Related Topics
Reflections on Impending Obamacare
Reform was surely needed to remove distortions imposed on medical care by its financing. The next big questions are what the Affordable Care Act really reforms; and, whether the result will be affordable for the whole nation. Here are some proposals, just in case.
Old Age, Re-designed
A grumpy analysis of future trends from a member of the Grumpy Generation.
Addressing the Computerized Medical Record Muddle
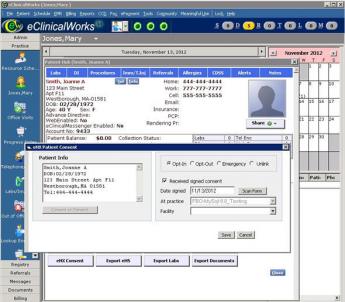
|
| Computerized Medical Record |
Who Should Rule? At first, even physicians were enthusiastic about computers in medicine. The computerized medical record was to have been the smash hit of Obamacare. It promised dozens of efficiencies, vast reductions in cost, and a glittering example of how young minds always see the future clearly while old traditionalists fail to recognize the obvious. However, after the expenditure of millions of dollars of development money, the reaction of doctors to the electronic record now is, "It's a good idea, but it's too much work." What seems to have soured the medical profession most was to discover that the computer designers had cast the model in imitation of the hospital medical record system, largely mirroring the viewpoint of the librarians. Record librarians spend a lot of their time telephoning doctors to come to complete their charts, and have little patience with excuses; they write the stuff, we file it.
Computer designers then brightened up, explaining the wonders of "real time". Compose as you work, let the machine reassemble it, go home at five o'clock. Doctors often wrote a separate composition called Physician Notes, nurses wrote on a different colored paper called Nurses Notes. Nurses notes were usually discarded at discharge until the hospital lawyers forced a stop to suppress evidence. No problem, the computer can easily integrate the two. Unfortunately, the nursing verbiage so heavily outweighed the physician scribble that the dominant emerging discussion consisted of -- what was formerly discarded. The narrative was composed by a couple of dozen people, very few of whom read anything written there except the last entry of his own. It was much like the academic scholar approach, in which a scholar with a new book, first looks in the bibliography to see if his name is there. Otherwise, no one reads bibliographies. When last heard from, this "Progress Notes" approach was headed toward extinction in favor of a "Discharge Summary" written by a single physician, although hospital lawyers still generally insist that the underlying notes be stored indefinitely, as a basis for constructing a legal case against the hospital if the outcome is poor.
All of this was quite bad enough when the system managers started to discover it was easier to get the facts by going straight to the doctor, who promptly labeled the system as "turning the doctor into an input clerk". The famous baseball player Jackie Robinson reached a different conclusion: "Never look back, 'cause something might be gaining on you."
When the computer began to supply a list of medical facts which the doctor had omitted from his recital, refusing to go forward until the missing data got supplied, the situation was getting threatening. One final thing: the medical librarians, naturally seeing the only purpose of filing this data was to retrieve it later, lobbied the reimbursement system that they needed a new code, the International Classification of Diseases (ICD) which reduced a million diagnoses in the Standard Nomenclature of Diseases (SNOMED3) down to no more than ten thousand, with the rest lumped together as "all other" or "not otherwise classified". Very few people understood what librarians were talking about, but when reduced to its essence, they argued that if a disorder wasn't common, it was easier to go the "boneyard" and go through the charts one by one. This transformation took place at the time these codes began to use for reimbursement purposes, resulting in repeated revisions of the code to match the money. It now seems pretty clear that a list of the commonest conditions must eventually revert to a meaningful coding tree if we are ever to escape from using endless high-speed iteration (the underlying process in digital computers) as a basis for finding charts on a shelf.
A brief analysis of user complaints is this: most efficiencies involved some shift of data entry from clerks to physicians, with resulting higher input costs. User-friendliness for patients soon dissolved with the public's awakening they too had expected to be helped, not regimented. Evidently, the designers of the software architecture did not adequately value the points of view of either patient or physician, which seldom match those of the third parties. The design of the computerized medical record evokes memories of the collision between the department store and the housewife in 1978 when only one of the two possessed the terrifying power of an expensive computer and got arrogant about it. In the end, the housewives won that war by fleeing to big box stores in the suburbs. The customer's determination not to deal with a monolithic billing administration under one roof resulted in a redesign of the department store. A subsite two blocks long sold nothing but children's shoes, but at least someone knew something about shoes.
The design of these products should begin, and eventually must finish, with the premise that medical care contains variable degrees of labor intensiveness, each degree following the other in quick succession. In addition, there is the Sherlock Holmes fallacy that a diagnosis is frequently based on a mathematical formula, when in fact most diagnoses are instantaneously recognized by an experienced physician based on what the patient tells him in the first five minutes of an interview. To modify slightly the words of Oliver Wendell Holmes, the life of medicine has not been logic, it has been experienced. The painstaking recording of the features which led to a diagnosis may well assist a beginning medical student studying the case, but they seem like a preposterous waste of time to a busy practitioner. Another clinical maxim for computer design to grapple with is that "More diagnoses are missed because the doctor didn't look, than because the doctor didn't know." Most of the time the doctor does look, and inking a check-block is merely an irritant. In those cases where he doesn't look, the cause is usually that he was either distracted or overworked, but in any case, he doesn't record what he doesn't see. But heaven helps us if he records everything he does see. It's easier to let a computer program recite everything which it is conceivable to see. Take for an example the recent discovery that sleep apnea is caused by the fatness of the tongue, now easily recognized without an MRI. Of what value are a zillion computerized records that the tongue was "normal to inspection"?
The designers should have begun with what is easily automated, like laboratory results, billing, and prescriptions; and only then constructed a useful system around them. A modest system which delights the medical personnel might then have enlarged its sphere when technology caught up to more difficult tasks like summarizing physicians' notes. With doctors of differing levels of personality and experience, little would have been expected until the system offered more in return. It may seem to others that patients will do anything a doctor tells them. But even in that traditional relationship, salesmanship is fine, rigidity is resented. There are many areas where relevant data entry is already automated, so a partial but greatly enhanced medical record is therefore immediately possible. Step by step, the totally digitized medical record could have advanced amidst general applause. This system should therefore re-begin by offering unchallengeable veto power to a large community of physicians, the early adopters, limited additionally to those who have earned the confidence of their colleagues by making a living as practitioners. They must repeatedly defend themselves to colleagues who are not early-adopters, never will be, in order to defend against the accusation they are hobbyists, or secretly nurse conflicts of interest.
That's on the data input side. On the output side, greater respect must be paid to the ability of electronic printers to produce overwhelming masses of reports. They are neat and uniform, but few doctors have time to read them. Doctors must continually devise concise summarizations, paying respect to the rapid obsolescence of relevant information as the case unfolds, rapidly discarding information which only recently was vital to know. At the same time, the system must tolerate a greater repetition of strikingly out-of-bounds reports. Reconciling summarization with redundancy is not an easy task. The ideas for flagging outliers and deleting noise must come from physicians in active practice, who will otherwise resort to adhesive tape, felt pens and alarm clocks. No doubt the requirements of accrediting agencies and the tort industry are in conflict with these notions. If necessary, separate records may be produced for their use and stored in standby locations. No attempt should be made to conceal their acknowledged irrelevance.
The Electronic Medical Record is a fine idea, so long as it limits data entry to material which is already digital, requiring no extra effort to get it into the system. As soon as medical professionals are commanded to touch a keyboard, costs will soar. We have plenty of useful things to do with digital medical data to keep us occupied until medical professional data entry does become feasible, as it must. It might be five years, or it might be ten. But to hurry it up is to cost billions of more dollars, producing very little to show for it. Therefore, the following billion-dollar solution is offered for this multi-billion dollar muddle. It's a Hail, Mary football pass, as would be said in college football.
The Big Data Approach. "Big data" is an unfamiliar term for most readers, but it describes the use of many computers to solve a problem whose data is too large for a single computer to handle. The design reduced itself to a single computer program called Hadoop, itself based on a disarmingly simple idea of splitting a vast amount of data into as many pieces as there are available computers. Soon referred to by non-reverent Google engineers as "Map, shake and merge", the program is free, Amazon will rent 50,000 computers to run a program, taking ten hours to run and costing about $12. Once the approach became feasible, many problems were found which could usefully employ fifty thousand computers at once. Just as happened in a number of computer revolutions of the past fifty years, people in charge of big data projects went wild with enthusiasm. A national Presidential campaign was apparently won by Hadoop. There were spy stories of drones picking out bandits five thousand miles away, and blowing them to pieces (Hollywood, please get busy). One man in Connecticut earned $6 Billion in one year, legally and for himself, and by the report, he was able to make it shake, rattle, and re-emerge. Anyone in charge of huge amounts of data is in a position to produce something pretty astounding with it. However, this sort of thing often ends in tears, and all hard reality lies under a mantle of jovial simplicity.
Beyond a certain point, most of the limiting factors preventing still further use of hundreds of thousands of computers reside in coordinating the symphony. If a computer has one electrical failure every thousand hours of use, fifty thousand will have fifty failures per hour, and just fixing the flaws becomes a new problem to address. Even without failures, the computers get out of synchronization pretty regularly. So although big data gets more powerful with increasing size, it develops new challenges. Nevertheless, it turns the science of statistics inside out, since it is often easier to count the whole thing than to take samples and estimate an aggregate result from them. So to speak, it becomes easier to take a preliminary vote of the whole electorate than to use Gallop Polls. Astronomy, chromosome research, weather prediction, opinions, styles, and tastes are only a small fraction of areas of interest which generate more data that can be readily managed with a single computer. Obviously, the stock market is another area which generates huge volumes of data, but simultaneously increases the incentives for secrecy, and pays its employees more than colleges can pay professors to popularize the techniques. The huge volume of data which can be expected to emerge from computerized medical records universally applied, will, therefore, present a huge opportunity, but one now held back by non-scientific incentives as well as serious privacy issues. We assume there is something of value to be learned by mining this data but we cannot be sure of it in advance. Nor can we be sure whether asking trivial questions, like determining the average square root of the nation's Social Security numbers, will make this enterprise the butt of every joke. Big data is the general approach of certain Wall Street hedge funds who have made astonishing amounts of money, much envied and imitated by other Wall Street firms who have only lost huge amounts of money. It is at the heart of the Google search engine, and rumor has it that Amazon is far advanced in the business of assembling and renting out gigantic computer farms to people who think they have a Big Idea and assemble cash to use a computer farm for ten minutes or so.
It seems perfectly certain the Big Data approach will be explored on this tempting mountain of medical data, which no one will be quite sure how to exploit. Much of the future of the approach will depend on its luck in discovering something strikingly useful during the early stages because the cost of it can be so quickly calculated.
What Purpose is Served? Whether big data techniques have any general utility for medical care is not certain. Big questions, like the distribution of diabetes among people who are overweight, can be answered by occasional investigations, or at most a few institutes committed to the task and reduced to a few sentences in a textbook. Only if utility in everyday use can be personally confirmed by almost every physician, will the original design of the Electronic Medical Record prove to be useful? No doubt, computers will shrink to the size of a walnut, and no doubt enormous surveillance systems can be designed for uses which plaintiff lawyers, consumer complaints, the patent infringement industry, and reimbursement oversight can best describe. No doubt it would detect the practice of medicine without a license, failure to maintain continuing education credits, and probably a dozen other investigations of suspicions. Bur all of these intrusions will be frustrated until someone devises a way to induce physicians to use computers in their everyday practice. For transmitting laboratory reports quickly, that day has already dawned; physicians would be very grateful to see a system created which would notify them of matters needing instant attention no matter where the doctor happens to be, including the toilet. Even the disruptive effect on the family life of being constantly on call can be tolerated if such an important service is created. But the dreams of the electronic record enthusiasts went far beyond that, in two principal ways.
The aspiration to be complete made the doctor into a clerk, cutting out the middleman who happened to be his secretary, nurse or assistant, and furthermore created an easy way to monitor whether he had fallen behind in supervision. And secondly, it created mountains of information which even in summary form, the doctor had no time to read . For doctors practicing in large group practices, addressing these two issues had been a growing necessity for quite a few years and was now seized upon by such organizations as a way to cope with their largest source of inefficiency. Doctors in private practice usually organized their own systems to avoid such issues, but now a solution for group practices is forcing solo practitioners out of business, because of a perceived need to be universal. At the other extreme, solo country doctors once had no need for such archives, and certainly had no time to cope with such demands on his time. Reducing someone else's profession to a vast array of yes-no answers soon taught the lesson that the task was not likely to be generally satisfactory for another decade, so some reformers were unwise enough to suggest the medical profession should be redesigned top to bottom to accommodate the issue. Making suggestions like that in Alaska, Wyoming, Texas, and other far-flung territories only lead to the election of physicians as congressmen in those districts, surely a worrisome thought for progressives. But in other areas, such resistance was seen as a sign that fee-for-service practice was a sign of wickedness. A more reasoned stance would be: Waiting a decade with such suggestions until the doctors in group practices can influence computer re-design, would leave time for the medical profession to adjust to many other urgent matters, first. (The next and final chapter address the direction we might consider if we really are prepared to redesign the whole system).
Originally published: Friday, April 19, 2013; most-recently modified: Sunday, July 21, 2019