charges (and patient bills), the public is easily under the illusion that it gets $50,000 of services at a cost to themselves of only $5,000. But the ratio of charges to costs is another matter entirely, taken up later. The point here is that there is a $5,000 subsidy, per Medicare subscriber per year, and there are about 50 million subscribers. These are 2011 statistics; the subsidy is constantly growing, is now the largest domestic contributor to the national deficit, and Obamacare may or may not make it worse.
In 1965 it was possible to look at these matters with more tolerance. In the first place, America had enjoyed a favorable balance of trade with the rest of the world for twenty years since World War II, and could not be expected to realize this balance was about to turn negative, apparently forever. Medicare was then new and untested, and the employer-based insurance community argued strongly and effectively that it had done its fair share without government subsidy. So, it seemed fair for the government to act as payor of last resort for the unpredictable costs of starting the system with a large cohort of elderly -- who immediately had Medicare costs but no prior opportunity to pay any Medicare payroll withholding taxes, the main source of new funds for the program. There had to be a way to pay for the indigent elderly, and the startup costs; and to get it through Congress. Presumably, it was planned to make adjustments and creep up on the deficit, but it never happened. So the designation of "transfers from general revenue" as a revenue source instead of a liability was not an accounting accident or illegal; it was just the complicated new system making optimistic guesses about the future, and guessing wrong. From the beginning, a well-intentioned design generated unsustainable deficits, and no one had the heart to say so. Now that we begin to see we must give up something else to be able to afford to continue on this path, we hear other things are being crowded out. The alternative to facing facts will lead to an unsustainable debt burden, adding force to a recession's artificially suppressed interest rates, potentially leading to a weakened international dollar, eventually raising the unthinkable specter of the dollar losing its status as a reserve currency. It is not necessary to understand monetary policy to understand that an implacable limit to the nation's borrowing -- is beginning to arrive.
When creditors sense they may not be repaid, they raise interest rates, so it gets even harder to "service" the debt. Other valuable parts of the economy cannot pay higher interest rates, so they get "crowded out" of the debt market, or else something they must buy gets crowded out. That's the first sign of serious trouble, and should be taken seriously, because people getting crowded out lose their willingness to help others.
Will Obamacare Reduce the National Debt?
It looks as though the first priority for the Obama administration is the reduction of the national debt. That may not have been the President's initial priority or even his present one, and indeed it probably has been furthest from his mind. However, almost any other priority except national security is likely to be crowded out if the debt is not reduced, and the essence of reducing the national debt is either reducing the Defense Budget or reducing the Healthcare deficit, and there are signs that he would rather reduce security than the health agenda. It does not matter as much as it seems. The cumulative long-term debts of everything the government is involved in will ultimately be reflected in the national debt, and government healthcare deficits are the largest item. If the longterm growth of debt from that source is not constrained, almost everything else is in danger of being crowded out. With restraint in government healthcare costs, attention can be shifted to educational costs, or housing costs, or foreign affairs. Without it, the bond market will dominate what he must do.
 The health of the economy is the main determinant of the whole matter, not the health of the public. 
|
 Unproductive to look closely at direct costs; concentrate attention on the indirect kind. 
|
So what generates the $250 billion deficit? To a large extent, it represents fluctuation in the economy or GDP, about which nothing can be done by insurance auditors, from either the public or private sectors. It does result from an unknown amount of padding in the indirect expenses, and probably a fair amount of imaginative accounting from state Medicaid programs. Hospital administrators complain that there are many unwarranted debts from unpaid deductibles and insurance copayments. And the originators of the Affordable Care Act attribute huge losses to the unpaid bills of uninsured patients.
 We are now engaged in a very contentious stress test to see what the truth is. 
|
Executive Summary.
The Affordable Care Act (Obamacare) is implemented by twenty thousand pages of regulations to be issued by the Secretary of Health, Education and Welfare. They must respond to two thousand pages of laws hastily passed by Congress three years ago. While much remains incomplete, a great deal is known about the coming plan. Are substitute components feasible? Are there potential solutions for the long run, "bending the cost curve downward" after the Affordable Care Act has done whatever it does or doesn't do? Five underlying issues come to the forefront, three of them inherited from the past, and two more added by Obamacare. Discussion of these five items constitutes the bulk of these reflections.
THREE INHERITED ISSUES: Within its announced goal of universal coverage at community rates, the Affordable Care Act built on, and continues to favor, a framework of what preceded it: tax-preferenced, employer-based, service benefits, a mysterious phrase which denotes three inter-connected issues. While the President was entitled to set his own priorities, his reaffirmation means he must actively espouse much of what originally generated the need for reform. In political jargon, by incorporating them within the Affordable Care Act, he owns them.
TWO NEW ISSUES ADDED: The most important question at the present moment is whether mandated universal insurance coverage is both feasible and affordable. Based on theory alone, market-set prices must necessarily disappear as a benchmark for reimbursement -- when everything becomes insured. Unless some additional provision is made, any system which replaces the market by becoming universal must somehow face this issue. The easiest way to retain a marketplace is to leave a large population outside the insurance. Since this would be politically awkward, it is more feasible to exclude a representative component of medical care outside the ring of insurance coverage. And here the most obvious opportunity is to set a higher cash deductible while discouraging supplemental insurance from covering it. Since a small front-end deductible is contemplated for Obamacare anyway, just make it a big one. While it would create some political blow-back, the alternative of ignoring this issue creates an unsustainable need for government price-setting to extend throughout 17% of the Gross Domestic Product, permanently. Because of this issue alone, Obamacare would seem to land on the edge of a Health Savings Account, and should seriously consider going that way entirely. Service benefits could be quite satisfactory retained in the payment of inpatient diagnosis-related groups (DRG), provided it is recognized that certain services like inpatient psychiatry have always proved unsuitable for DRG. In order to retain market-set benchmarks as widely as possible, any other inpatient situations where DRGs are partly unsuitable might be included within the deductible as well, perhaps with small accommodations. And SECOND, as a final last-minute compromise, Obamacare consigned residual uninsured populations to the underfunded (and often poorly administered) state Medicaid programs, to the immediate dismay of state Governors and physicians familiar with existing Medicaid. Health Savings Accounts address both the marketplace and cost issues, simply and quickly. But a second urgent challenge is to bring Medicaid up to speed in the next six months, a daunting prospect indeed, and an expensive one. The administration has seemingly allowed itself to get lost in the weeds of insurance exchanges without a clear and simple insurance design to offer through them. Health Savings Accounts (a savings account linked to catastrophic coverage) afford proven benefits for healthy working people. If the basic plan for ensuring everybody is to give poor people the money, giving them the money takes care of poor people in Health Savings Accounts, too.
STRESS TEST. These two problems -- market pricing destruction, and overwhelmed state Medicaid programs -- readily appear to be deal-breakers because they are newly-created. A more subtle issue is not whether the old problems simply will leave us where we started, but whether the act of universal mandate becomes a stress test which brings out problems which were tolerable with more slack in the system. No one can predict the size and timing of such issues, so it is usually wise to proceed in small steps. Most likely, inherited problems from the old system will indeed emerge as greatly magnified by a universal mandate. The "old" system was business centered, tax preferenced, and delivered service rather than indemnity benefits. It twisted itself and the health industry to help these three requirements endure. With a change in central priorities, the health industry may no longer accommodate them.
So after The Affordable Care Act has been accepted, discarded or modified, the old problems will probably resurface. We suggest here some longer-term goals which could be facilitated by advance preparation for them. Although an essentially unchanged system has accumulated a great many small fixes which need repair, the big ones proposed are these: Eliminate the tax inequity for health insurance based on an employee's type of employer. Any time is the right time to do that. Second, make it easier to migrate from Job Lock and the other problems of employer control, by successively eliminating the advantages of employer-basing. Third, remove the barriers hampering a migration of the (medical office) center of medical care away from tertiary institutions, and toward retirement villages (the principal location of disease). Fourth, utilize the recent advances in large-scale computing to establish a system of individually owned insurance, which can simultaneously subsidize the lingering debts of everyone's first year of life, plus the mostly inevitable expense of everybody's last year of life -- while paying for much of it with investment income during the intervening healthy years of employment.
A number of smaller reforms can additionally be identified, useful in themselves, which would facilitate larger, long-run, goals.
Executive Summary, continued
continues the inequity of denying the same tax exemption to everyone because of the nature of employment, and would be very hard to defend in open public debate, but even equalization will fail to adjust historical disparities in premiums upon transition to universal coverage (because of resistance to rebalancing the pay-packets). Secondly, service benefit compromises which might be tolerated in a private system become dubious within a government mandated one. And thirdly, businesses have outgrown their 20th Century role as a rescuer of vital community service, and now often regard health costs as a growing burden to company competitiveness, which stockholders must be induced to accept. Businesses themselves may be changing perspective and beginning to see the advantages of employee-selected and employee-owned portable health insurance. They may have come to see that employer-basing drove them toward selecting a one-year term model, rather than a lifetime whole-life model, and the employee-owned model is portable between jobs, and able to pay much of its own cost by compounding investment income. Many of the present complaints grow from discontinuity, while continuous coverage greatly reduces the expensive patchwork of multiple insurance forms, pre-existing conditions, uncoordinated successive insurance plans -- and is able to generate investment income, besides. The easiest way to become adjusted to a billing and information system is to avoid frequent changes in the companies running them. Forcing insurance companies to maintain a nationally uniform system is a disruptive way to get there, reduces innovation and competition. Beyond a certain point, people will rebel.
But among the opportunities neglected by mandated universal-coverage at community-rated seem to be: Opportunities for coordinated compound interest to finance coordinated lifetime systems; opportunity to coordinate insurance company information barriers at least enough to eliminate the need for up to three insurance forms to pay for one medical service completely; an opportunity to re-examine the technicalities of traditional patient cost-sharing, thereby downgrading or eliminating ineffective co-pay, but expanding much preferable deductibles buffered by Health Savings Accounts. In the past, many compromises were made to accommodate the highly untraditional insurance concept of service benefits, including bungled but laudable transitions to reimbursement by diagnosis-related groupings. It would be a great mistake, however, to equate this hospital approach with system-wide elimination of fee-for-service. Information systems and cost accounting based on item charges are highly developed and cumbersome to replace; no system outside the acute care hospital has more than experimented with other approaches. It would seem far simpler to modify insurance design to isolate two billing approaches (itemization and capitation) and force them to include, side by side, both office-based care and inpatient services using the same hospital cost accounting data to establish reimbursements. Mandated universal systems can facilitate some of these things, but the real test of democracy is to achieve them without resorting to force.
All of the foregoing areas of omission from the Affordable Care Act should be regarded as areas where improvements in the health administrative system might be possible for either political party to espouse. Therefore, if both parties might agree on some of them, progress might continue even though there is another acrimony in the background. The list of other approaches opened up to examine is probably longer than the average reader has the patience to read, but it includes Last-year of Life escrow, and gradual dispersal of the physical centers of health delivery away from tertiary centers, not toward them. More modest goals and timetables for computerizing physician notes would greatly reduce transition costs for providers. Centralized statistics might thereby be lessened, but the quality of care need not be. The savings from digitizing physician office notes have been greatly overstated, and mostly apply to physician practice aggregates, which inherently magnify communication and record-keeping costs.
Although health reform is now portrayed as a settled decision, the debate which preceded it never anticipated a 50% swing in cost difference between Obamacare and its insurance alternatives. At this time of national financial turmoil, such savings might actually exceed 5% of Gross Domestic Product, thus providing appreciable funds for other urgencies. It seems incredible that such an equilibrium would escape re-examination.
PRIORITIES NOT EXPLORED: Every reformer must choose priorities, but cannot escape criticism for other roads not taken. The chosen highest priority of ensuring everyone with community-wide premiums must also now demonstrate it was achievable without injuring the quality of care. It must also be demonstrated that the commendable goal of spreading expenses widely did not require so much complexity and inflexibility that the delivery system could not keep up with scientific advances. Even if all that can be achieved, the question will remain whether the time and effort might have been better applied to solve a myriad of other healthcare problems which have less to do with insurance. Other problems undiscussed in this paper might have included the financial abandonment of inpatient psychiatry, the unnecessary diversion of non-emergencies into hospital accident rooms in order to retain control of the system within acute care hospitals, unprioritized expenses encouraged by internal hospital cost-shifting, and distorted state budgets encouraged by complex shifting of underfunded hospital Medicaid costs to other payers, especially Medicare. By burying medical costs within insurance, physicians directed to use less expensive methods are denied truly useful information about the cost of components. (That is, not about posted charges, but about what is the true cost.) Item costs are the central signals used, and the present attack on the fee for service offers no substitute signals. The nursing profession is distracted by clerical functions, and its training programs transferred out of hospitals into less meaningful college environments, by reimbursement bundling. The medical profession has seen its overhead costs inflated by compliance with questionable reimbursement requirements, effectively impoverishing primary care, and overcompensating procedural alternatives which can more easily transfer overhead to the hospital. The serious issue of "Job Lock" raised by the earlier Clinton proposal is an inherent component of employer basing, probably continuing as long as employer basing does, and possibly as long as the Tenth Amendment does. The tax inequities for self-employed and small-business employed persons are stubbornly continued, as will be exposed when premiums stabilize. Many of these issues have insurance features because insurance is the dominant method of payment, but they are not considered here as direct consequences of the insurance model. While this list could be extended, its present extent already strains the limits of what can be coherently grouped by sources and causes. This paper confines a critical analysis of those insurance issues where solutions are proposed.
and Generally empowers non-physician administrative control through reimbursement as a means to control rather than assist the higher goal of widespread good medical care.Introduction, continued
Almost three years after the President presented 2500 pages of the proposed health law to Congress for approval, the commentary is hampered because important rules are still unissued. If the program eventually works well, criticism and proposed alternatives may well be set aside. But if enough voters become upset during the early stages of implementation, there will be no escape from the review of other options. To some people alternatives of any sort would seem premature, but here they grow from a preliminary perception that this enormous program has wandered from identifying the basic problem, and thus failed to concentrate on a coherent remedy for solving it.
At its root, the Affordable Care Act is, quite rightly, an insurance reform. Reform of a system is considered to be failing because healthcare costs were rising alarmingly and many citizens had no insurance to buffer them from it. The bulk of citizens did have insurance, and their indifference to cost was considered a cause of the escalation. It was therefore elected to make health insurance universally mandatory and uniform, with government subsidies for those who could not afford it. A unified system would eliminate enough inefficiency to pay for itself, and while some individuals would see higher costs, average lifetime health costs would decline overall, as the peaks and valleys of lifetime costs level out. Governmental control of the insurance system would thereby put it in a position to ignore the nationwide indifference to costs, while its evident power to ration would make rationing unnecessary. More than this was, of course, promised during political campaigns, and more were probably secretly hoped for. But this short summary intends to make the best case for what was offered and will be accepted as the basis for analysis in this paper. If less than the best case makes an appearance, it will be noticed.
Insurance reform is expected to change something, so it seems fair to criticize the Affordable Care Act for accepting three major questionable aspects of the old system, as well as two innovations of its own. Much of this critique will focus on the new problems making the old problems worse, possibly bringing other old problems to the surface, as well. Criticism without offering a substitute is useless, so this paper re-examines Health Savings Accounts in this new environment and finds it actually makes that alternative more attractive. Combined with a repeal of the present tax preference for employer-controlled coverage, these two reforms might be sufficient alternative, with a more gradual beginning. However, the reader is asked to consider the far more ambitious proposal for lifetime, individually owned health policies, universally mandated if you please, with the potential for internally generated investment income to pay for substantial parts of its cost. And the reader is asked to look beyond insurance reform as the way to reduce medical costs without rationing, with the example of moving the center of medical care (physician offices) away from the acute care hospital campus, toward the concentrations of most illness (retirement villages). This latter would largely consist of removing obstacles to where the system seemingly wants to go, anyway. Several other non-insurance reforms are presented in sketchy form, with the urging that most of their seemingly insurance-related features are merely a reflection of present predominant payment routing through insurance, a feature now found in almost anything medical. When they rise to a level embedded in law, they may, of course, require legislative attention to reverse them.
The difficulties it should first correct are distortions of medical care imposed by existing insurance-like financing, searching for a way to conduct a pre-payment system. High costs and failure to include everyone are important issues. But they were only two of many distortions emerging from an employer-based, tax-preferenced, prepayment system. It had been awkwardly forced into an ill-suited term-insurance format long before the present Administration took office. The national clamor of dissatisfaction did not originate out of a united voice of the uninsured population demanding more free coverage, nor was individual cost constraints a central problem for the insured public; rather, clamor mostly originated with third-parties imagining that soaring aggregate costs could be constrained by cost-shifting them, and actuaries endorsing the delusion. Fundamental sources of unrest are to be found in limitations of one-year term insurance itself when applied to a pre-payment process for lifetime expenses -- further complicated by accidentally employer-basing it. Both of these distortions were seriously amplified by uneven bestowal of tax preference, also by accident. The number of small claims is too large to support the claims-processing cost. The size of the premium pool is too small to permit so much free care to be hidden within it because the average premium must not preclude the middle class from affording it. The cost of young and old dependents is rising, the cost of the employee who pays the bill is shrinking, but they are mostly the same people at different ages. The result was unaffordable delivery cost throughout a century of progressively vanishing disease. The health beneficiaries of this process were the patients, with longevity increased by three decades. The financial beneficiaries are also easy to identify. Just count the growing number of non-professionals who are making a living serving it.
On top of all this, a host of new problems are now predictable from additionally striving for universal insurance coverage. In the long history of insurance, there are no precedents to follow, for eliminating market-set prices as a benchmark for insurance reimbursement. The relevant test of whether insurance reform is successful in the end, rests on whether these and other distortions can be improved, ultimately leading to better, less expensive medical care for everyone who needs it, as distinguished from insurance for everyone, payment from no one. Three historic flaws in the existing system might be about to become four. Ominously, present indications are that Obamacare will not only raise aggregate costs appreciably but that at least half of the formerly uninsured population will discover Medicaid coverage was not their idea of an improvement. Unless Medicaid can be significantly and rapidly improved, four problems will become five. The great bulk of problems to be addressed have scarcely been comprehended by non-medical people. For example, no attempt has been made to reconcile more expensive care with more "affordable" care, which would appear to be its opposite. Very likely, medical care difficulties will continue to rankle, no matter how universally Obamacare manages to extend some sort of insurance coverage at a community rate. This time around, the public must insist on a more informed appraisal of the many consequences, of which political consequences are the least important.
------------------------------------------------------------------------------------------ That might sound fair, but it certainly contained political dynamite. Americans prefer individual insurance policies to generational transfers because they distrust the promises of politicians. Americans would surely prefer to own their own policies and take them to their next job if they could. It's not clear that individual health insurance policies are impossible, but they would be difficult to achieve unless they were greatly simplified. One of the great advantages of the Health Savings Account approach is that it would make individual policies a feasible option. It is thus worth a moment to consider the difficulties of employer-basing any kind of health insurance, before going on to the difficulties of present forms of health insurance, regardless of where it is based.
In Summary
In Brief Summary. Suggestions for American healthcare reform are made, embracing the full potential of unencumbered Health Savings Accounts, and changing the physical center of healthcare delivery while turning some of the incentives of reimbursement in a better direction. Unfortunately, most of the intent of the suggested changes to the system cannot be appreciated without understanding the history and economics of health insurance, and the complexities of the modern health delivery system. An attempt to capsulize these matters is mixed among the proposed solutions to them in outline. They come from a physician with decades of practice behind him, fifteen of them before Medicare was created. No claim is made of lack of bias. The more important suggestions are:
A. INSURANCE REVISION
..1. Health Savings Accounts, linked to debit cards, reinsurance, investment vehicles, and marketing. ..2. Elimination of Co-pay, but increase of deductibles. ..3. Equalized tax-exemptions (for health) for all citizens, regardless of employer. ..4. Reduction of employer domination of employee health insurance choices. ..5. Increased deductibles for elective admissions to the hospital (or decreased deductibles for emergencies).B. REIMBURSEMENT REVISION
..6. Revised ambitions for computerized medical records. ..7. Substitution of market-based prices for hospital cost-accounting in DRG calculations and patient bills.C. ACCOUNTING REVISIONS AND APPEALS
..8. Establish a nation-wide appeals mechanism for both beneficiaries and providers. ..9. Independent negotiation and payment for aggregated hospital indirect costs. ..10. Inter-institutional comparisons of charge-to-cost ratios, indirect costs shifts, and indirect costs.(D. LONG-TERM: INDIVIDUALLY OWNED AND SELECTED WHOLE-LIFE FUNDING)
..(11.) Payment of Last year-of-life costs from an escrow to Medicare, beginning last-year-of life pre-funding...(12.) Gradual substitution of whole-life health insurance for term-life health insurance, beginning with first year-of-life post-funding.
..(13.) Encourage migration of office medicine toward the campus of retirement communities. As a beginning, charge some agency with discovering obstacles to moving (independently competing) physician offices to the campuses of Retirement Communities.
Obamacare And Its Repair, Executive Summary
For a while, there was a great air of mystery about why President Obama was in such a hurry to get his healthcare bill through the Democrat-dominated House of Representatives, after passage by a Democrat-majority Senate. There were to be no amendments, and in front of television several thousand pages were dumped on the desks of Congressmen with no amendments permitted, under orders to call a vote within a day. Just read Jacob Hacker's book The Road to Nowhere about the Clinton Plan for Health of ten years earlier, and since Hacker was a campaign advisor for Obama, make a strong guess that Obama was following the same plan -- but encountered a sudden twist. Everybody in the House and Senate had been encouraged to submit his best ideas, so inevitably the House and Senate versions differed so much they had to go to a House-Senate conference committee, also dominated by Democrats. As related by Hacker, the plan was for the President to appear before the conference committee, pick the cherries out of both puddings, and emerge with his health bill. The rest would be discarded as useful camouflage.
Unfortunately, the Senate bill passed but Senator Kennedy died, and to general amazement, a Republican Senator (Scott Brown) was elected to take his seat in Massachusetts. Senator Byrd of West Virginia died soon thereafter, and the ability of the Senate to defeat a filibuster was destroyed while the health bill was half-way through the plan. Since an amended bill would have to be resubmitted to the Senate, it would never pass. So an identical copy of the Senate bill was hammered through the House of Representatives, avoiding the need for a conference committee, and thus avoiding certain defeat in the Senate. So the Obama bill is really the Senate version, containing much baggage which was originally intended to be dropped. And failing to contain some nuggets which would have come from the House bill, which might have made the final product make more sense. Soon afterwards, the House of Representatives suddenly elected sixty-some Tea Party stalwarts, making it absolutely certain that Obama was just going to have to live with the 450 sections of the Senate bill, because these hootin', hollering Congressmen quite naturally supposed that their districts had sent them to Congress to defeat Obamacare, anyway they could. Rather than accept the voters' mandate that Obamacare just wouldn't do, an effort was made to portray the new Republican Congressmen as mindless obstructionists. Which is exactly what they thought the voters wanted them to be. When the Supreme Court then put its foot on the federal government telling the states to take the uninsured into Medicaid, this lesson in what the Tenth Amendment says, was soon followed by the utter failure of the computer programs for the Electronic Insurance Exchanges, and nobody could see what their health plan looked like (or cost), to say nothing of being unable to buy it if they wanted to. Although Section 1251 of the Affordable Care Act assures that everyone could keep his old plan if he preferred it, millions of letters were sent to subscribers who couldn't buy one of the new plans for computer reasons, that their old plans were canceled, while the President confused everybody by repeating the mantra that they could keep their old plans.
Quite soon, employers of more than fifty employees were given a two-year delay in mandated switch-over, echoing the experience which had caused the Clinton Health Plan to be withdrawn a decade earlier, and arousing the suspicion that Big Business was again going to pull out. Individuals were given no such reprieve and naturally were upset about it. Just about every newly offered plan contained a far larger deductible than most people had ever seen and a higher premium than they had ever paid. What made it affordable was the government subsidy, which the computer mess made it difficult to measure. Very few had read the 450 sections of the new law of the Land, and if they had, would have been highly disconcerted. Much of it was never intended to be enacted, but it was impossible to know which sections they were, and so it was not reassuring to be told that the President intended not to implement such unidentified sections. With our troops retreating in Afghanistan and Iraq, and both Syria and Russia conducting acts of war in defiance of us. And the economy still in a slump after five years of "recovery". And the Federal Reserve buying dud bonds by the trillions of dollars worth. And the rest of our allies in worse financial shape than we were -- incompetence was a word on every tongue, to defend against it by the Democrats, to denounce it by every Republican.
So that's where it stands, six months before the next election. In the meantime, I have been working on two projects for real reform of the healthcare system. The first is to improve on the Health Savings Accounts, which John McClaughry and I devised in 1980. The proposal is that since anyone and everyone can start an account, it is universal by definition, portable between jobs, tax-deductible for everyone, and running about 30% cheaper than conventional insurance. I am proposing to expand the program by making Flexible Spending Accounts convertible to it and permitting it to pay the premiums for the deductible catastrophic insurance which is a condition for buying it. Doing so would extend the income tax deduction which you get if your employer buys insurance for you, to everyone. But all of that is without mentioning the astonishing amounts of money that would accumulate from investing the HSA in low-cost index funds of premium American stocks. Nothing is guaranteed, but the experience of the last century is that this approach would assure enough internal income to pay for the entire lifetime healthcare cost of most people who bought it young enough. If you are sixty-four years old, you may have missed most of your chance, but younger people could have quite a windfall. The transition from here to there is pretty technical, and I hope I have not over-simplified it.
The second theme I have pursued is to start listing the many simplifications and cost savings for American healthcare, which I have assembled in sixty years of practicing medicine. What I am suggesting is what real healthcare reform would look like, not just coverage extension. The Congressional Budget Office predicts that spending a trillion dollars will still leave us 30 million uninsured people under the Affordable Care Act. Instead of that, I propose we develop three specialized (and probably non-insurance) programs for 8 million people in jail, 8 million mentally impaired, and twelve million illegal immigrants. Forget about mandatory; if you want to help thirty million people, devise three specialized programs aimed at these three groups, and you have it. Meanwhile, a whole group of flaws was introduced into American health insurance during the last Depression of the 1930s, and they should be repaired. It is preposterous to use three insurance plans to pay for a medical service (80% primary, 20% secondary, plus Major Medical for outliers). First dollar coverage was designed to exploit the Henry Kaiser income tax deduction, which should have been repealed decades ago. Co-pay of 20% has no effect on utilization, and 50% co-pay would infuriate people; co-pay should be abolished. Service benefits mean you never know what your bill is, and never know how much it is going to be; costs escalate. Payment by diagnosis means it doesn't matter how long you stay in the hospital, or how many tests you have, the hospital gets paid the same; consequently, it is essentially a rationing device for inpatients, making hospitals charge emergency room and outpatient services astronomical amounts. And the whole thing has transformed the purpose of health insurance. Nowadays, the real reason to have health insurance is to keep the hospital from fleecing you. Which they have to do, to remain solvent. The list goes on and on, to the point where you have to concede that you can only do so much in a short time. You just have to hold back to keep from overturning the system.
Adam Smith and Karl Marx
|
| Adam Smith |
Ever since the two revolutions, American and French, the Anglo-Saxon world has strongly believed there is no better way to determine fair prices than by marketplace auction. There are, of course, a few situations of market failure which call for government intervention. The continental Europeans tip their caps to this idea, but often revert to central planning of the Napoleonic variety, with its idea that if you have a very smart expert, you should listen to him. We are a nation of immigrants, of course, and so modern American politics quite often divides along lines of preference between market-set prices and central planning. Both systems occasionally fail us, but the native preferences of people mainly divide between faith in central planning and faith in "common sense" market solutions. Our present tangle of opinion about paying for healthcare brings out this distinctive divide. Most of us believe in the marketplace, but in a pickle half of us will give it up pretty quickly and look for expert guidance, while the other half grimly continues to believe "a thing is only worth what you can sell it for."
|
| Karl Marx |
Mitigated individually by compassion and charity, American healthcare prices were always market prices until health insurance made an appearance in the 1920s. The insurance company could employ accountants, but they could not adjust for either quality or personal hardship. The response has been relentlessly in the direction of setting prices as the cost of production plus a standard mark-up. When Lyndon Johnson gave us Medicare and Medicaid, he gave us the accounting approach, in spades. In place of the accounting approach as a check against market failures, he gave us a common sense as a check against accountant errors. For some years, hospital prices haven't seemed quite right. Increasing peculiarities were met by increasing administrative protectiveness keeping the public, even doctors, from getting a sense of satisfaction from increasingly vague responses. Some people are instinctively suspicious, and this sort of behavior brought it out in them. Maybe I'm just like that, but I prefer to think that my views are mostly colored by happening to sit in a congressional hearing room, while Brian McMahon explained the proposed DRG system.
New Foreward
In the early 1980s, American hospitals adopted the remarkable concept of being repaid by Medicare and Medicaid on the basis of the patient's diagnosis, instead of itemized bills for the patient services. The system spread to other health insurance companies, and the diagnosis list was greatly simplified. The result was "Diagnosis-Related Groups" or DRG.
I happened to be in the audience at the Congressional hearing considering this proposal and was initially pleased with what seemed to produce a considerable reduction of paperwork and a potential increase in public understanding. Now proven entirely wrong on both predictions, I am in fact appalled by the changes in medical care DRG provoked. However, I must admit it was a brilliant way for the insurance industry to suppress costs of hospital inpatients. Unfortunately, that was just pushing on a balloon, with the costs bulging out elsewhere. These unexpected consequences were even more devastating because it took so long to understand what was causing them.
Whatever the original motives, the DRG paperwork simplification has proven to be primarily a cost control measure. One illustration of this core theme lies in the way the DRG list itself was simplified. Starting from abandoning the Standard Nomenclature of Diseases and Operations(SNODO, a compendium of well over a million diagnoses) and going to the International Classification of Diseases (ICD) of only several thousand, as a basis, "diagnoses" were reduced to the original DRG set of about 250. Right there, was an unrecognized sign that medical science wouldn't play much of a part in it. Presumably, it was easy to set 250 prices, hard to set a million of them. But both the hospital and the insurance company were really only interested in one thing: what was the aggregate amount of the reimbursement. If they could agree on some approximation, all that medical stuff could be skipped.
Refinements of the DRG list now amount to about three hundred different price numbers, one among which could be assigned to each patient with some sort of medical justification, like "all other". Increasingly, diagnoses were assigned to a particular diagnosis group more because of the similarity of their prices than a similarity of their medical content. Increasingly, all bills were considered automatically fair by the auditors if the grand total of hospital payments was unchanged. Just over the horizon can be seen the approach of matching each DRG to some target based on a budget rather than progress in medical care. The purpose was to hold down the prices of hospitalizations through standardizing them; if the hospital received the same amount of money, what difference did it make? The answer to that question is: we always expected future medical progress to change the cost of care, sometimes up, sometimes down. Regardless of national cost problems, we did not expect the payment system to define the direction of medical care, or for the people most concerned with costs to over-rule the judgments of those primarily concerned with the patient, without even talking to them. Mutual respect and compromise -- now, those are different things. Freezing the revenue stream means if you want something new, you have to give something up. For a hospital of all places to exclude the patient's physician from the trade-off is going to lead to something the patient won't like. Making the physician an employee may silence him, but that only makes the medical catastrophe worse when it surfaces. As shown by recent statistics, the overall profit margin on inpatient hospital patients has remained close to 2%. If that is your only measure of success, the DRG seems a success.
However, a simple example casts doubt on the finality of that decision. Payment based on diagnosis means it no longer makes any difference how long a patient remains in the hospital. Such an effect surely raises costs, but since the price is constrained, the extra cost reappears somewhere else. The same is true of laboratory tests, and bandages, and a whole lot of other costs like cleaning people and computer technicians. So now the burden of holding costs downshifts from the insurance to the hospital itself? Plausible, except that isn't what happened.
What happened was hospitals shifted their sources of revenue toward services not covered under DRG, like the Emergency Room and the outpatient area. They bought up doctor's practices and created satellite clinics. Since no one works as hard for a salary as he would work by being paid piecework, we get a doctor shortage. And consequently, the cost of new medical schools has to be added to the indictment. Since the episodic treatment does not cover an entire illness, it is not and never will be suitable for DRG. And since the hospital administration covers both types of services, it opens the business school opportunity to divert costs to the inpatient area and profits to the outpatient area, while paying big administrative costs to the umbrella organization. Getting hard boiled like that translates somewhere into even greater pain for the indigent and uninsured. Emergency services now have a profit margin of 15%, and outpatient areas now return 30%. Administrator salaries are now in seven figures.
But even that isn't so bad as the trick by which it is accomplished. It's called the Chargemaster, and it has the unfortunate byproduct of dumping the highest charges on the patients who can least afford them, the uninsured ones. When you joke about aspirin tablets which cost twenty dollars, see if you can laugh at bills of $300,000 for treating Hodgkin's Disease, the same conditions for which an insurance company pays 10% of the bill for aspirin or Hodgkins. A famous surgeon friend of mine once muttered, "Nowadays the main reason for having health insurance is to keep the hospital from fleecing you."
Cost Shifting, Reconsidered

|
Cost-shifting is a necessary accounting evil, without which no large organization could survive. Confusingly large amounts of it, however, undermine trust in the leadership. More specific criticism of current healthcare leadership is its reliance on moralizing rather than an apology. That is a sure sign that oppressors (i.e. insurance and government) made it necessary, and suggests that leadership is toadying to them.
Since managers have no choice but to engage in cost-shifting, it seems better to cost-shift with some hope of repayment. By switching to lifetime health insurance to replace the one-year version, many more opportunities can be developed for repaying the older individual what had been "borrowed" from him as a youth. Even without the notion of paying interest on the loan with investment proceeds, it seems more comfortable to seek loan forgiveness from yourself at a later stage of life, if that proves the necessary insurance metaphor.
The proposal to revise insurance architecture also contains a transfer of the site of cost-shifting from hospitals to the external insurance mechanism, where the underlying problems originated. There is a certain justice to that, but its main attraction is to make it visible and consensual, and therefore more generally accepted. It is one thing to convince a classroom of business students, quite another to convince the whole public, of the regrettable need for cost-shifting that will never seem completely fair.
And finally, there is the investment income. The public is no more likely to forgive its mercenary features than it is to accept that bankers are interested in more than profits from the interest on a loan. After all, interest-bearing loans were forbidden by law for centuries. When it first hears of the fairly astonishing 10% return from a passive investment, and the even more astonishing sums to be derived from ninety years of investing, the public will likely scoff at some sort of trickery. A great many people still prefer managed accounts to passive ones, in spite of Professor Ibbottson's rather convincing data from the immediately preceding century.
Two sources of concern are nevertheless impossible to answer. America may lose its dynamism, as even the Roman Empire eventually did, and nothing can withstand the financial consequences. And secondly, so many people might switch to passive investment that it loses its edge, and eventually pays less than hiding all savings in a mattress. That is to say, high returns imply high risk; without risk, there will be no returns. These considerations are long term and have nothing to do with healthcare. For this reason, I have reluctantly made the suggestion that we establish an independent organization, for all its flaws, to study whatever is happening and continuously make mid-course corrections to adjust for it.
54 Blogs
SECOND FOREWORD (Whole-life Health Insurance)
A short summary of the proposal to fund health insurance, so far. The proposal supplements and funds almost any health insurance, and does not replace it.
Foreigners Are Fed Up With Paying Our Bills.
Simple Gifts
'Tis the gift to be simple, 'Tis the gift to be free,
Grand Strategy: Semi-Insured Health Insurance
Post-Payment for The First Year of Life
The First Year of Life, Leading to the Rest

Ideal Universal Health Insurance on the Accordion Model
The outline of ideal universal health insurance is easily stated but bears little resemblance to what we have. It's a pity because we could easily have most of it.
Concerns Provoked by "Whole life" Health Insurance
No Plan is Free of Risk; Long Range Planning is Political
Comparatively Easy Financing for the Uninsured
 The unanticipated consequences may prove to be difficult, but financing the uninsured is pretty simple.
The unanticipated consequences may prove to be difficult, but financing the uninsured is pretty simple.
Increased Potential for Retirement Villages
 Third-party insurance is blocking certain patient preferences, as demonstrated by what rich people prefer to do when they are sick.
Third-party insurance is blocking certain patient preferences, as demonstrated by what rich people prefer to do when they are sick.
Migrating to Retirement Villages

Unfair Income Tax Incentives
 .
.
The Resentfulness of Rejected Benefactors

Evolving Employer Attitudes About Employee Privacy
 Healthcare costs and their insurance reimbursement have grown to a size where they affect the national economy outside their direct scope.
Healthcare costs and their insurance reimbursement have grown to a size where they affect the national economy outside their direct scope.
Correcting the Co-insurance Blunder
New blog 2013-04-09 21:36:41 description
Hospitals' Ratio of Charges to Actual Costs
 New blog 2013-06-12 18:59:30 description
New blog 2013-06-12 18:59:30 description
Loud and Clear: Health Savings Accounts
Co-Insurance (2)
New blog 2013-07-01 16:26:04 description
Cost to Charge Ratio (2)
New blog 2013-07-17 19:12:46 description
Obamacare's Constitutionality
 Obamacare's constitutionality was argued before the U.S. Supreme Court in late March, 2012.
Obamacare's constitutionality was argued before the U.S. Supreme Court in late March, 2012.
Roberts the Second
 Chief Justice John Roberts seems to be intent on radical changes to the Supreme Court, made in a conservative way.
Chief Justice John Roberts seems to be intent on radical changes to the Supreme Court, made in a conservative way.
A Government of Limited Powers

Final Rule: Outpatient Reimbursement Regulations
By gum???
Political Parties, Absent and Unmentionable
 Our Constitution is much praised for exquisitely balancing power between the three branches of government. It would even be an achievement to require two centuries to find a way to unbalance them.
Our Constitution is much praised for exquisitely balancing power between the three branches of government. It would even be an achievement to require two centuries to find a way to unbalance them.
Chicago Sauce on an Arkansas Turkey
The sound-bite is: the Obama health reform proposal of 2009 will extend affordable health insurance to every American (citizen), and save Medicare from ruin by cutting costs. Review of the proposal suggested he should press the reset button.
Picking Out the Raisins From the Pudding
 President Obama's present political pickle is a veritable textbook of the loopholes, traps, and flaws of our legislative system.
President Obama's present political pickle is a veritable textbook of the loopholes, traps, and flaws of our legislative system.
"They Don't Make That, Anymore"
 Pharmaceutical drugs seem to follow a trajectory of fifty years, from new and expensive, to cheap, old and eliminated.
Pharmaceutical drugs seem to follow a trajectory of fifty years, from new and expensive, to cheap, old and eliminated.
An Unending Capacity to Generate New Problems
New blog 2013-06-11 13:51:10 description
Classical Health Savings Accounts (C-HSA)
In a big legislative package, there are technical areas where the lobbyists have considerable sway in the outcome. Here are a few.
Reconstructing the Reconstruction
Only Three Things Wrong With American Healthcare
 What needs to be fixed in American healthcare can be very simply stated as three fundamental problems.
...
What needs to be fixed in American healthcare can be very simply stated as three fundamental problems.
...
What Obamacare Should Say But Doesn't
Here are ten healthcare finance reforms, superior to Obamacare. By far the easiest and most effective is equalizing the tax exemption, now only enjoyed by big employer groups.
Looming Early Issues in Obamacare
 Obamacare is constructed from the regulations issued by the Secretary of Health and Human Services. They respond to the laws passed by Congress which were two thousand pages long. After two years, only the outlines of this program are known. What are the looming issues?
Obamacare is constructed from the regulations issued by the Secretary of Health and Human Services. They respond to the laws passed by Congress which were two thousand pages long. After two years, only the outlines of this program are known. What are the looming issues?
Elective Hospital Admissions: Flexible Deductibles
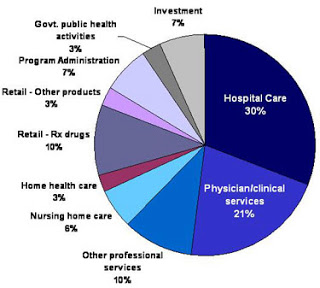 Although deductibles should be applied mainly to outpatient decisions, their most important effect could be on elective hospital admissions.
Although deductibles should be applied mainly to outpatient decisions, their most important effect could be on elective hospital admissions.
The Pharmacy Example.
 New blog 2013-04-19 14:35:18 description
New blog 2013-04-19 14:35:18 description
Taxes as a Form of Consumption
 Most people find taxes are their biggest expense. Why not reduce them?
Most people find taxes are their biggest expense. Why not reduce them?
Rationing, No Matter What You Call It.
 The ethics of healthcare reform concentrate on the ethics of healthcare rationing.
The ethics of healthcare reform concentrate on the ethics of healthcare rationing.
Merging Insurance Companies with Health Delivery Systems
 Competition is the American way, it's what the antitrust law is all about. But in re-designing insurance for healthcare, it would be useful to encourage some vertically integrated pilot experiments.
Competition is the American way, it's what the antitrust law is all about. But in re-designing insurance for healthcare, it would be useful to encourage some vertically integrated pilot experiments.
Addressing the Computerized Medical Record Muddle
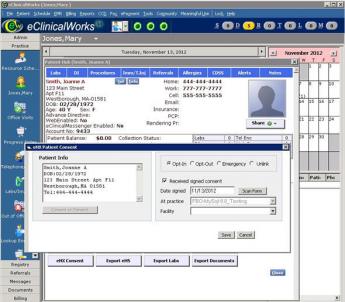 Physicians and patients are unhappy about computerized medical care. Aside from them, everybody is happy with the idea.
Physicians and patients are unhappy about computerized medical care. Aside from them, everybody is happy with the idea.
Physicians Must Dominate Medical Computing Design
New blog 2013-04-19 14:33:21 description
Will Obamacare Reduce the National Debt?
Executive Summary, continued
New blog 2013-06-13 17:45:19 description
Introduction, continued
New blog 2013-06-14 19:33:13 description
In Summary
Suggestions are made for introducing competition, internally funded compound interest, patient cost sharing, and insurance restructuring into Obamacare.
Obamacare And Its Repair, Executive Summary
New Foreward
Why are hospital prices so high?
Cost Shifting, Reconsidered
 New blog 2013-07-16 16:55:35 description
New blog 2013-07-16 16:55:35 description
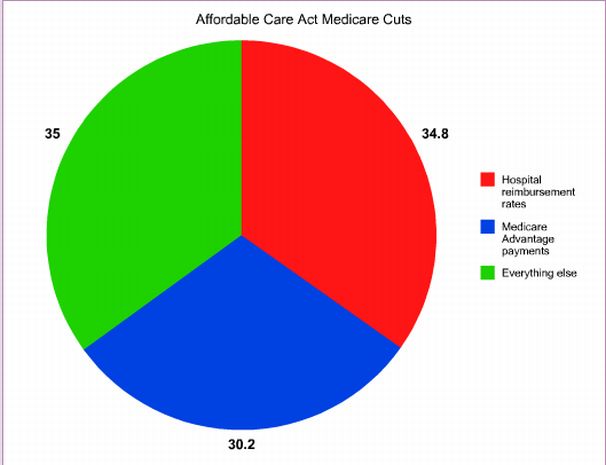 .
.