3 Volumes
HEALTH SAVINGS ACCOUNT: New Visions for Prosperity
If you read it fast, this is a one-page, five-minute, summary of Health Savings Accounts.
Second Edition, Greater Savings.
The book, Health Savings Account: Planning for Prosperity is here revised, making N-HSA a completed intermediate step. Whether to go faster to Retired Life is left undecided until it becomes clearer what reception earlier steps receive. There is a difficult transition ahead of any of these proposals. On the other hand, transition must be accomplished, so Congress may prefer more speculation about destination.
Consolidated Health Reform Volume
To unjumble topics
SECTION TWO: Hidden Economics of Healthcare
Here are samplings of the reasons Healthcare Reform still isn't going anywhere.
We started this book with high cost as the main driver of public concern about healthcare. Our proposed alternative is the Health Savings Account. However, a central disappointment in the Affordable Care Act grows out of neglecting almost everything the matter with the system, besides cost, especially the cost to poor people. Many problems can not be cured by spending more tax money, directly or indirectly, and they deserve some time in the debate. We therefore pause to review a number of other issues which are perhaps less obvious, but not necessarily less serious. Chief among them is the employer-based system, which once served us well, but is wearing out its welcome.
The same might be said of Medicare, but that topic is treated later in the book.
Second Edition: The Coming Shape of American Healthcare
There are plenty of problems with American health financing, but three features are the basis for optimism and the subject of this book. The first is the possibility that research can get us out of the jam we are in. The National Institutes of Health has started to prioritize its research, sensibly focusing on the most expensive diseases first. Opportunities will always dictate the attractiveness of a particular line of research to the investigator, but to the extent, a funder can influence choices, the N.I.H. has started to put a priority on the cost of diseases that cost the most to treat. It is their estimate that eighty percent of healthcare expenditures can be roughly assigned to only six diseases (Cancer, Diabetes, Parkinsonism, Arteriosclerosis, self-inflicted Conditions, and Psychosis.) If somebody gets us an inexpensive cure for only one of them, it would have a big impact on costs. At the moment, the best estimate of lifetime health costs is roughly three-hundred fifty thousand dollars per person, in the year 2000 dollars. By spending the present annual 33 billion dollars on research, it seems reasonable to look for a decline in health costs in the next decade, after which even research costs should decline. Expense is most heavily influenced by the need to institutionalize certain situations. I once wrote a paper on the patients in the Pennsylvania Hospital on July 4, 1776, and the diagnoses were remarkably similar to the present time, concentrating on disorders of the legs and brain, where you have to be put into bed to be cared for.
One thing we can, of course, be very sure of: everyone will eventually die, and thus will have one terminal illness. We can eliminate any or all five-- and you can be sure that something fatal will take their places, although you can't be sure it will be cheaper to treat. Nevertheless, longevity will lengthen, making healthcare cheaper, per unit of longevity. Perhaps the way to put this is to aim for only one fatal condition per lifetime and to re-design our insurance to anticipate this direction of things. As a side consequence, the longer you delay the grim reaper, the more income will be generated within Health Savings Accounts, more patents and copyrights will expire, more drug competition will lower costs. Unfortunately, the longer you live, the more it will also cost to extend that retirement. The resulting certainty is for greater consumption pushed into old age, and the likelihood is, more money will be spent on living expenses and less on sickness expenses. Any way you turn it, Social Security or it's equivalent will need more money, and Medicare or its equivalent will probably need less.
In later sections of this book, we discuss the creation of last-year-of-life insurance, as a re-insurance step to make this transition more automatic and less a debate about fairness. It takes decades to grow this fund to the point where it can accomplish its intended goal, so if we procrastinate, the problem will someday be upon us, leaving too little time to get it started. In the meantime, it's entirely possible to spend the premium money on short-term expenses, leaving it to our children and grandchildren to worry about. Since it's absurd to suppose toddlers and grammar-school children can be persuaded to fund their retirement by agreeing to consume fewer lollipops, it seems likely the first-movers will be well-to-do-parents, seeing an opportunity to escape taxes or refund future expenses of their own, like college tuition. And then, we might play the counter-cyclic game with the economy. Ingenuity might be applied to linking immigration quotas to domestic unemployment, or top-heavy stock markets. The worse our unemployment pool becomes, the less we need immigrants, and the more we need surplus cash for retirement endowment. If we are destined to have a fairness argument about prefunding retirement, let it be based on considerations like this. At least it has the potential to set ground-rules far in advance and can demonstrate what is politically feasible. For many decades it will be impossible to guess what future costs will look like. but meanwhile, actuaries and statisticians will be encouraged to speculate on how well we are doing, and how much individuals will have to supplement from their own resources. Newsmedia will have room to find examples of people who gambled and lost, or gambled and won, or what is likely to happen to everybody who ignores the problem.
The second optimistic direction to take has been known since Aristotle. Compound interest thrives on increased longevity. Ever since the pirate ships of the sixteenth century, our country has resisted the simple teachings of this mathematical assertion. In the past thirty years, we have crossed over the bend in the curve where it really is possible to derive astonishing multiplications of assets, simply by living as long as most people now survive. Never mind the trivial or even negative interest rates imposed by the Federal Reserve. The Fed has the mandate to maintain stable prices, and it will return to it, after a brief interval of praising inflation as a useful tool to manage a recession. The sixteenth-century pirates liked shares better than gold because they never could tell in advance when a sail they were pursuing into harm's way was a rich prize or a molasses barge. If we had to, we could base our currency on common stock index funds just as well as on debt or credit, and after a brief turmoil, things would be much the same.
And finally, we are edging toward a recognition that healthcare ought to enjoy a common tax exemption. We aren't there yet, but the tax exemption of Health Savings Accounts could close most of the gap for all Americans, and it has already made considerable progress. You could close the gap entirely by the passage of a one-line amendment, but you could also essentially close it by extending Health Savings Account deposit accounts to the point where differences were no longer worth fighting over. Once again, we have crossed an invisible line. When the public sector grows to be more than a quarter of the Gross Domestic Product, tax preferences become dominant and are no longer tolerable. We aren't going to shrink the public sector appreciably, we can't grow the GDP even up to a 2% growth target. So increasing the tax exemption is about all that is left.
We might, if you like, add a fourth direction to take. At 18% of the GDP, healthcare is too large to be distorted by a linkage to employment. Everybody naturally is reluctant to threaten a gift of 20% of his income; indeed, it would seem monster ingratitude to do so. Even though we know it is unfair (after all, life is unfair), and it makes the whole structure unsound to balance the health cost of the whole nation on the one-third of the population which is working -- and on less than half of that third -- who mostly aren't particularly sick. This can't last, folks, and you can say you read it here, first.
Employer Based Health Insurance
In 1965, the most fundamental of economic fundamentals reversed itself. America's international trade balance shifted from positive to negative, has remained negative ever since. It's irrelevant that international currency shifted backward to soften the blow; that's what floating currencies are supposed to do. The era of effortless and largely unchallenged American post-war world supremacy was over. From now on, it was to be everyone for himself, in Medicine as in every other trade.
A new triumvirate, consisting of hospitals, health insurance, and medical schools asserted medical leadership, fought against each other for domination, and consequently found themselves a prized destination for opportunists. The new name of the game was to gain control of the payment system, and through it control of hospitals, and through the control of the doctors. But the sponsors of the earlier system, the employer-based one, were still around, and to a large extent, still, dominate. No proposal for running healthcare could omit physicians from the center of control. Most who attempt it, seek to use medical schools as a surrogate for the practicing profession. However, medical schools are in competition with their alumni by owning hospitals, and the rest of the profession see medical school control as favoring a competitor. They resist it bitterly.
Meanwhile, the doctors had experienced entirely different socialization by going away to various wars, and discovering how little they needed hospitals. As shown in episodes of the TV series Mash, new bonds were formed between a medical band of brothers, operating successfully in tents, not medical centers. This experience comes and goes, but unfortunately, there has been such a succession of wars, the experience gets reinforced. One of the great paradoxes of the present medical upheaval is to see government and insurance doing their best to herd doctors back into hospitals so they can be controlled by salaries, rather than by their patients. And while they seem to have largely succeeded, the ACA ambition to control medical care by control of the payment system is appreciably undermined at its interface between institution and profession. It is always an uphill battle, to defend a more expensive, less satisfying, approach; eventually, it is a losing approach. The oppressive cost of everything, the collision between recessions and inflations, seemed to be keeping everybody under control for the time being. But it would be unwise to assume calm will prevail forever, or that a command-and-control arrangement would continue to work through the hospital, without fragmenting somewhere. In a larger sense, a lot of this history was irrelevant. The people really causing commotion were business leaders with an entirely different agenda; their model was Henry J. Kaiser.
Much of the resulting endgame depends on what Washington will be willing to do. Congress will have its own ideas, but Congress is often in a hurry. What isn't complicated, is often politically difficult, and it helps things along if the public has thought about them first. The Supreme Court gives itself more leisure to think, but sometimes that isn't a pure advantage. The President has more staff, but he can't always control it. Medical cost-cutting turns out to be like closing military bases; it has to be gradual, it has to be spread wide and thin, but it must show early benefits quickly. In its first six years, for example, a lot of people must see some benefit, and very few must see their jobs destroyed. All this can be done, but it can't be done repeatedly. The country cannot afford to keep using up its reserves with noble experiments. World affairs and world economics surely present enough distractions, without inventing artificial ones.
On medical affairs, Congress should learn to listen more to doctors and less to our ancillaries. But for this to happen, doctors will have to become more open about their experiences, rather than electing more doctors to Congress, where they become seen as competitors rather than experts. When Congress finally wakes up to the full dimension of what has happened, everybody is going to need some friends he can trust.
In the final section of this book, we will talk a little about some of the thorny transition problems to be expected. It's not a comprehensive discussion, but a wake-up to the healthcare industry and to Congress, about the complexity of some of the implementation problems they are abandoning to the Executive Branch -- at everyone's peril.
So, come along, let's learn a few hidden things. Start with employer-based health insurance. That's what we had for the past century but hardly noticed it. It even helps to know a little of its history.
A Short History of Employer-based Health Insurance. Instead of starting with Bismarck or some other link to a non-American, let's say health insurance in America began as a proposal of Teddy Roosevelt's during the Progressive Era just before the First World War, a century ago. The American Medical Association had a flirtation with Teddy's national health insurance but came to prefer something like the business community's Blue Cross system, as it eventually evolved during the 1920s. Business scarcely recognized it, but large American companies were beginning to shift control from founding families to stockholders, an evolution which advanced during the next three decades, as a way to extract capital gains taxes to float war debts. To a certain degree, growing shareholder control was a step toward meritocracy; in a human relations sense, it may have been a step backward. The shift extends to only about half of corporations even today. But health insurance and stockholder control of the big companies advanced side by side, scarcely realizing how diminished employer benevolence was undermining the process. We glorified the decline of a semi-feudal system, but we lost something in the process.
 American health insurance traces back to President Teddy Roosevelt 
|
It makes a huge difference whether the boss is a paternalistic owner or the manager of someone else's company. In the first instance, he spends his own money, in the other instance, his only absolute mandate is to generate money for the stockholders. That's a measurement applied to every "good" manager. Plenty of owners were tight-fisted, and plenty of managers were benevolent. Even today, small businesses (less than a billion dollars in assets) are mostly "Subchapter S" corporations, and about 15% of really large "Subchapter C" corporations are still dominated by founding families. But in spite of frenzied rhetoric about the "rich owner", the shift in attitudes is clear; as founding generations move away from active involvement in their companies, they become less involved with employees. They themselves become more like their hired managers. Current investment trends, moving into index fund passive investing, further widen the distance between stockholders and owners-by-inheritance. The "silo effect" of specialized departments further isolates the core business from non-revenue support departments.
Cost-shifting was an early development, transferred from the business to the hospital. The concept originally underlying Blue Cross was that private rooms should produce enough profit for the hospital to support the poor folks in open wards, whereas semi-private rooms just break even. At first, only a handful of ministers and school teachers were in the semi-private category. When hospital finances improved, more working-class people moved into the semi-private category, the wards shrank in size, and semi-private -- became the standard clause in employee contracts. For two hundred years, multi-bed open wards were standard, but semi-private became standard in a single decade. Semi-private nevertheless acquired a charity flavor. The "Blue Cross discount" began to apply to semi-private beds, at the same time semi-private became readjusted to become "standard size" for "service benefits". That is, most employees of corporations started to be cared for at less than actual cost, at the Blue Cross discount-to-business rate, because their contract called for being provided certain services, no matter what they cost. In fact, what they appeared to cost was so distorted by cost-shifting, you couldn't tell who was subsidized. It would not take long for a new standard to be demanded: sharing a room with strangers was so low-class. Private rooms were going to be the only decent thing. Spending other people's money is fun.
And because Blue Cross organizations became dominant during the Second World War, their competitors in cash benefits ("indemnity carriers") greatly resented paying more dollars for the same semi-private room than Blue Cross patients did. Some of this was doubtless a response to wage and price controls during World War II, a way of raising wages without expanding the (taxable) "pay packet". The response of commercial indemnity carriers was to price their premiums on "experience rating", which especially cut into the profit margin of Blue Cross private-bed patients. The way that worked was, the insurer waited a year to see what inflation had done, and made a trailing readjustment in the following year's premium. One unexpected outcome of this price warfare was to make the hospital reluctant to reveal its tentative charges, where the employer demanded to be shown the actual costs of his employees, as well as prices to everybody else. When Blue Cross coverage reached government employees, a new power center gained possession of itemized hospital bills. A new employee representative could easily see how much or how little the government was actually subsidizing charity care. Naturally, as the new source of benevolence, they claimed they were paying too much.
When Group practices, or HMOs, started to pay for healthcare, they too demanded to see comparable bills or at least standardized prices. And so it went, with each new wrinkle in payment. Some people paid listed prices, but big groups could afford to send auditors to look at the books. There had long been a three-tier price list, and now there was a six-tier one because of having list prices and actual payments on each of three levels. Soon it began to seem there might be sixty prices for the same thing. Like a stag cornered by barking dogs, the hospital fended off the payers as best it could. Because of the long period of catch-up following the Great Depression and then the Second World War, hospitals usually needed new buildings and improved wage standards for employees. How were they to pay for this, when everybody seemed to be demanding to get backlogged services at the old prices?
For centuries, hospitals had existed on a system of collecting whatever they could, and delivering needed care as best they were able. Their deficits were covered by public subscription, by religions, and by tightening the belts of the charity-minded hospital volunteers. Sometimes the rich guy who lived in a mansion on the hill would donate, sometimes he wouldn't. Surely, the government had a responsibility to rescue such a deserving charity. The student nurses and the young doctors in white worked for no pay at all. That's right, after I graduated from medical school I worked for four years without a dime of pay. If hospitals overcharged a few insurance companies, well, there was nothing else they could do to keep the doors open. Until health insurance made a significant impact, hospitals ruled medical care. They were the only institutions which seemed to work, all new ideas seemed to come from them, and any new idea which came along was somehow centered within hospitals. Although it wasn't described as such, hospitals began to suffer the disease of conglomerates. If an organization takes on too many functions at once, it performs some of them poorly. Usually, one of the subsidiaries fails and drags the rest of the conglomerate down. That's essentially why the Supreme Court, in the State Oil v. Khan case finally decided vertical integration cures itself and usually does not require antitrust judicial action to break it up. That doesn't mean vertical integration is wonderful; it just has to be shown to be bad before you punish it. Unfortunately, high legal fees unbalance the situation. The corporation can usually afford the lawyers, the individual practitioner can't. Threatening to bankrupt the opponent is now a standard procedure in the courts of Justice.
Disregard for the Tenth Amendment in the 1937 Court-packing incident greatly injured the Tenth Amendment's Constitutional requirement that health and health-related activities should be regulated at the state level. But it also heightened public attention on the Constitutional issue, since hospitals, nurses, doctors, pharmacies, and the Blue Cross organizations were all organized along state lines. Only when the Federal government under Harry Truman began to sound serious about central control of medical care, did health insurance begin to cross state lines, and thus weakened hospital and Blue Cross domination of it. By the time Lyndon Johnson began his piecemeal assault in 1965 with Medicare and Medicaid, the insurance industry had broken healthcare into four "markets":
Large-employer groups. The healthiest groups, and hence the cheapest to insure, became the low-hanging fruit. Union pressure combined with the passage of ERISA expanded and somewhat fragmented the groups, but large employers were first and dominant in the planning.
Small-employer groups. Curiously, this often became the most expensive silo of the markets, because of successful pressure to expand -- even mandate -- benefit packages, and the fact that certain expensive cost generators can be selectively insured when the personnel manager knows them by name.
Individuals. Because of adverse self-selection, "non-group" had the highest marketing costs, and often the highest medical costs. It was possible to eliminate the worst abuses, such as figuratively buying insurance while riding to the hospital in an ambulance. But subscribers to non-group insurance move freely between employers and thus can avoid being dropped from the insurance when they change jobs. What is generally touted as a great disadvantage of employer-based insurance, could easily be called the exploitation of being in a position to select only healthy people for jobs. Insurance companies obviously and regularly "prefer to work with groups". Circumvention wears many disguises. When an insurer tells you this is "his company's policy", be sure to kick him in the shins. His company is part of the problem, not part of the solution.
Executive "Cadillac" plans. are mentioned for completeness, although they could also be grouped with steak dinners and baseball tickets, as mere sales promotion kickbacks for the people who make decisions on behalf of members of a large group. They often had "first dollar coverage", essentially paying for everything even faintly describable as medical care, down to the last penny. It should prompt some concern to learn that health insurance for college professors and politicians is often of this variety. In terms of aggregate medical cost, of course, Cadillac plans are negligible. However, as long as they exist, they light the way for those fortunate who can focus on Henry Kaiser gimmicks rather than the treatment of illness and eventually migrate to the rest of the tax-deductible group.
The general purpose of market stratification is to offer much the same product at different prices. Like other concessions which vice makes to virtue, they constrain admiration for the essential, desirable, feature of insurance in the first place: it spreads the risk and lessens the cost of what is supposedly an unpredictable random health catastrophe. If the insurance industry is really serious about this mission, it would start with one outstanding example of it: catastrophic coverage. Remember, the higher the deductible, the lower the premium. Let's repeat that: the higher the deductible, the lower the premium. Are insurance companies really motivated to have lower premiums? That's like saying Insurance Companies want to lower legal costs in order to preserve the impartiality of the courts.
Almost nobody can withstand a million-dollar illness, but almost anybody can afford a hundred dollars a year. Once you have that minimum feature, you can then start to talk about more expensive, more common coverage -- until we eventually reach first-dollar coverage for non-essentials, at wildly unaffordable premiums. By the way, if you would like to know why I didn't acquire catastrophic coverage back in the days when it was widely available, it was because I already had first-dollar coverage given to me by the University where I worked, I couldn't use extra catastrophic coverage even if it was free. This is no longer pre-1965. Everyone should have catastrophic coverage. Only if he can afford it, should anyone have more than that? Since the logic is beyond dispute, has it occurred to anyone to ask why that isn't the usual case? Read on.
Henry Kaiser's Cleverness Out of Control
The Henry Kaiser caper. In 1943 during the Second World War, Henry Kaiser has given "Liberty Ship" contracts to build freighters for the Pacific Theater. To build ships in East Coast shipyards was to invite German U-boats to sink them as they headed for the Panama Canal. There was a price-control mandate from the War Production Board, seeking to restrain wartime inflation by prohibiting raises or bonuses. So Kaiser protested he had difficulty attracting steelworkers to California because he could not offer incentives to move. By whatever means of persuasion, Kaiser was able to obtain an exemption, permitting him to treat healthcare fringe benefits as non-salary, thus exempt from income taxation. As Cicero noticed, "In times of war, the Law falls silent." Other expedients may have been allowed, just in order to win the war, but such loopholes were apparently closed after victory was achieved. This one persisted.

|
| Henry J. Kaiser |
In later post-war years, just exactly who negotiated with whom remains unclear, but in essence, the IRS continued to treat employer health benefits as tax-exempt gifts and still does, eighty years later -- provided the employer pays the premium. This unintended post-war extension is fiercely defended by organized labor whenever someone brings it up, and they are quietly supported by the management of a big business. Congressmen are scared of the whole subject because of bad experiences with united lobbying, linking unions, and big business. In Washington, such an alliance unites the support of the leaders of both political parties. It must be mentioned here that Government itself is one of the biggest beneficiaries, acting as a huge employer offering fringe benefits, itself. Consequently, Congress itself finds it has a conflict of interest when the subject is on the floor.
 The ones carrying the placards are seldom running the show. 
|
| Protest Politics |
The clamor to retain this tax ruse is joined by non-profit charities and state, local and federal businesses, who are included in the favored tax-excluded group -- even though it would appear the employers do not share in this feature. Their revenues are often fixed, and their budgets have shifted to expect this gift; consequently, their noise is equally loud when discontinuation is suggested. My own medical society employees participate. As James Madison feared when he designed the Constitution, the number in the wagon being pulled outnumber the people pulling the wagon. In the lobbying case, the ones carrying the placards are seldom the ones running the show, and seldom fully understand the issue.
Small businesses are entitled to the tax exemption but many do not avail themselves of the opportunity when they discover premium rates for their group of employees are often higher than the individual rate. Furthermore, small businesses are overall less dependably profitable than big ones, so their tax rates are usually lower. The essence of the self-interest of big business for "employee" health benefits tends to concentrate in those companies who make big profits, and thus pay high corporate taxes; less profitable businesses have less tax liability to play games with. Things take time to emerge, but after eighty years there has been plenty of time for the "gift" to be taken for granted, and the pay packet gradually adjusted to recognize that fact. Nothing remains to justify it except the tax deduction.
While it is hard to be precise, it is obvious that when things get less expensive they attract more buyers. Generally speaking, higher-wage businesses have lower health insurance premiums, because they can be more selective in their hiring, partly as a consequence of lower costs in their experience rating. Moreover, if an employee somehow gets a gift of his insurance premium, his employer actually saves more than he does, although less attention gets drawn to it. If there is anything a big business gets fierce about, it is to be deprived of savings which seem to result from its own cleverness. In this case, that argument seems more acceptable than it really is, since the benefit is now almost exclusively sustained by lobbying. The employee would have had to pay a higher income tax on a higher salary if he bought his own insurance with after-tax dollars. But that tax is based on his gross before-tax cost, including Social Security, Medicare, and other assessments, which the employer pays less of, on a lowered salary. Nor must he pay half of this and half of that, itemized on the pay stub, in matching money. This part of his cost is reduced by about 35% when he gives away the health insurance, and everything else is a tax wash. That is, other taxes have been warped to take advantage of the tax exclusion, with the result the employer community is not entirely unwilling to have unions demand they be coordinated that way.
The overall result is both employee and employer are better off than by just a straight tax deduction on the insurance premium, while the employer is far better off because he can multiply it by the number of his employees. Google, for example, has 55,000 employees, some of whom are paid extraordinary salaries. And then, the employer's tax deduction is against a 40% tax rate instead of against a blended tax rate for the employees of perhaps 20%. And finally, the insurance premium is reduced below the individual rate by forming a group and demanding hospital discounts. All of this is the result of gifting health insurance premiums on behalf of the employees. For executives with a very high salary, it can probably accomplish remarkable savings for the shareholders by giving the executive a Cadillac plan. Because it makes a good smoke-screen, no one troubles to correct wide-spread misapprehensions, especially among others who are already tax-exempt.
 Gifts to employees are more tax-sheltered than equivalent salary would be. 
|
Indeed, a little multiplication is convincing that tax abatement is not only supporting a substantial proportion of health insurance, but it represents a noticeable portion of corporate profits. So, although a major portion of this distortion would soon readjust to a new climate of opinion, any move in the direction of removing it abruptly would probably unnerve the stock market for an indeterminate time. It took eighty years to build up to this condition, and it cannot be corrected in a few days. It would, therefore, be important to have a solution to it, ready to be announced. Here's my proposal.
Proposal 4: That a schedule of reduction of both the tax exemption of employer-based health insurance and the corporate income tax be prepared along the following lines: That in consultation with economists, the corporate income tax rate be reduced until it matches the average blended individual tax rate. And the tax exemption for employer-based health insurance be reduced in a step-wise fashion until it disappears. The process shall take no longer than three (3) tax years, keep the two reductions in balance, and be commented upon by the Federal Reserve, and overseen by an appropriate committee of both House and Senate.While it is conventional to ascribe a tax evasion to the employee and to blame it on those dreadful unions, the employer gets somewhat more tax benefit than each employee, multiplied by thousands of employees in the bigger firms -- but it's just a tax dodge for both shareholders and employees, with the shareholders coming out somewhat ahead. Nevertheless, the employer advantage mostly derives from comparing an individual employee gain with an aggregated corporation gain. It may reflect union salesmanship that the aggregate employee gain is usually not displayed since that immediately makes the two more nearly equal.
Since salesmanship has come up, I might as well apply a little of it to my own proposal. I believe sober analysis reaches the conclusion that the tax exemption is about all that matters, to anyone. Following the proposal, the government would gain taxes and corporation stakeholders would have to pay them. The shareholders would be compensated by a corporate tax reduction, but the employees would not. Although the employer might argue either side, the employees would be the ones who would surely complain. But let's take it another step.
Let's recall what happened in Ireland when the corporate tax rate was reduced to 12.5% in 1983 from its former rate of 50% in 1982. Essentially nothing happened to government revenue, which has only varied at much as 10% between 1975 and 2015. There was hardly a ripple in 1983. That's not to say nothing happened, it just did not affect government revenue much. For that to be the case, it is mathematically necessary to have more corporations, each paying less tax. That's indeed what seemed to happen, but it took twenty years to convulse the Irish economy, starting from a comparatively low level. Ireland is mostly a rural nation, and new corporations came in from abroad (UK and Scandinavia, mostly) to locate primarily in Dublin, as city dwellers. That started a housing boom, which required mortgages, and eventually toppled the banks. The
Irish corporate tax rates remained at 12.5% before, during and after the crash. The present American state and the federal tax rate are the highest in the world, and our situation is that corporations are fleeing abroad to escape it. The corporate tax refugees in Ireland have so far generally remained in Ireland, probably because it is disruptive to move and the people speak English.
Judging by the Irish experience, America could similarly expect the fundamentals might change more slowly than might be guessed, but probably more quickly than they did in Ireland. The net effect on government revenues would be negligible, but the effect on employment would be strikingly positive. With higher employment, wages would rise. Somebody would lose, but it wouldn't be America; a deft new President might even be able to deploy some new power abroad, peacefully but firmly.
The current President might have to ride a bucking broncho for a few weeks. So in summary, most of the economic turmoil to be feared would likely be short-term and in the financial markets. I can easily imagine the skepticism with which the affected employees would greet this analysis and all the op-ed columns in the usual newspapers. Balanced against that, American medical care would at least get a lot of distortion wrung out of its accounting processes, and surely would be improved in the long run, by regaining control of its own finances.
Let's return to the details. It is sometimes argued the gift of insurance premiums is an addition to the salary, but almost all economists agree the salary soon re-adjusts up or down, to reappear in the pay packet. Stop calling it wages and treat it as total wage costs, and you soon see the point. No doubt it takes time to adjust, and it seems fair to say the employer benefits from corporate tax reduction more quickly than the individual employee does. The tax amount comes close to $2000 per year per employee. Because the hidden benefit lies in taxes, the profitability of the company enters in as well, and what is true of one employer may not be as true of another. In particular, it is not true of the government and non-profit sectors, who have no corporate income taxes to pay. There may be some political hope in that.
If a business is profitable to the full limit of corporate taxes, the nominal benefit is the full limit of the employee's tax bracket, but the offset to the employer can be about twice that rate in corporate taxes. Here, we assume a blended income tax rate of 20% for the employee and 39% top state and federal rates for the employer. In companies with 10,000 employees, financial saving alone can be considerable. Almost all corporations listed on an exchange are profitable most of the time; there might be more swing in smaller businesses.
Anyway, sometimes it just seems more attractive for small businesses to have Subchapter S tax treatment. On that subject, it is a little difficult to say what pressures motivate small family businesses. Some people allege the whole Subchapter S complexity is a reaction to utilizing this distinction and therefore should be counted as an indirect benefit of the Henry Kaiser gambit. During the 2009 Tea Party agitations however, it was noticeable that small businessmen at the microphone were extremely vocal in their opposition to Obamacare. Unfortunately, it is hard to know how well small business understands the inside operations of big businesses. As they say, Macy's doesn't tell Gimbels.
With regard to all employees as a class, it seems safe to say, people who are well enough to be employed, have mostly lower healthcare costs, and therefore seem more attractive in the eyes of their health insurance company. That would maybe result in lower premiums. Since only 25% of persons aged 25-34 are insured, Obamacare calculated they would break even if they enrolled 40% of the "young invincibles" at average rates. Generally speaking, that would be males, who -- without the Henry Kaiser gimmick -- might have an 80% avoidance rate. But remember, there's also the automobile insurance phenomenon: compulsory auto insurance induces a great many to stop paying premiums after the first month or two.
With Obamacare, the dropout rate is reported to be 13% during the first year of operation. The kids resent being overcharged for something they feel they don't need and calling them "young invincibles" inflames rather than softens that feeling. The much more important point is they don't get anything back when they are older , except sympathy. That's the central flaw in employer-based one-year term insurance, and let's hope you notice the Health Savings Account corrects the injustice. With auto accidents, young people have higher rates, and that's accepted as normal. With health insurance following the same logic, it ought to be the other way around, shouldn't it?
Taken all together, it is pretty easy to see why big business demanded a one-year exempted delay from Obamacare, which later was extended another year. No doubt they intend to keep a low profile but will keep demanding "temporary" exemptions, at least until the recession is over, and possibly forever. Until we see the eventual experience with employees, the largest group affected, it will be impossible to predict the limits of the subsidy program for the uninsured. Nevertheless, it is fairly obvious this essentially political impasse is being treated as an untouchable issue, and believable estimations of "fairness" will be a long time in coming. Businesses of all sizes like to present themselves as a big happy family. But in fact, the large common market produced by our continental boundaries means a comparatively small amount of American trade (but admittedly a growing one) is international. The main competition for big American business is small American business, and don't you forget it.
To a fairly large extent, this split is also a split between family-controlled business and stockholder-controlled business, between Subchapter S and Subchapter C corporations, and between university-educated management and small-college educated bosses. It's geographic, it's regional; it's R and it's D. If you ever watched a pro football game with businessmen in the audience, you know both large ones and small ones always feel challenged, and both intend to win, even when they might both end up losing.
Solutions: Nevertheless, the issue of revenue neutrality, at least for employer-based health insurance, is easily summarized. You don't have to be a professional negotiator to see that something close to a 2/3 exemption for everybody could make it revenue neutral. And then, through inflation and other traditional means of attrition, mid-course corrections might whittle it down.
But that's only part of it. Remember, the employee payroll deduction is only half of the issue. The employer gets the other half, by paying lower corporate taxes. His total payroll cost ends up much the same, but by this time the reader should see that doesn't matter. Corporate taxes are too high, probably in part because of class antagonisms. We have a flight of corporations abroad, and we see the Irish example that you shouldn't go too fast. But a reassuring part of this problem is we have Congress to negotiate it. Having learned how to raise food stamps by raising farm subsidies, they don't need any lessons in triangulation. No need to mention volume discounts on the insurance premiums, and discounts the insurance company shifts to the hospital. The details of such features are not public information.
Taken altogether, it sometimes appears equal treatment might be easier to attain than the elimination of the tax exemption. If everyone received a tax exemption, at least in part, we might at least eliminate the distortions imposed by rent-seeking the loopholes. It might raise healthcare prices at a time we need to lower them, so a stepwise approach might turn out to be the only feasible one. This is a time when healthcare is so expensive that only a really radical approach might be noticeable. Perhaps it is time just to get rid of the inequality, so later sacrifices for the economy will not seem so hypocritical.
There's one other misconception to be wary of. A tax reduction at the 50% employer rate is not at all the same as a 50% reduction of the employer's taxes, although it may sound like it. It's likely to be far smaller.
Public Misconceptions
(Healthcare for Citizen Lobbyists)
There are a few other ideas about the cost of medical care, which I would say are widely held, but the truth of which seems dubious. In fact, I would characterize them as misconceptions. If misconceptions are held long enough, they eventually work their way into the tax code.
Is Preventive Medicine Always and Everywhere Less Expensive? As heads nod vigorously in support of prevention, please notice in general usage it suggests several different things. The overall implication is that small interventions for everyone are less expensive to society; less expensive, that is than large expenses for the few who get the disease. That is clearly not invariably the case, and unfortunately, in a compulsory insurance world, it may seldom be the case. The point is not that preventive care is a bad thing, because it is often a very good thing, even by far the very best thing. It's just not necessarily cheaper.
Take for example a tetanus toxoid booster, which ten years ago cost less than a dollar for the material. Recently in preparation for a vacation trip, I was charged $85 dollars by my corner drugstore, just for the material. If you do the math, $85.00 times millions of Americans is a far greater sum than the present aggregate cost of Americans actually contracting tetanus, especially following the advice to have a booster shot every ten years. This becomes more certain if one adds in the cost of administration. The vaccine is quite effective, Americans had almost no cases in the Far Eastern Theater in World War II. The British who did not vaccinate routinely had large numbers of often fatal cases. Furthermore, even if the tetanus patient survives, the disease is hideously painful. Is it better to immunize routinely? Yes, it is. Is it cheaper? I'm not entirely sure, because I have no access to the production costs of tetanus toxoid. But it certainly seems likely it isn't cheaper. Malpractice costs, which are a different issue entirely, complicate this opinion.
 Better, yes. Cheaper? No. 
|
| Preventive Medicine |
Something, probably malpractice liability, has transformed an effective preventive procedure from clearly cost-effective to -- probably not cheaper for a nation which no longer has horses on the streets, but still has horses on farms and ranches. This is presently mostly a malpractice liability problem for the vaccine maker, not a preventive care issue. Take another well-known example. In the case of smallpox vaccination, it is now clearly more expensive to vaccinate everyone in the world than to treat the few actual cases. The waffle currently being employed is to limit vaccination to countries where there are still a few cases, hoping thereby to eradicate the disease from the planet.
Over and over, an examination of individual vaccinations shows the answer to be: better, yes, cheaper, no; with the ultimate answer depending on accounting tricks in the calculation of cost, cost inflation because of third-party payment, and related perplexities. To be measured about it, excessive profitability of some preventive measures could act as a stimulant for finally calling off prevention, by taking on a briefly more expensive campaign to achieve final eradication. Somewhere in this issue is the whisper that "natural" gene diversity of any sort must never be totally eliminated, a viewpoint which even the diversity philosopher William James never openly extended to include virulent diseases.
Routine cervical Pap tests, routine annual physical examinations, routine colonoscopies and a host of other routines are in general open to questioning as to cost-effectiveness. The issue is likely to increase rather than go away. Much of the current denunciation of "Cadillac" health insurance plans focus on the elaborate prevention programs enjoyed by Wall Street executives, college professors, industrial unions, and other privileged health insurance classes. A more useful approach to a borderline issue might focus on removing such items from health insurance benefit packages, particularly those whose cost is subsidized, either directly or by income tax deductions. Those preventive measures which demonstrate cost-effectiveness can have their subsidy restored, or be grouped together into a category which must compete for eligible access to limited funds.
The inference is strong that unrestrained substitution of community prevention for patient treatment escalates costs rather considerably, and -- at the least -- needs to demonstrate more cost-effectiveness before subsidy is extended. While self-interest is a possibility if only physicians are consulted, total reliance on bean-counters could eliminate benevolent judgment entirely. Community cost effectiveness is a ratio, and both sides must be fairly argued. Don't forget many people quietly recognize the need for gigantic cost-shifting between age groups. Spending money on young workers to pay for shots is one way to shift the cost of elderly illness, backward to the employer they no longer work for. It can be a pretty expensive way to do it.
In the final analysis, without some form of patient participation in the cost, this issue is probably unsolvable. To launch a host of double-blind clinical trials to find out the truth will lead to answers of some sort, which will quickly be undermined by price/cost confusion, leading to increasingly futile regulation. Including preventive costs in the deductible at least allows public participation in the decisions and true balance to begin; which is to say, even universal preventive care admiration cannot be adequately assessed except in the presence of a substantial open market for the product.
Much "preventive" care is really "early detection" or "early management". That's entirely different. When the goal changes so subtly, it is often not possible to judge what is worthwhile, except by placing some price on pain and suffering. The abuse by the trial bar of the monetization of pain and suffering in the malpractice field, ought to be a gentle reminder of that. Preventive colonoscopy has clearly caused a decline in deaths from colon cancer; that's a medical judgment and a transitional one. Whether the cost of catching those cancers early was cost-effective is largely a matter of colonoscopy cost, and on digging into it, will be found to be as much an anesthesia issue as a colonoscopist one. In any event, it is not one where the opinion of insurance reviewers should be decisive. If the litigation industry moves to make an omission of prevention a new source of action, it will surely be a sign it is a past time, to caution the public about the direction of things.
 Average Hospital Profit Margins: Inpatient 2%, Accident Room 15%, Satellite Clinics 30% 
|
| Payment By Diagnosis |
Outpatient is Not Necessarily Cheaper Than Inpatient For the Same Problem. Medicare provides half of the hospital revenue; the other half is often dragged into a uniform approach. The reimbursement mostly has nothing to do with the itemized bills hospitals send and may have little to do with production costs. The DRG (Diagnosis-Related Groups) system for reimbursing hospitals for inpatients is thus not directly based on specific costs in the inpatient area. It is related to clustered diagnoses lumped into a DRG group, and then assumes overpayments will eventually balance underpayments within individual hospitals.
That last point, depending on the Law of Large Numbers, is questionable, and especially so in small hospitals. When two million diagnoses are condensed into 200 Diagnosis groups, group uniformity just has to be uneven. Reimbursement means repayment, but this interposed step often interferes with that definition. Someone in the past fifty years discovered the reimbursement step was an excellent choke point. Manipulating the reimbursement rates without changing the service is a handy place to choose winners and losers; it's largely out of sight of the people who would recognize it for what it is. Furthermore, for various DRG groups, or for all of them, it becomes possible to construct a fairly tight rationing system for inpatient costs.
The degree to which actual production costs match a particular DRG reimbursement rate is blurred by inevitable imprecision in the DRG code construction. It is impossible to squash a couple of million diagnoses into two hundred code numbers without imprecision. It works both ways, of course. The coders back at the hospital will seek weaknesses out, experimentally. A grossly generalized code is placed in the hands of hospital employees, resulting in a system which suits both sides of the transaction, but is one which ought to be abolished, on both sides, by computerizing the process. At least, computers could avoid the issue of mistranslating the doctors' English into code.
The overall outcome with Medicare is an average 2% profit margin on inpatients during a 2% national inflation. This is far too tight to expect it to come out precisely right for everybody. And in fact, inflation has averaged 3% for a century but is 1.6% right now. The Federal Reserve Chairman desperately tries to raise it, but it just won't go up. If you don't think this is a serious issue, just reflect that our gold-less currency is supported by a 2% inflation target which the Federal Reserve is proving unable to maintain.
For technical reasons, the same forced loss is not true of outpatient and emergency services, which usually use Chargemaster values. Emergency services are said to approximate 15% profit margins, and outpatient services, 30%. It is therefore difficult to believe anyone would start anywhere but the profit margin, and work backward to managing the institution. In consequence, the buyer's intermediary has stolen the pricing process from the seller. Without the need to communicate one word, prices rise to the level of available payment and then stop there. But let's not be too specific in our suspicions. Some incentive to direct patients to the emergency and outpatient areas must develop, and is acted upon in the pricing. It just doesn't have to be so confusing and so high-handed.
Any assumption by the public that outpatient care is cheaper than inpatient hospital care is likely to be quite misleading. Short of driving the hospital out of business, revenue in this system is whatever the insurance intermediary chooses to make it. There was a time when the intermediary was Blue Cross, and behind them, big business. Nowadays, it is Medicare, but Obamacare probably aspires to the turf.
Let's test the reasoning by using different data. Because hospital inpatient care is reimbursed at roughly 106% of overall cost, while hospital outpatient care is reimbursed at roughly 150%, hospitals are impelled to favor outpatient care, no matter which type of care happens to have the cheapest production cost, the best medical outcomes, or enjoys the greatest comforts. Instead, the rates and ratios are ultimately determined by magazine articles and newspaper editorials. At some level within the government, a political system responds to what it thinks is public opinion, vox populi est vox Dei. No matter what their personal feelings may be, hospital management encounters more quarrelsomeness on wages in the inpatient area, less resistance in the outpatient and home care programs. So, true costs must actually rise in the outpatient area, sooner or later, following the financial incentives. Personnel shortages follow, as does friction between hospitals and office-based physicians. The process is circular, but the origin of favoring outpatient care over inpatient care was primarily driven by some accountant reading a magazine article.
A highly similar attitude underlies the hubbub for salaried physicians rather than fee-for-service. It's a short-cut to a forty-hour week, and following that, to a doctor shortage. And following that, to enlarged medical school budgets. If anyone imagines that will save money, the reasoning is obscure.
Everybody can guess what it costs to wash a couple of sheets and buy a couple of TV dinners. Everyone fundamentally understands Society's need to transfer medical costs from the sick population to the well population. Nothing known about hotel prices justifies a 50% difference in price between inpatient and outpatient care, all else being equal. The room price mainly supports overhead costs which are unrelated to direct patient care, so those fixed costs are like migratory birds, settling to roost where it's quiet. Remember, it doesn't cost driving the system, it is now profit margins.
The Return of a Discharged Hospital Patient Within 30 Days is not Necessarily a Sign of Bad Care. Rather, it reflects the fact that hospital inpatient reimbursement is entirely based on the bulk number of admissions, not the sum of itemized ingredients. Having undermined fee for service, Medicare must resort to taxing the whole admission.
Early re-admission can, of course, be a sign of premature discharge or careless coordination with the home physician. But these issues are so remote from the basic reason for admission, that bulk punishment is unlikely to change the criticized behavior. That behavior may mean a convalescent center is convenient to a hospital, making it reasonable to move the patient without much loss of continuity of care; and treating his return to the acute facility becomes a matter of small consequence. It is also a matter of cost accounting; when you claim a hundred dollar hotel cost to be worth thousands of dollars, many distortions are inevitable. If a hospital essentially shuts down on weekends, for example, there actually might be better care available somewhere else.
Imposing a penalty for returns to the hospital post-discharge has certainly changed behavior, but it is far from clear whether institutions are better as a result. Without a detailed study of longitudinal effects and costs, this threat is no more than an untested experiment. Without access to accounting practices, doctors assume the penalty for a high re-admission rate merely affirms that hospital insurance reimbursement by DRG is solely dependent on the discharge diagnosis, therefore bears little relation to the quality of care. Given a particular diagnosis, reimbursement is totally independent of any other cost. When all you have is a hammer, everything looks like a nail to the DRG.
The legitimate reasons for re-admission to the hospital are many and varied. Collectively, they could well constitute a general attitude on the part of a particular hospital that it is reasonable to send many patients home a little early in order to achieve greater overall cost savings -- in spite of sustaining a few re-admissions. But this is somewhat beside the point. The insurance companies accept the fallacy that favoring readmission is the only way a hospital can increase reimbursement under a DRG system. This is merely a debater's trick of redefining the issue, from true cost to reimbursement amount. More or fewer tests, longer or shorter stays have no effect, but readmission can double reimbursement. Consequently, re-admission has been stigmatized as invariably signifying careless treatment, justifying a penalty reduction of overall reimbursement. This is high-handed, indeed. It would require a research project to determine which of the alleged motives is actually operational.
The Doughnut Hole: Deductibles versus Copayments. To understand why the doughnut hole is a good idea, you have to understand why copay is a flawed idea. In both cases, the purpose is to make the patient responsible for some of the cost in order to restrain abuse. As the expression goes, you want the patient to have some skin in the game. The question is how to do it; the doughnut has not been widely tried, but the copayment approach is very familiar: charge the patient 20% of the cost, in cash.
This co-pay idea finds great favor with management and labor in negotiations because the premium savings are immediately known. If the copayment is 10%, then employer cost will be decreased by 10%; if it is 50%, the cost is reduced by 50%. In midnight bargaining sessions, such simplicity is much appreciated. However, the doughnut hole was not devised to make negotiations simpler for group insurance, it was devised to inhibit reckless spending, theoretically unleashed once the initial deductible has been satisfied.
Health insurance companies also like both co-pay and doughnuts for questionable reasons. Both offer an opportunity to sell two insurance policies as two pieces of the same patient encounter, adding up to 100% coverage, but eliminating the patient's skin in the game. Doubling the marketing and administrative fees seems like an advantage only to an insurance intermediary, while it totally undermines the incentive of restraining patient overuse. In practice, having two insurances for every charge has led to mysterious delays in payment of the second one, even though they are often administered by the same company. Physicians and other providers hate the system, not only because it involves two insurance claims processes per claim, but because it often makes it impossible to calculate the residual after insurance, i.e., patient cash responsibility, until months after the service has been rendered. Patients often take this long silence to imply payment in full, and disputes with the provider are common. Long ago, older physicians warned the younger ones, "Always collect your fees while the tears are hot."
It has long been a mystery why hospital bills take so long to go through the system; at one time, protracting the interest float seemed a plausible motive. However, the persistence of delayed processing during a period of near-zero interest rates makes this motive unlikely. It now occurs to me that the reimbursement of health insurance costs by the business employer is related to corporate tax payments, and hence to the quarterly tax system. Using the puzzling model of a monthly bank statement for online reporting would have some logic, but great confusion, attached to the bank statement approach for group payment utility. But in the end, I really do not understand why health insurance reimbursement or even reporting to the patient, should take so many months, and cause so much difficulty. Recently, the major insurance companies have started to imitate banks by putting the monthly statement continuously online on the Internet. If doctors find a way to be notified, the billing cycle could be speeded up considerably, and even the deplorable custom of demanding cash in advance may abate. The intermediaries probably won't do it, so it is a business opportunity for some software company, and a minor convenience for the group billing clerk.
So, the idea of a doughnut hole was born, after empirical observation about what was owed on two levels, one for small common claims, and another for big ones. Formerly, the patient either paid cash in full or was insured in full, so arriving at the Paradise of full coverage is purchased in cash within the first deductible. Unfortunately, once that last threshold was crossed, the sky became the limit. Some way really had to be found to distinguish between extravagant over-use, and the use of highly expensive drugs, particularly those still under patent protection. The idea was generated that if the two levels of the doughnut hole were calculated from actual claims data, there might often be a clear separation of minor illnesses from major ones. Since the patient would ordinarily be uncertain how far he was from triggering the doughnut hole, the restraint of abuse might carry over, even into areas where the facts were not as feared.
It is too early to judge the relative effectiveness of the two different patient-responsibility approaches, but it is not too early to watch politicians pander to confusion caused by an innovative but unfamiliar approach, while the insurance administrators simplify their own task by applying a general rule, instead of tailoring it to the service or drug. And by the way, the patients who complain so bitterly about a novel insurance innovation, are deprived by the donut hole of a way to maintain "first-dollar" coverage, which is a major cause of the cost inflations they also complain so much about. Some people think they can fix any problem just by loudly complaining about it. Perhaps, in a politicized situation, it works; but it doesn't fool anyone.
Plan Design. The insurance industry, particularly the actuaries working in that area, have long and sophisticated experience with the considerations leading to upper and lower limits, exclusions and exceptions. Legislative committees would be wise to solicit advice on these matters, which ordinarily have little political content. However, the advisers from the insurance world have an eye to bidding on later contracts to advise and administer these plans. They are not immune to the temptation to advise the inclusion of provisions which invisibly slant the contract toward a particular bidder, and failing that, they look for ways to make things easier, or more profitable, for whichever insurance company does get the contract. The doughnut hole is a recent example of these incentives in action; no member of any congressional committee was able to explain the doughnut for a television audience, so it was ridiculed. The outcome has been a race between politicians to see who could most quickly figure out a way to reduce the size of the hole. The idea that the size of the hole was intended to be an automatic adjustment to experience, seems to have been totally lost in the shuffle. Asking industry experts for advice is fine, but it would be well to ask for such advice from several other sources, too.
Fee-for-Service Billing. In recent years, a number of my colleagues have taken up the idea that fee-for-service billing is a bad thing, possibly the root of all evil. Just about everyone who says this, is himself working for a salary; and I suspect it is a pre-fabricated argument to justify that method of payment. The obvious retort is that if you do more work, you ought to be paid more. The pre-fabricated Q and A goes on to reply, this is how doctors "game" the system, by embroidering a little. I suppose that is occasionally the case, but the conversation seems so stereotyped, I take it to be a soft-spoken way of accusing me of being a crook, so I usually explode with some ill-considered counter-attack. My basic position is that the patient has considerable responsibility to act protectively on his own behalf. That is unfortunately often undermined by excessive or poorly-designed health insurance. Nobody washes a rental car, because that's considered to be the responsibility of the car rental agency. A more serious flaw in the argument that we should eliminate the fee for service, was taught me in Canada.
When Canada adopted socialized medicine, I was asked to go there by my medical society, to see what it was all about. That put me in conversation with a number of Canadian hospital administrators, and the conversation skipped around among common topics. Since I was interested in cost-accounting as the source of much of our problems, I asked how they managed. Well, as soon as paying for hospital care became a provincial responsibility, they stopped preparing itemized bills. Consequently, it immediately became impossible to tell how much anything cost. The administrator knew what he bought, and he paid the bills for the hospital. But how much was spent on gall bladder surgery or obstetrics, he wouldn't be in a position to know.
So I took up the same subject with the Canadian doctors, who reported the same problem in a different form. Given a choice of surgical treatment or a medical one for the same condition, they simply did not know which one was cheaper. After a while, the hospital charges were abandoned as a method of telling what costs more, and eventually, no effort was made to determine comparative prices at all. There's no sense in an American getting smug about this, because manipulation of the DRG soon divorced hospital billing charges from having any relation to underlying costs, and American doctors soon gave up any effort to use billing as a guide to treatment choices. We organize task forces to generate "typical" bills from time to time, but these standardized cost analyses are a crude and expensive substitute for the immediacy of a particular patient's bill.
My friends in the Legal Profession make a sort of similar complaint. The advent of cheap computers created the concept of "billable hours", in which some fictional average price is fixed to a two-minute phone consultation. In the old days, my friends tell me, they always would have a conference with the client, just before sending a bill. The client was asked how much he thought the services were worth to him, and often the figure was higher than the actual bill. In the cases where the conjectured price was lower, the attorney had an opportunity to explain the cleverness of his maneuvers, or the time-consuming effort required to develop the evidence. A senior attorney told me that never in his life did he send a bill for more than the client agreed to pay, and he was a happier man for it. Naturally, the bills were higher when the attorney won the case than when he lost it, which is definitely not the case when a hospital is unsuccessful in a cancer cure. Similarly, you might think bills would be higher if the patient lived than if he died, but income maximization always takes the higher choice. So the absence of this face-to-face discussion is a regrettable one in medical care, as well.
Hospital Cost-Shifting by Age Group, Patient Income, and Payer Class
When kids get sick, the parents pay the costs. When the grandparents get sick, Medicare may well pay a large part out of tax withholdings, premiums, and government borrowing, but working children still are the last resort for the grandparent generation, if resources fail. What's the common theme, here?
All medical costs, whatever the age of the patient, ultimately rest on the contributions of some working person, aged 21 to 66. The medical payment system is largely driven toward transferring funds from non-sick people to sickly non-working ones. The non-sick increasingly resent this stubborn fact, but as long as we continue an employer-based system it will only get worse. It is necessarily a dangerous hostility to encourage.
Indeed, our whole society is somewhat based on the interdependent family unit, using the assumption breadwinners pay for themselves and children, and are ultimately responsible for their parents as well. It's somewhat dismaying to reflect, that with a decline in the power of religion, a decline of the importance of the family may threaten the stability of many under-examined issues, just like healthcare financing. If the employer or the government supersede the family, the family is still the fall-back; and anyway, all taxes and profits ultimately derive from working people, just not the family's own, particular, working people.
Whole generations vocalize decreased respect for marriage in various ways, but do not seem to have considered the disruption it would cause, to get taken at their word. Viewed both ways, if we discuss the ability to pay for healthcare, we have to admit there is nobody to stand behind those bills, whatever the age of the patient -- except some breadwinner. Then, when we ask whether the country can support the cost of healthcare, we are actually questioning whether a solitary age generation of workers can really afford to pay the current costs of everyone else. Must demographics somehow be twisted to suffice, or can we tweak the system? Can we all live ninety years, and only work for thirty of them?
The Demographic Distribution of Health Costs. Unfortunately, health costs do not self-distribute to match health revenues without some pushing. Mostly, the process is, revenues are twisted to match costs.
About 3% of health costs concentrate in the first year of life, about 15% of costs are generated in the last year of life. The last year of life itself has shifted, from age 47 in 1900 to 83, today. Given some time, longevity will grow to 93. From these facts alone we see a minimum of 18% of costs being redistributed from workers to non-workers, and inter-generational cost shifts as a whole are probably closer to 68%. That's variable and inaccurate because hospitals know you have to be born and you have to die, so they find ways to pay bills, shifting the cost of what isn't mandatory, onto the bills of those who cannot escape. That, in turn, is shifted a second time, to the people who can better afford to pay them. It seems to the business office like money going in and out of the accounting office door, but in fact, it goes in one door and goes out through quite a different door.
 Mostly, revenues are twisted to match costs. 
|
| Hospital Cost Shifting |
It just has to be that way; no other way will work. It isn't rocketing science to figure out, it actually doesn't cost thousands of dollars to deliver a baby, or to pronounce an old fellow dead. Just compare the price of a five-star hotel with the price of (one half of) a semiprivate hospital room or the cost of a frozen food dinner with a hospital meal. This isn't cheating; it's just an institution trying to serve the community.
Indirect Overhead. One of the generalizations which is made fairly, however, is a typical hospital ends up with too much indirect overhead. Somebody has to be paid to mow the lawn, but you can't very well bill patients individually for lawn-cutting. Somebody must answer the telephone for the institution. Over the past centuries, a lot of activity was dumped on the hospital, because hospitals are nice, they are handy, and everybody shares a piece. They are a favorite place to hold local elections on the second Tuesday in November, for example, because they generally have some spare space in the lobby, and they belong to everybody in the community. They have cafeterias and gift shops because that is part of their function. As long as they have them, why can't the community use them? They also have parking garages, partly with the same motive banks use, to issue mortgages for buildings which could be sold for some other use in a pinch. And mortgages are cheap, right now. The point is not they are building things they don't really need, the point is an accumulation of such costs provides a handy vehicle for -- large indirect overhead charges on the cost report. Every overhead cost must eventually be added to some bill, and can thus -- why not-- be re-assigned to areas of the hospital which normally house patients of a target group.
There once was a time when indirect costs avoided elderly patients; as soon as Medicare became an entitlement, the incentives shifted. Now, serious expensive diseases are all migrating into the Medicare age group. As they do with computerized cost-shifting of pediatric units, and as they will when Obamacare pays for some indigents. But please don't pass regulations to suppress the salaries of cost accountants, in order to control all this abuse you have suddenly discovered.
When 100% of the costs must be supported by 20% of the patients, no hospital in existence could stay in business for a week, without cost-shifting. No doubt, most hospital administrators would welcome insurance companies doing this cost-shifting on their own books, but they would be foolish to permit it. Sooner or later, some community activist would protest it was dishonest, and the insurance companies would promptly dump it back in the hospitals' laps. In a sense, hospitals are reinsurers of last resort and must remain reluctant to give away the tools of their trade.
Diagnosis Related Groups (DRG), in Relation to Medical Electronic Records.

|
| The American Medical Association |
For a concept supposedly working moderately well, the Diagnosis Related Groups (DRG) system for inpatient reimbursement has a bizarre history. It has led to some unconfessed, and widely unrecognized, disastrous results, and should be thoroughly reworked as soon as possible. In a scholarly sense, the story begins eighty years ago. The American Medical Association decided all of the diseases, ultimately all of the medical care would be better understood if reduced to a systematized code. Originally, the code was visualized as a six-digit complex, with the first three digits defining an anatomical location, followed by a second set of three digits specifying the cause of the disease affecting that location.
SNODO That 6-digit structure limited code to a thousand diseases in a thousand locations, or a million "disorders" just for a beginning. Roughly half those theoretical combinations have no biologic existence, although even fanciful codes had some value for detecting coding errors. Other regions of the code exceeded the number of conditions actually found to exist, but originating in a digital structure then allowed virtually unlimited expansion, but sacrificed the significance of a particular position within the code. IBM was enlisted as a consultant, who advised the AMA to stop worrying about it; just provide a numerical code for everything, in the finest detail possible. Mathematicians could later easily make it usable for calculating machines, the forerunners of computers; and non-existent conditions created no harm. Some of those consultants had worked with a system which produced great success for the U.S. Census and perceived no advantage to limiting the code numbers while planning for them to be manipulated by machines. The third group of three digits was soon added, making a nine-digit Standard Nomenclature of Diseases and Operations , familiarly known as SNODO, which could identify a million different operations, whether actually performed or not. Actually, groups of three or more digits separated into groups of three digits by hyphens transferred the significance of code-position to the cluster level, which proved adequate.
SNOMED The pathology profession subsequently added still the fourth set of digits, for microscopic features, so the potential was soon up to a hundred million microscopic conditions. The team of physicians who worked on coding the medical universe contains many names now famous, notably including Robert F. Loeb and Dana Atchley of The College of Physicians and Surgeons of Columbia University. For at least thirty years, the Joint Commission on the Accreditation of Hospitals (an AMA and AHA joint affiliate) enforced a rule: every discharge summary from every accredited hospital in America must code and index every discharge diagnosis in SNODO code. It was tedious work, kept alive by the glittering future prospect of developing an Electronic Medical Record by 1940.
|
| Robert F. Loeb |
ICDA After twenty years or so of this enormous task, the Medical Records Librarians rebelled. The labor effort was burdensome, and the librarians were in an occupational position to observe how little use was being made of it. On their demand, an alternative simpler coding system was adopted, called the International Classification of Diseases (ICDA). At first, it was limited to the one thousand commonest discharge diagnoses , therefore limited to the charts which the librarians could confidently observe would be used. In time, it was expanded to ten thousand commonest diagnoses. Limiting medical codes also limited the cost and effort of coding and was considered an important retreat from over-enthusiasm. Meanwhile, expansion of the SNODO code by a handful of true believers continued to fill up the coding gaps, soon using and exceeding the capacity of the 80-column IBM punch card (originally, ten digits plus metadata), one card per diagnosis.
Unfortunately, the code was in danger of collapsing from this unanticipated expansion, since computers had not yet advanced to the point where they could rescue SNODO from the limitations apparent to its users. It was a classic case of a hypothetical system appearing to be better than the one in actual use, but not living up to its promise when both systems encountered actual use. The ICDA coding scheme did suffice for immediate purposes, and the "calculator" system was at least a decade away from evolving into the more flexible "computer" which could skip around the limitations of a punched card input system.
The professional difference was this: the doctors roughly understood the coding logic and could devise an understandable code for most charts through the logic of a structured language. The record librarians had not been trained to encipher (or even dither, as photographers say) the code by logic; a thousand codes was about the limit of what anyone could memorize. The burden of manual coding eventually overran the code design, before practical results could defend its utility in other areas of the hospital or the profession.
All the medical record world promptly abandoned SNODO; except for the pathologists who intuitively recognized ICDA could never approach their own greatly expanded needs. Eventually, pathologists took SDODO over, expanded and redesigned the basic framework, and produced what they are rightly proud of, an elegant codebook called SNOmed which obeyed meaningful internal coding rules. It still came, however, as a large and expensive book, which most practitioners were reluctant either to buy or to use.
|
| Dana Atchley |
DRG Meanwhile, a group at the School of Hospital Administration at Yale under the leadership of John Thompson lurched in the opposite direction of drastically reducing the ICDA code (initially expanded to 10,000 entries, which proved too large for some purposes, while still lacking specificity in many others), back down to only 468 of the commonest "diagnosis clusters". The purpose was to find clusters of diagnoses with common characteristics, which could be used by unskilled employees to identify diagnosis submissions which normally fell within certain bounds, but who in a particular case were sufficiently deviant to warrant investigation as "outsiders". This gross sorting by machine was then examined by the PSRO (Professional Standards Review Organizations), especially in the central feature of the length of stay. They termed their product Diagnosis-Related Groups (DRG) , which made no pretense of being complete but was complete enough to encompass the majority of outrider events. The computer version of their concept was called Autograph, which had some attraction to hospital administrations as a way to predict outriders. To summarize what happened next when Medicare adopted DRG for payment purposes: both DRG and ICDA started to expand, and SNOMED was relegated to the role of the codebook for Neanderthal pathologists.
 Two million diagnoses are compressed into two hundred payment groups. 
|
| Diagnosis "Related" Groups |
Using the standard diagnosis codes, one-size-fits-all did not help the hospital and insurance accountants a bit, since my habit they tend to believe all businesses are about the same, no matter what the business produces. Their complaint was coded with thousands of codes were too big and complicated. Simultaneously the medical professionals were finding them much too small for the job. Meanwhile, ICDA was fast losing its reputation for being compact and inexpensive, while the opposite feeling immediately developed: the DRG was far too small for what physicians could now realize was going to play a very large and important role in everybody's finances. Two vital areas of the hospital had difficulty communicating from the beginning; now, there was no longer even a common language to use. There was no quick fix, either, because both DRG and the underlying ICDA designs were based on the frequency of occurrence, rather than precision and logic. Furthermore, the copyright was owned by professional societies who had little interest in finances, and considerable interest in reducing their burdensome coding workload. In the background, however, computers had made the task of code translation a trivial one. A third profession, the computer department, scarcely knew what the other two were talking about, but they came closer to affinity with the accountants.
Like the three bears of Goldilocks, some codes were too large and some were too small, but at least there were three of them, each crippled in a different way. Comparatively few doctors understood what was going on, and in spite of their vital interest at stake, had trouble getting over their hatred of the boring coding task. Since this whole issue of data coding and summarization has taken on major importance to the success of the Affordable Care Act, in some circles the uproar has become a political war dance. Let Obama do it if he likes coding so much. Basically, the librarians were saying they resented being criticized for making important mistakes in a task they didn't understand very well. In summary, everybody hates coding.
Overview of the Future.One a faction of the small field of those who are interested in such matters has decided to expand both the specificity and the reach of ICDA, which is now up to its tenth edition of revision. Unfortunately, it does not seem to some of the pathologists to be a sensible approach. We have an elegant code in SNOMED, they protested, which is arguably too big to use; expanding ICDA seems destined to reach the same destination, on the rebound from being too small. We now have ample data on what is common. The most efficient approach would at first seem to be condensing the highly specific SNOMED to a useful size, based on the frequency of use. The approach would stand in contrast to making a list of diseases by frequency, and then subdividing their specificities. While such a condensed volume could be printed as a book, we are now at a point where every record room within the hospitals of the nation is equipped with several computers, so the elasticity of the code should no longer be anyone's problem. Let the machines do the drudgery.
This whole process could now rather easily be automated for much more than its original purpose of classifying disease populations, and in a pinch it could even substitute 26-digit letters for 10-digit numerals, imparting some clues in the process. Further condensation of an already condensed version began to be used for payment purposes, adding still greater amounts of practical nuance. You might suppose everyone could see paying the same amount of money for treating the same disease (tuberculosis, let's say) of two different organs (let's say of bone, and of the kidney) was either going to bankrupt someone or enrich someone else. And that's only money. Any scientific or diagnostic decision based on a code of "All other" will make computerized medical records sprint faster toward worthlessness. At the rate it's going, lumps of "all other" will have no relation to each other, except to justify the same reimbursement for treatments of vastly different value. Or difficulty. Or cost. Or contagiousness.
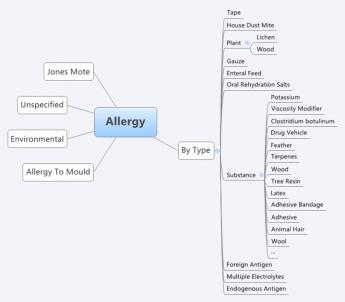
|
| SNOMED |
In automated form, SNOMED is quite ready to be revised still further in other directions for other purposes. It could, for once, integrate the accounting and demographic functions with the rest of medical care. But a great many other useful functions can be imagined, once computers have a stable platform on which to build, and the task of coding can be safely undertaken without much physician input burden. Safe, that is, from the danger, the whole coding framework will get changed, again and again. In a certain sense, this is similar to the brilliant choice by Apple of the Unix skeleton, when Microsoft Windows seized on quicker expedients. A great many sub-professions seem to wish to have their own codes for their own purposes and resist the idea a physician code should be imposed on them. When you encounter such obstructionism, it is easy to suspect motives. But the general rule is: when it comes to a choice between scheming and incompetence, it's incompetence, nine times out of ten.
However, medical care and hospital care are medical functions, and their accounting and demographics will always eventually return to their medical professional core. Meanwhile, notice what happened to DRG, a code so crude it relegates most refinements to the category of "All Other". The fact of the matter is, it is a crude approximation, some cases paying on the high side, some on the low side of true costs. If the hospital loses money on inpatients, well, just build another wing to the outpatient department. Underlying this response was the enduring misconception that outpatient care is inherently cheaper than inpatient. If it's the case, well, we'll just have to fix it.
The surprising lack of chaos from such experience has almost nothing to do with medical content, and almost everything to do with having insufficient case volume to remain in balance. That is, the big hospitals smudge it out, and the small hospitals don't understand it. The highly prized profit margin of 2% or 3% can easily be achieved by admitting slightly more cases of a profitable kind (ie hire a surgeon expert in certain profitable operations), or by the government adjusting just a few DRGs to profitable status (like reducing tariffs on behalf of favored industries in Congress). Meanwhile, the rest of the enterprise becomes progressively more expensive, because there is no fixed relationship between service benefit prices and audited costs, and now an even less regular relation, to cost-to-charge ratios.
It is a precarious thing for institutional solvency, to depend on a financial balancing of a particular caseload within one set of four walls, and then complain hospitals are too small to survive. Between their accountants and their record librarians, this outcome drives the smaller institution into a futile chase after higher patient volume. Of course, we need to change with the times. But some basic truths never change, and one of them is every ship should be able to sail on its own bottom. You don't approach that by giving every ship a new hull.
Let's get specific. In the first place, allowing only a 2% profit margin during a 3% national inflation is to walk on the edge of a dangerous cliff. If some fair profit margin could be agreed to, it is only an average among hospitals. You might as well reduce the DRG to four payment levels, and reimburse hospitals on the basis of which of the four walls the patient faces. With enough tinkering, you might arrive at the desired total hospital reimbursement to match any profit margin you establish, totally disregarding the diagnoses of all patients. Quite obviously, you must code the diagnosis to whatever number of digits it requires to identify the unique condition. You could match up all of the hundred dollar cases and all of the fifty thousand dollar cases, call the two codes, and pay only two prices.
But such an effort is just a delusion. Somebody-- or some machine-- has to go to the trouble of coding every single diagnosis down to the point where the code is no longer meaningful to costs and assign relative values among them. Only at that point would it be legitimate to assign a dollar amount to each relative value. You have to maintain the code as treatments change, which will be quite frequently. You can do it, and you can computerize it. A computerized version of this process would scarcely be any different from copying the English description and, like a Google search, getting back a number to copy; it might even be done by voice transcription. But there is still no guarantee charging itemized bills wouldn't turn out to be cheaper, and at least have a different meaning. DRG in its present form is nothing but a crude rationing system; get rid of it, or spend the money to make it work. I can't guarantee if you put a doctor in charge, it would work. But I can guarantee that if you don't put a doctor in charge, it won't.
Proposal 5: Congress should be asked to commission a computer program to translate English language diagnoses into SNOMED code, preferably by voice translation. Suggested format: a search engine where English variants of discharge diagnoses are entered, and a SNOMED code number returned, along the general lines of entering common phrases into Google and receiving file location numbers in return, except it returns the SNOMED code. If the code is not found, the computer accepts a manual entry by a trained person. verified by an expert over the Internet to become officially entered into a master list which is periodically circulated as an update. The search program and its supplements should be produced on DVD disks to be used on hospital record room computers by other professional users. It should provide "hooks" so the Snomed codes and patient identification can be transferred electronically to related programs, such as payment codes and billing.
So that's how DRG got to be what it is. It's perfectly astounding such a crudity, devised for other purposes, could be so "successfully" employed to pay for billions of dollars of Medicare inpatient care, such that payment by diagnosis-lumps threatens to spread to all medical care. There is even another way to describe it: inpatient hospital care has been lumped into a rationing system which constrains national inpatient care to a 2% overall average profit margin. That's just as surely true as if someone deliberately tried to make it that way.Payment by diagnosis ignores both cost and content, based on the mistaken assumption those features have already been carefully accounted for. It does not matter in the slightest how long the patient stays or how many tests he gets, or how many expensive big hospitals swallow up inexpensive little ones. Meanwhile, emergency rooms and satellite clinics also do not affect the cost inherent in a supposed linkage between the diagnosis and the cost. The failure to link drug prices into this modified market system is particularly noticeable.
The exciting potential has been lost to have the patients who can shop frugally as outpatients, set the price for inpatients who are helpless to act frugally. Their much more generous profit margins support what is essentially a hospital conglomerate. Any corporate conglomerate executive could tell you what happens when one department is subsidized, while another is treated as a cash cow. And the fun part is this: squeezing physician income against an unsustainable "Sustainable" Growth Rate creates the "doc fix", which annually blackmails physicians into acquiescence past the next November elections.
SGR: Sustainable growth rate, earmarks by a different name. SGR is a term borrowed from financial economics, signifying the rate at which a company is able to grow without borrowing more money. It is easily calculated by subtracting dividends from return on investment. Any variation from this definition will produce different results. A sustainable growth rate in Medicare is calculated by a formula, modified every year in special ways which closely resemble "earmarks", but contain special adjustments for changing work hour components, malpractice cost components, etc. It is a large task for the Physician Payment Commission to determine yearly changes in thousands of services, and it must be frustrating for them to see their painstaking calculations tossed aside every year by Congress, in response to howls from the various professions. Whenever this occurs it is a fair guess the calculation has been misused. The discussion has long since transformed from a simple calculation to a simple threat: physician reimbursement will be cut. Each year it is cut, and each year Congress relents on the cut at the last moment. But ultimately its design will prevail: on the pie-chart of healthcare expense, physician reimbursement will shrink, and hospital reimbursement will expand, as physicians migrate to salaried hospital employment, and enjoy an instant 40-hour week amidst a physician shortage. This keeps the AMA in a constant state of agitation, and physicians in a constant posture of supplication. At the end of 2013, the proposed cut in reimbursement had grown to 26%. When almost every physician has an overhead of 50%, a cut of 26% is beyond meaningful. And every year the financial attractiveness of joining a hospital clinic for a dependable salary grows, with consequent improvement in the overall power of the hospital conglomerate, and steadily decreasing relation to market-set pricing readjustments.
Insurance Reimbursement, The Missing Item on the Itemized Bill. The DRG system threatens patients, too. After discharge from a hospital, the patient is sent a multi-page itemized bill, which purports to be what the patient would owe without insurance. Such bills traditionally omit any mention of the insurance reimbursement, which is the only payment the hospital receives if it has contracted to accept "service benefits" as payment in full. Since that is almost always the case, the "total of service benefits" is exactly equal to the "total patient responsibility". Since the patient will pay nothing if patient responsibility is limited to service benefits, and service benefits are exactly equal to whatever the patient received, the explanation goes round and round without ever revealing what has been paid. The illusion that you have been told something worth hearing, is maintained by providing an almost endless list of itemized charges.
Most hospital employees do not have the foggiest idea why the list is even produced, and its accuracy is therefore questionable. A variety of specious explanations, therefore, emerge, usually with a focus on billing a handful of uninsured people, or insured people whose service benefits have expired as "outsiders". There may be a particle of truth to this, easily refuted by showing the supposed items on the bill were often fabricated by employees who know very well they are seldom used for anything. Most likely, the purpose is to conceal the true insurance reimbursement from competitive insurances who might undercut them. As profit margins shrink, it becomes increasingly dangerous to let competitors know what they are. As margins widen, it is even easier for competitors to undercut them. As a matter of common observation, most retailers in any business are less than forthright about their profit margins, so perhaps this concealment can be forgiven as normal commercial behavior. It becomes more questionable when seen as an industry-wide practice, intended to defend a system of double-pricing. In this case, it defends the employer tax discount as the lowest price around, when compared with those rascals, the uninsured or the insured but fully taxed.
The DRG payment to the hospital is not zero, but it is far less than the total on the itemized bill and is seldom revealed. One central message it sends is however pretty clear: "This is how much you would be charged if you didn't have Insurance X." The shortfall in revenue is made up by overcharging the emergency room and the outpatients, who are unsuitable for anything resembling the present DRG. If the hospital does not have enough outpatient work to sustain the inpatient losses, its only recourse at present is to call the architects and build a bigger outpatient department. To fill it, just buy up a neighboring group practice or two of neighborhood doctors. Fix the DRG, and it would be hard to say what would eventuate.
Bottom Line: Who is Injured? For a long time, service benefits insurance was the only thing supporting the hospital industry, and commercial behavior by the hospitals was justified as the only way to support their charitable mission. Now that Health Savings Accounts have reached 12 million clients, with assets reaching $22.8 billion, a viable way to provide indemnity insurance has definitely arrived. Not only are HSAs cheaper for the customer, they very likely provide higher payments to hospitals. This last point will only be clarified when we learn what discounts the catastrophic high-deductible insurance have been able to extract, but hardly anything else will affect the answer. To the extent one competitive method receives major discounts and the others generally do not, this service benefit discount is probably only of benefit to the insurance companies who enjoy it. A personal episode in my family illustrates.My son went to a well-known Boston hospital for outpatient colonoscopy and received a bill for $8000.00. When told that was outrageous, he protested and promptly received a bill reducing the charge to $1000. He was delighted to send a check for that reduced amount, even though I told him a fair price was probably around $300. He reminded me of a comment from a famous surgeon now deceased, whose name is emblazoned on a tall pavilion in another city. The old surgeon growled, "The only reason to carry health insurance is to keep the hospital from fleecing you." In a sense, that growl applied directly to the colonoscopy, which that hospital had converted from markup into a holdup.
Discounts for Health Savings Accounts? HSAs scarcely have to penetrate the market much further before they have the market power to command an equal discount. That may still take a little time, because some states have hardly any penetration, while California has a million subscribers. In the meantime, the patient needs to be careful to ask for prices in advance. Almost every health insurance has started to impose high deductibles, so their proper stance is to insist on equal treatment. The old system of "First-dollar coverage" was responsible for making outpatient care a target for this sort of thing. The next advance, after making all outpatient care match market prices, is to insist a hospital charge the same thing for the same service for inpatients as it does with outpatients. To make that possible, it has to return to fee-for-service billing, and management of Health Savings Accounts should settle for no less. That's the main reason DRG billing offends me, although there are lots of other reasons, and lots of other people are injured in different ways.
Hospital Cost-Shifting Reacts to the DRG
Medicare's payment-by-diagnosis system requires a diagnosis code for its computers to specify the payment. Codes are the way doctors can conduct their activities on a medical level while revealing to the billing department what the activity is worth. The billing department knows well enough these values will be later smudged and bloated, so why make work for yourself being accurate? Careful, fellows, your foot is on a slippery path.
High-handed Codes. The government could have chosen a coding system called SnoMed (Standard Nomenclature of Medicine), which specifies several million diagnoses in detail. Or it could have specified ICDA (International Classification of Diseases), which in its various iterations can identify several thousand. What it did choose was DRG, or Diagnosis-related Groups, specifying about two hundred. With various adjustments and offsets, this translates: there are only two hundred different price buttons to push -- for millions of diagnoses. The theory is, some cases will cost more, some will cost less, but in the long run, it all comes out just exactly right. Saves work for the billing clerks, that way.
Careful, fellows, you have stepped over the line of what is allowable latitude. Buried in your computer cubicles, hidden behind green eyeshades, you have convinced yourselves the world will tolerate anything you do for your own convenience. Try talking to one of them some time -- you will surely find the door is locked, or the boss is out to lunch, or it isn't company policy to allow accountants to talk to outsiders. If you have credentials, you may talk to a spokesman who seems to keep repeating himself. It does not seem to have occurred to anyone that the public wants to know if the charges are fair, and at the very least has a right to know if they are accurate. How can they be either fair or accurate, if millions of activities are reduced to two hundred price buttons?
 Pure and simple: A rationing system. 
|
| DRG |
I remember well, sitting in the Congressional hearing room when this proposal was first made. I giggled over Congress letting someone even utter such nonsense, let alone pass a law to go ahead with using it. But now I have to listen to reports this system has been in place for twenty years, and it works just wonderfully fine. A friend of mine was a graduate student at Yale, helping to develop the DRG system in its original form. He, too, is appalled that such an unexpected usage could even be considered, for what had an entirely different original purpose. The DRG was part of a coding system devised to assist the Professional Standards Review Organizations in monitoring insurance claims for errors and fraud. The behavior of each diagnosis group was studied for its general outline, and general patterns were identified. If a case fell outside the norms, it was tagged for investigation. Just how well DRG's worked out for that particular purpose, I have no idea. But to extend it for the actual payment of particular claims, simply boggled the mind, and still does.
Children Playing With Matches. When you let people do things like that, some pretty unexpected things happen. In the first place, using a system tailor-made for Medicare, you need at least one extra system to pay for patients who don't have Medicare. However, Medicare accounts for about half of average hospital revenue, so there is automatic pressure on everybody to conform to the system of the big cajun. An elaborate system called Chargemaster was devised for itemized services to be listed on an itemized bill, which now runs to dozens of pages for each patient. Since nobody much was going to use anything but DRG, the reasoning went that constant revision of thousands of itemized charges would be a big and useless task. Since you had to do it, you set the charges so high you wouldn't have to come back and revise them so often. Countless reporters have asked dozens of hospital administrators to explain the itemized bills which emerge, and almost every administrator admits he doesn't understand Chargemaster, and never looks at it.
Chargemaster. The billing clerks of the hospital look at it, however, and the patients look, and reporters look. Itemized bills totaling tens of thousands of dollars are sent, first to the patients, and then to the bill collectors. Stephen Brill's America's Bitter Pill is filled with "Tom and Mary of Tuscon" anecdotes, so let me add a couple of personal ones. For example, I received a bill for Seven thousand dollars from my own hospital accident room for twenty minutes treatment for a sprained wrist; the hospital clerk had joined in such a welcoming reunion for old times' sake, he forgot to collect my insurance numbers. After several strikingly threatening letters, communication eventually stopped. I have to assume they eventually found my insurance numbers on the record of an earlier admission. In another case, I discovered that another of my hospitals sends its bills when tests are ordered, not when they are performed. Consequently, a patient I discharged from the accident room without having the tests the interne had ordered, received an astonishing bill for the services, anyway. Since he was vice-president of the insurance company which covered him, there were some gratifying repercussions. On a later occasion, my oldest son received a bill for $8,500 for a colonoscopy from a famous Boston Hospital, and asked me what I thought was fair. I said it was worth a couple of hundred dollars, so he called his insurance company, following which the revised bill was one thousand dollars. He fell all over himself writing a check, for what I still say was a gross overcharge. Notice one theme running through all of these true stories. They all involved outpatient services.
You see, the hospitals were all shifting to a Chargemaster system for outpatients because the inpatient charges (often for the same services) were frozen by the DRG. In fact, it is widely quoted that inpatient profit margins were 2%, accident room profit margins were 15%, and the outpatient area made a profit of 30%. If anything approaching that is true, well, what would you do in their place? The next time you go past your local hospital, try to notice if a construction crane is working on a new building. The chances are excellent you will find it's a new outpatient building.
 If you put physicians on salaries, you get an instant forty-hour week. Soon, you get physician shortages. 
|
Hospitals are busy buying up physician practices because of the indirect effect of the DRG. Furthermore, the prices are high and the government is paying the bill through the hospital reimbursement system. My old friends smile, and a wink they will go back into practice if the hospital reimbursement declines. That long-term cost has to be factored in, although I doubt it will happen as they age. But if it does, the cost of reconciling a physician surplus might have to be included in the eventual reckoning of what the DRG did or did not save.
When you get down to it, the DRG is an excellent rationing tool, and rationing invariably creates shortages. Robert Morris learned that lesson the hard way during the Revolutionary War. He didn't speak much during the Constitutional Convention in 1789, but he was utterly determined that we not construct a command economy -- which is rationing on a grander scale. He kept his attention on his own business, while his protege Alexander Hamilton did the talking, and his best friend George Washington did the listening. How is the DRG a rationing tool? The government makes the rules, sets the prices, and monitors the outcome. However you choose to achieve a 2% inpatient profit margin, its economic effect is remorselessly judged as 2% revenue, operating within a 2% inflation rate, achieved by a 2% inflation target at the Federal Reserve. All the slack in the system has seemingly been driven into the out-patient and accident room areas. Except it hasn't. Everything the inpatient system asks for shall be given to it, on a 2% cost-plus basis. Profit margin, indeed. What we have is a cost-plus procurement system.
The Doc Fix
Unless a Congressman's name is attached to it by the media, it generally isn't easy to know who was the originator of a disagreeable law. In the case of Medicare, moreover, the program is technically an amendment to the Social Security Act, so revenue amendments must originate in the House of Representatives, Committee on Ways and Means, Subcommittee on Health. The difficulty is easily fixed by the Senate making an amendment to some unrelated House bill such as housing relief in Kansas. All subsequent amendments must jump through the same hoops because Congress is very strict about such traditions.
At any rate, some amendment was passed by both Houses to the effect that doctors' reimbursement would be held down if general Medicare costs had risen more than a certain amount. The theory was of course that doctors are in control of all medical costs, and therefore should be punished if they rose too high. The real purpose was to keep the doctors docile and quiet, since, at the last moment, each and every year, an exception to the punishment was made, just for one more year. This went on for eighteen years until Republicans finally achieved a majority in both Houses of Congress, and the law was promptly repealed in 2014. It was now possible to be pretty sure who had been behind the law all along. To reinforce this identification, the Senate Majority leader, Mitch McConnell (R, Ky.) executed a flashy last-minute parliamentary maneuver to rescue the repeal from its unidentified enemies, who had surely been of the other party. The "doc fix" was finally fixed.
In the course of this wrangle, it was revealed that physicians received 12% of Medicare expenditures. It reminded me, I had published a graph in The Hospital That Ate Chicago, showing that physicians received 20% in 1980. That would suggest their reimbursement had fallen by 8%, and perhaps that is true, corrected for inflation. However, reimbursements to other providers have risen, so the net change in physician reimbursement might be different from 8%. However, a related but different factor probably played an important part in this shift. Also during that period, a majority of physicians changed from solo private practice to working on a salary provided by a hospital group practice. The net effect was to shift the spokesmen for doctors' financial interests. It used to be the American Medical Association and now was to be hospital administration. In time, substance will follow form.
True, the primary cause of this shift was DRG pressure to shift revenue to the outpatient area, but since hospitals also participate in the Henry Kaiser tax dodge, this incentive was also at work, in a combined or concerted effect. The overall reimbursement effect was to shift physician overhead out of the costs, but not out of the reimbursement, which now goes to the hospital. Since almost every physician in practice spends 50% of his gross revenue on office overhead, there is plenty of room for shifts which do not appear on the balance sheet. Yes, physicians temporarily protected their net income by this maneuver, but the hospitals acquired an expense they did not necessarily intend to maintain. Squeeze the hospitals with DRG or other means, and politicians, as well as hospitals, had a piggy bank they could always return to, in a pinch.
The Doc fix has finally been repealed, possibly in part because it has served its several purposes. But tickling the victim for campaign contributions hasn't been repealed. This ancient parliamentary maneuver is unaffected. It will return, in other guises.
Reverse Bribery. Still another seemingly tangential issue is in the news, six months after control of Congress shifted parties. An ordinary layman would wonder if a 2.5% tax on medical devices is worth the acrimony its repeal seems to engender. But the ordinary layman is not familiar with bare-knuckle Chicago politics. When the Affordable Care Act was approaching legislative action, most of the affected groups were approached to sign up. Behind the enticements was an unspoken threat: if you don't come on board, you will be sorry. With only one notable exception (the medical device people), everyone signed on. And then the 2.5% special tax was laid on Medical devices. If you wonder why such small matters stir up so much bitterness, the history of the legislative preliminaries would seem of value to the search.
Amending Laws Rather than Rejecting Them
Division of power is one of the strengths of our system of governance. Isolating power to authorize spending, from power to spend, serves as an example. It's rather different, if one side seems to be winning all the battles; some fundamental power should possibly then be shifted. If the Founders believed God wound up the Universe clock and then let it run by itself, it seemed sensible to organize all government operations the same way. Entropy does not pick political favorites.
Very likely, the founders underestimated the time it would take for final balance to be struck between these two viewpoints, because it is nearly always the majority opinion which needs to be resisted. That's the unwritten assumption about what today is called Quaker Process, which occasionally irritates jumpy people. But nevertheless, in two hundred years, only slavery has seemed intractably unbalanced enough to warrant re-balancing by force. The Supreme Court-packing episode of 1937 came pretty close, ultimately shifting commerce regulation from states to federal. But it should have been done by amendment. Deleting the word "interstate" from the "interstate commerce" clause, must have seemed clever. That innovative way of amending the Constitution by one-word amendment has now lasted nearly a century, has never been exactly repeated, and surely would be reversed if the states could discover a way to regain their intended former power. Parsimony of words is admirable, but to have Courts amending the substance of a law is not in the province of either the Judicial or Executive branch. It takes some process the minority will agree to.
The Roberts Court seems to be continuing the "interstate" example of reversing policy by shifting the meaning of substantive words, as in "tax" and "penalty", when almost everyone agrees more orthodox amendment is more civil. Revising the meaning of "State exchanges" to include "Federal exchanges", clearly exceeds public tolerance for unorthodox approaches to language, however. If that's where they are going, the Court better slow down before their example is taken by lower courts, and ultimately by common practice. If you want to be treated like a leader, you must act like one. Our doctors in 1965, if not our lawmakers, had noticed Canada offering block grants to provinces who adopted the National Health system, which even Quebec felt forced to accept if they were going to be taxed for it, anyway. It seems particularly extortionate when applied to the Affordable Care Act. Our Supreme Court was primarily declaring, hinted extortion of this sort was unacceptable because of repeated Executive Branch examples of it.
 The Interstate Commerce Clause became the Commerce Clause, and Penalties became Taxes. 
|
| The Living Constitution |
That a majority of the Court was willing to reverse the meaning of language even after previously striking federal coercion in the same law, probably reflects the underlying opinion of one wavering Justice rather than the whole Court, while the Chief Justice struggled to maintain authorship of the decision. In the long view, elections rather than a few altered words may clarify the legal point. But an opportunity has been created for opportunists to move faster than the whole Court usually would.
In the case of King v. Burwell much the same thing as in the Court-packing episode happened, but in a law rather than the Constitution. Just as the word "Interstate" was deleted to read "Commerce Clause", while in the other, "State and Federal Exchanges" became "exchanges". The original language of the Act, about who can extend subsidies, was reversed to mean its opposite. This additionally has the subtle effect of endorsing the Legislative practice, demonstrated in this legislation, of placing deliberately opposite views into House and Senate versions, in order to conceal the real intention until the conference committee meets, the press is absent, and a holiday is near. In this case, it has the alternative appearance to the public that some members of the Court may have been better informed about the facts behind drafting the bill, than others.
A cloud of conflicting stories were printed after the decision, and it is hard to judge which one was truthful. My own preference is for the book by Jacob S. Hacker, The Road to Nowhere , written from interviews years earlier about the maneuvers of Hillary Clinton's allies for the Clinton Health Plan. Hacker now sounds particularly pertinent, since he was active in the Obama campaign, and because the reasoning of the majority about "ambiguity" sounds so strained. The suspicion of cover stories is regrettable. The public likes to believe the cloistered Supreme Court does not read the newspapers, as Mr. Dooley once put it, and only acts on testimony under oath in front of opposing counsel. That may be physically impossible, but the appearance is worth preserving.
Heath Insurance Companies Reach for the Brass Ring
In the light of future developments, we might someday look back on the University of Pittsburgh as the place health insurance stepped over a line and merged group practices with health insurance companies. It's true that was somewhat the way the first Blue Cross in Houston, Texas, had been organized, although it eventually split into component parts. It's the thought running through closed-panel insurance that this might be an easy way to circumvent antitrust laws because vertical integration is no longer considered a per se violation. Although, as mentioned earlier, it isn't necessarily a good thing either, and it isn't immune to a trial of the facts.
It has certainly aroused violent discomfort among excluded competitors in allied industries, to allow mediation control to fall into the hands of a corporation which could profit from the favoritism. Better to conduct arms-length transactions; the regulator should not profit from its own decisions. No law exactly says this should be so; the customers just like it better. And indeed Pittsburgh was the location of the defining court case, decades ago, where non-profit organizations were declared exempt from antitrust suits, just as Philadelphia had the first case which declared an end to charitable immunity. Until someone re-litigates these cases in a changing environment, these old court decisions retain a particularly large impact on local thinking.
Red tape is always expensive, and right now high costs are a challenging problem. Furthermore, big business is currently paying the bill, and big business would like to be satisfied on the point. That raises another historical point. Henry Kaiser gets credit for inventing the employer-based tax exemption, but the issue was rampant in all of the steel industry, which was often the leader in such innovations. The steel industry has pretty well abandoned America and gone to the Far East except for steel made out of scrap. The health insurance companies traditionally jumped at the command of the big employers, but maybe there is an opportunity for a revision of leadership in the industrial unions, particularly in steel. But while it may well be true this political vacuum has been filled with new leadership, it is likely some old traditions persist. The bitterness of the Molly Maguire era was thought to have ended a century ago, but if your ancestor was hanged or assassinated, the legend lives on. Sounds sort of like the Balkans, doesn't it? Some people in Bosnia are still endorsing genocide in retaliation for Thirteenth-century church burnings.
 Red tape is always expensive. 
|
Based on reasonings of this sort, it is fair to conclude that even if the big business (or big government) changes its mind about the ultimate outcome, this kind of behavior may or may not change. Uncertain of the eventual outcome, both providers and vendors of care may think it is better to leave the matter alone. And if someone else pays the bill, someone else may decide to change the system of utilization control. Through a convoluted history in several steps, the University of Pittsburgh has formed a large salaried group practice and merged it with the captive teaching hospital at one end, and the captive health insurance company at the other. Pennsylvania is a large state with rather wide sociological and industrial differences, but it is only natural that the other medical schools, hospitals, physician groups, and insurance companies would worry that this system might migrate into their neighboring territories. At the very least, rearrangements on such a large scale would be expensive and complicated. And not necessarily beneficial to the common good.
In case the reasoning isn't clear, let us restate the argument which was persuasive to the United States Supreme Court in the case of State Oil v. Kahn . As conglomerates acquire new businesses, they find they are not particularly good at managing a few parts of the whole. It is a failure in those defective components, which brings the whole conglomerate enterprise, down.
Companies may merge across traditional occupational boundaries, for a variety of reasons. One of the most questionable reasons to merge is to eliminate an unwelcome constraint on your plans, such as a new invention. Another would be to eliminate a critic whose views thwart you for reasons you do not understand. In the present situation, a medical school which supplies new physicians to a region should not be allowed to favor or control its graduates, or to enhance, protect or destroy their environment, particularly if the public suffers from the effects of it. When a medical conglomerate is allowed to profit in some of its divisions, in spite of losing money in others, the interests of the conglomerate may not be parallel with the interests of the public, in their choices of winners and losers. A mixture of taxable and non-taxable activities offer many opportunities for this to be the result.
Is It Better to Die in America?
The purpose of healthcare financing is to redistribute the pain of paying for it. Otherwise, the patient doesn't want to be sick or die; illness itself is a disincentive to abuse. The concern about abuse mainly arises when someone else pays for it. The indigent patient doesn't want to be sick, either, but somehow that's different. Not only does the public resent the cost, but the public also resents the need for the cost, as well.
Two of the central figures in devising Obamacare -- supposedly free healthcare for everyone -- have framed the issue as to whether it is better to die in America or somewhere else. Just about no one wants to die anywhere, at any time I notice. The mortality figures are too fuzzy to judge whether the extra cost is worth the money, but essentially there isn't enough provable difference among developed nations to assert most care lengthens the lifespan of the patients. Especially for cancer patients. Apparently, the diffusion speed of new knowledge makes it impossible to tell how much it helped. Or else the amount of new knowledge isn't sufficient to show up in such crude data. By that standard, medical care is just as "good", one place or another, one insurance system or another. It just costs more, that's all. When some research laboratory finds a cure for cancer, health care still won't seem to have proved it helped.
But life expectancy will increase; in the long run, costs will come down. It can be very confidently assumed that those who invest their savings early in life will enjoy a more prosperous retirement than those who depend on entitlements.
Sometimes, Even the Supreme Court Looks Negligent
If the United States Supreme Court makes a mistake, it remains pretty much a mistake in residence until the Court itself re-examines the matter. It would be indelicate for anyone else to cite a list of examples for this observation, so they are customarily taken up one at a time, at considerable expense. The desirable re-examination with the greatest consequence to Healthcare would be the 1982 decision in State of Arizona v. Maricopa County Medical Society.
Maricopa County is where Phoenix is located in Arizona, and its County Medical Society was one of the pioneers in what was then called Foundations for Medical Care. These were organizations in which local physicians took the lead in organizing and managing health insurance for the local community. The rules and policies of the Foundations were conceived and implemented by physicians, who were dismayed by the consequences of defects in health financing they could see in daily practice. Except for this physician dominance, it would be fair to say that Foundations for Medical Care were about the same as what we now call HMOs. It is also true these physicians were impatient with both the government and the health insurance companies, who seemed to resist helping the sick poor by implying it might violate some per se technicality aimed at business corporations. As the lame excuse would have it, our hands are tied. The obvious fact is someone in Arizona didn't like physicians or didn't like what they were threatening to do.
An agreement among competitors to lower prices for the poor, is after all not exactly the same anti-competitive behavior, as a "contrivance" to raise prices for your own benefit. It seemed most unfortunate to lump it together with its opposite as "per se" violations, requiring no examination of the evidence to distinguish the two. And furthermore, on the topic of regulating business corporations, it is not exactly an enumerated Constitutional power of the federal government, to amend the Constitution by treating all corporations as essentially identical or lowering prices the same as raising them. The whole anti-Foundation movement sounds pretty spurious.
At the same time, "Foundation" physicians believed they could see opportunities for reducing waste in the local hospitals which would only be exploited if physicians were in charge because physicians could sense the cost/benefit more readily than anyone else. Having recently returned from the Korean War, these doctors knew medical care could be excellent even without such a thing as health insurance, and indeed even if hospitals were only a collection of tents. Perhaps a few of them were overly influenced by the TV serial, "MASH", whose central theme is that if doctors take the lead and do the right thing, much can be forgiven. That's a sort of Hollywood restatement of the latitude of ancient Courts of Equity, charged with finding a way to achieve Justice --to cover a situation where obvious harm exists, but no law exactly addresses it.

Accordingly, the "better sort" of the doctor in Arizona believed they perceived the respectable doctors would readily agree to care for the poor at lower rates, whereas the shirkers in their midst would ruin things for everybody by refusing to do a fair share of pro bono work. Like labor unions, the doctors greatly resented the free rider phenomenon.
The idea of a two-class system of medical care was also abhorrent to them, however; if there wasn't enough money to spread around, a "good" doctor would just agree to lower his fees unilaterally. This moral quarrel often conflicts American business, which takes the view that it doesn't really matter what costs or taxes or burdens are imposed by the government. What matters to big business is that all competitors need to abide by the same handicaps. When handicaps are roughly equal, the difference between success and failure is -- talent. But the contrast between that and the antitrust position of individual tradesmen has never been satisfactorily defined.
To a considerable degree, talent rising to the top summarizes the aspirations of the anti-trust statutes, where it regularly becomes a source of both suppression and escalation of prices. Physicians are ultimately expected, not least by their colleagues, to find their highest duty is fiducial to the patients' best interest, particularly when the main conflict is merely a financial one. A corporation, by contrast, has a primary duty to its shareholders, who can sue them if they put benevolence ahead of profit. A corporation is a contract between the State and the shareholders, quite the reverse of the duty of government to its individual citizens. In the antitrust arena, the contrast between citizen and corporation is jumbled. Particularly in the case of the per se violations, the difference between a business corporation and a medical society is quite wide enough to justify considerable professional latitude. As it is not, in the case of insurers, and as it only partly remains, in the case of hospitals. Anti-trust statutes could have a real value in distinguishing borders between individual tradesmen and various groupings of them, but so far the distinctions are far from reasonable. The Maricopa Medical Society responded with perhaps excessive enthusiasm to the challenge of making local sense out of a price-fixing dilemma, but it was never given the opportunity to make its case.
At one time, local healthcare costs were suppressed by imposing competition on the hospitals, holding insurance administrators to be mindless clerks to pay the bills, not as cup-bearers of fairness in a naughty world. Needless to say, the hospitals and health insurers had long chafed at the ability of physicians to switch hospitals freely, and the patients to switch insurers, whereas Arizona's Attorney General seemed to suspect some vague return to Robin Hood notions of a special right to defy the law. Somehow the ancient concept of professional latitude has been supplanted as inconvenient to the goals of competitors. In certain parts of the country, big business is already expanding its financial control of hospitals and insurers, into acting as agents for assuring high-quality medical care, while suppressing its cost. On Wall Street, such behavior is quickly seen and labeled as "talking up your book of business". With the defeat of physicians by the Maricopa decision, plus the withdrawal of big business owners from identifiable management roles, the way was soon opened for hospitals and insurance companies to assert unrestrained control of their own finances. Thirty years later, hospitals and insurers are now universally merging, and applying selective controls over admitting pliant physicians as their employees. The Affordable Care Act is the mechanism by which the government interjects a new layer of control, thereby converting the government itself into the new hidden battlefield. It seems a very far cry from leaving medical decisions in the hands of physicians and their patients, to choose treatments, and to agree on their price.

|
| Sen. John Sherman |
The Attorney General of Arizona, himself a colorful character, soon brought suit for an anti-trust violation, since price-fixing was a declared per se violation or identification of the absence of competition. These were additions made to the Sherman Anti Trust Act by earlier Supreme Courts, who found an Act first written on the back of an envelope was lacking in regulations. Further strictures were imposed by the Clayton Anti-Trust Act, but these both might be remedied by subsequent Congresses, and thus lacked appropriate majesty. The crucial consequence was that the District Court of Arizona found it quite unnecessary to hold a trial or hear the evidence. The Court found against the doctors entirely on the basis of a motion for summary judgment. The matter then passed through the Court of Appeals to the Supreme Court, which on the theory that price fixing is price fixing, on a vote of 4 to 3, upheld the Arizona suit. All the way from a writ of summary judgment in a district court, to the United States Supreme Court, without formal examination of the facts. If either of the two absent members eligible to vote, had voted, it is certainly mathematically possible for the decision to have gone the other way.
Perhaps, strictly on lawyerisms, that was safely correct. But in terms of the effect on medical care, it won the war for control of hospitals and the insurance companies which began with Abraham Flexner's beatification of college-educated physicians. Somehow Maricopa was interpreted to mean that a hospital or an insurance company might do many medical things which were forbidden to organizations run by physicians. The consequence is Foundations run by physicians are under constant threat of what might happen to them if they do what HMOs are now seen to be doing every day. The whole Clinton health fracas revolved around this particular case and its implications. From the physician point of view, if you had medical training, you had been disqualified from running a Health Maintenance Organization, because a change of leadership seems to shift the antitrust issue to a different level within two identical organizations. And that was true even if the physician had been trained for the role, while the administrator had not.
What was particularly galling was to be tarred with the brush of antitrust, whereas others could describe identical behavior as self-disciplined and in the public interest. Self-imposed financial restraint was taunted and abused by aspirants for the same job with the same temptations, with multi-million dollar incomes, but without adherence to the same code of ethics. The emerging joke is that after the Clinton Healthcare Plan's uproar, the public decided they disliked HMO's intensely, mainly because they couldn't choose their own doctor, and the doctor was being hampered in doing what seemed professionally best for the patient. None of these legal issues had significantly arisen for physician-run HMOs. While of course, that outcome might appear, such disputes would be settled by physicians, using medical arguments, followed by a change in management if the medical community at large, widely disagreed with the decision. The only substantial difference was that doctors were running one organization but subservient in the other, and the Courts had found that whenever doctors were in charge it amounted to price-fixing between competitors. As matters eventually turned out, the hospitals resolved this battle by converting nearly all practicing physicians into their employees, and the war has now shifted to who will control hospitals.
It now remains for some case to be found and carried to the Supreme Court which might allow an examination of the facts of this matter, perhaps remanding the case back to the District Court to hold a trial. That would seem a bare minimum after thirty years, even though now it might no longer address precisely the same issue. Somehow, a way must be found to examine which of two rather extreme theories of the Wild Wild West needs to be laughed off. Either we must re-examine whether, always and everywhere, price-fixing is such an undiluted evil it never requires an examination of the evidence. Or whether the absence of identifiable harm introduces a balancing need to question such judgments when made under professional circumstances.
While on the subject of mixing business practices with professional standards, we might as well direct judicial attention to the unfair and probably (equal justice) unconstitutional tax preference for employers who purchase health insurance for their employees, to enjoy a huge corporate tax saving themselves by doing so. Not merely for the benefit of the employees, which is much discussed, but a usually much greater financial benefit for the shareholders when the corporate tax level is high enough. An unnecessary grievance is created for millions of self-employed and unemployed people who lack this tax shelter, and also for the owners of usually much smaller business enterprises, who must compete with them.
It might be argued that double taxation of corporations inevitably provides the loophole of double tax-exemption, and even this would often understate the discrepancy because of the differences in marginal rates. Lack of participation in this double tax benefit is arguably the main obstacle to extending employee health insurance to others or even substituting a superior health payment methodology. Now seventy years old, this grievance can be regarded, not only as having dubious evasions at its historical origin, but has resisted multiple efforts for repeal, and distorts the relative lifestyles of the two main participants in the workforce: small, and large, businesses. Henry Kaiser claimed he once had difficulty attracting employees to his West Coast war industries because of wartime wage and price controls, an excuse which should have ended the practice in 1945. Lack of a review-and-reconstruction of this bizarre lobbying product could potentially distort the application of the Affordable Care Act, in ways which are impossible to foresee. Indefinite enshrinement of the legal principles in this tangle, particularly the indefinite postponement of its resolution, could reverberate for more decades. The fringe-benefits circumvention, for example, has since grown entirely out of control, while it is fiercely defended by business and union interests. As it grows, however, the inequity to the self-employed and unemployed by remaining excluded from it, also grows.
Summary of the Maricopa Case
From a legal standpoint, the most uncomfortable feature of the case of the Maricopa Medical Society is that it went all the way to the Supreme Court without any trial of the facts or real opportunity for the defendants to present their case. That is, the whole HMO movement was effectively removed from the hands of physicians by a motion for summary judgment, on a Supreme Court decision, 4 to 3. It would be interesting to learn the attitudes of the remaining two Justices who recused themselves, but who could have reversed it.
To hold a trial of the facts by remanding the case for trial, would seem to be one easy way to introduce the defense which the doctors would have made. It could be improper to suggest to their lawyers what the defense should now be because new officers of the Medical Society might hold different opinions. The Medicaid Act was passed in 1965, requiring state consent for a jointly administered program. By 1972, Arizona was the only remaining state not to have agreed to Medicaid, which by then was widely recognized as the worst run and most underfunded medical program in America. In 1982, Arizona adopted a small portion of Medicaid, and it was only in 1988 that it fully adopted the program. In 2001, Arizona's governor was offered 7.9 billion dollars over four years, as matching money for the insurance exchange feature of the Affordable Care Act, which by then heavily absorbed the Medicaid program. The Governor recommended to the Legislature that they accept the offer because at least it was "better than Medicaid". There can be little doubt the Legislature of Arizona was adamant on the issue. And the Medicaid program is certainly better funded than it formerly was. But the central feature of Medicaid's HMO remains that of the Maricopa decision: its policies and administration are not directed by physicians. On the issue of whether the control should rest with payers or professionals, payers prevailed.
What were the doctors expected to do with sick poor people? No doubt, there was a wide divergence of opinion, but it must have seemed likely to someone, only a handful of saintly volunteers would now step forward, and none of them would be willing to pay hospitals their list prices. There is some truth to the last part. The doctors felt it would only work by shaming a substantial majority of their own members into accepting the cases at discount prices, and the only weapon they had was to make it a condition for membership in the medical society. That might once have been a powerful incentive, but the systematic undermining of its powers has now made it more questionable whether it could still succeed in its original plan. At the time of the first trial, there was probably enough slack in hospital revenue to cover the indigent need. With a changing economy, the premise needs to be tested more hesitantly.
Under these contentious circumstances, surely the Supreme Court could, even now, find some words to devise a better outcome. Price fixing is a per se violation of the act, and there is little doubt that all HMOs now fix prices. Only a physician-run HMO can be accused of "fixing" prices too low for competitive reasons, although it has always been arguably how strongly they would naturally compete for indigent patients. The Supreme Court may be reluctant to overrule the price-fixing part because of the spill-over effect of a century of custom, and the Arizona politics of this case are surely thorny.
As time passes, the Maricopa case is fast becoming as dignified by long-standing, as the price "fixing" notions were when it all started. Surely, at least the Court could find some clarifying language about physician-run HMOs as obiter dicta . The response of the non-physician-run HMOs was to exploit the opportunity to eliminate the competition of physician-run groups within the price-fixed arena. In the meantime, however, the public has found HMOs run by non-physicians have become contentious in the extreme, whereas the earlier physician-run Foundations for Medical Care were tolerated by most physicians, and embraced by quite a few. The matter is one of the important threads in the Obamacare controversy, so the Supreme Court has an opportunity to improve quite a few situations by writing a clarifying paragraph or two.
Psychiatry: Scientific Frontier, or Stormy Seas ?
Although scientific news about healthcare research is mostly pretty good, a storm may be approaching in psychiatry. Not only are that specialty's finances in disarray, but as the rest of the profession steadily conquers its share of diseases, lack of progress in psychiatry becomes more noticeable. Large sums are donated and granted to repair this gap, in a typically American approach to such obstacles. Maybe it is too soon to expect dramatic results. President John Kennedy once learned Thorazine was helping psychotic people go home from state mental hospitals, and put that information alongside the painful cost of maintaining 500,000 rather decrepit beds. Effectively, he closed most of them. It was well-intentioned but too quick. The important thing to notice was how very many psychotic patients there were, and therefore how big a job it entails.
 Psychiatry was ruined, first by Freud, and then by the DRG. 
|
Around 1965, the recreational drug scene along with its flower children and colorful activists unexpectedly hit us, trailed by optimistic news reports that heroin really wasn't so bad, LSD might have therapeutic potentials, and marijuana might even be beneficial compared with alcohol. Some of these contentions have been scientifically dismissed, but one discovery was greeted with delight by school children: marijuana was about the same as alcohol, but the smell on the breath didn't give it away. For a while, it was unclear whether drugs made you psychotic or psychotic people were attracted to drugs; it's still not entirely clear. The city police, who were dragooned into maintaining law and order amidst this commotion, resorted to the only resource they had, which was the local jails. The public agreed, perhaps hoping to scare the miscreant children, and passed laws about speedy trials for drug offenders, mandatory jail sentencing, and mandatory long sentences. The prisons filled up, older prisoners taught newcomers some tricks, and it was not long before the prison systems and the school systems were destabilized. We closed the snake pits and skid rows, all right, but we gave ourselves a drug problem, a prison problem, and a school problem.
The simultaneous development of a problem we had never quite seen before, at least to anything like a similar degree, caused a few reflective people to remember we had always had a large segment who was mentally unstable. It was a tenth of the population, possibly even a fifth. My pristine suburb spends 8% of its budget on "Special" education. Some of this was indeed new. Alzheimer's disease is one of the outgrowths of the advancing longevity we are so proud of. Women who delay having children are especially prone to deliver babies with Down's syndrome of mental retardation. Women are now going to work instead of tending children and aging parents, forcing these patients more into the open. The mechanization of warfare means more rejections for mental inferiority because soldiers need to be smart to be trusted with such weapons. So it's hard to know whether there is more mental disorder than before, or whether it has always been there, and is emerging from the shadows. In any event, we must newly face a very large segment of the population who are unemployable, and as they age, are adrift even from the discipline of regular employment.
The medical profession, preoccupied with its more usual tasks, woke up to this situation in odd little ways. One strange alert we might have noticed was the woeful inability of any medical coding system to define a relationship between psychiatric diagnosis and its treatment. In almost every other sort of condition, the diagnosis alone conveyed a pretty good idea of what the disease would cost; not in psychiatry. That was true within SNOmed and ICDA, the two main diagnostic codes for all fields of medical diagnosis, as futile efforts to squeeze it into DRG were to prove. It is also just as true within DMS (Diagnostic and Statistical Manual of Mental Disorders), the codes the psychiatric profession struggled to devise as a codebook of legitimate psychiatric conditions. It's definitely possible to construct an organized list of psychiatric diagnoses, using numerical codes instead of words. But it defies the imagination of everyone who tries it, to establish any reproducible connection between psychiatric diagnosis codes and the duration, cost or efficacy of treatments. Especially efficacy of treatments, without which little progress can be expected.
In the future, expect to hear less and less about surgery and medicine. Lots of people get sick, but sick with fewer different diseases. Research currently only seems to need to devise four or five cheap effective cures. But with psychiatry, the research is powerfully inhibited by the thick impenetrable skull, the lack of resemblance between the brain's anatomy and its functions, the extreme dangerousness of surgical experimentation, and the lack of any good idea how to connect the brain with the mind. We have a long, and expensive, way to go.
The American Health Plan; Only in America is it Imaginable
Nobody told us to do it, but let no one suppose our scientific community was the only group who had the notion. Exceptionalism likely originates deep in our culture of conquering the wild frontier. There's also the Abe Flexner or Teddy Roosevelt progressivism theory, but sometime during the winning of World War II, we Americans strongly exaggerated the idea we could do anything and carried that idea to surprising levels. Somewhere in the course of building the atom bomb, landing a man on the moon, defeating the whole world at war, defeating the Great Depression, and winning a whole lot of Nobel Prizes, we gave ourselves the idea we really could conquer all of the diseases. All it seemed to require was to spend tons of money and to set our minds not to quit. It probably is well to remember that at the time of the Bretton Woods Conference in 1944, we had two-thirds of the gold in the world, locked up in Fort Knox. Foreign trade was paralyzed because nobody else had any money.
Since 1900, average longevity has expanded from 47 years to 83. At least thirty major diseases have disappeared, fifty percent of drugs now in use were unknown just seven years ago, and so on. In 1950 we had 500,000 licensed beds for a mental disorder, in 2010 only 40,000, although John Kennedy's impulsiveness probably overdid it a bit. Far from all those mental patients were transferred to jail, and far from all those jail inmates came from mental hospitals. There has been a remarkable acceleration of scientific discoveries, new drugs, new cures. And it would take more than money to do it. Why worry now about what medical care costs, when it is obvious if we cured all the diseases, even the poorest among us could easily afford to spend -- nothing at all on health care. Foreigners scoff at such childish belief, but then, they retire in their thirties and wonder why they don't accomplish anything. Nobody ever won a war without taking casualties. You aren't listening to Quakers, when you hear that last one; the feeling isn't universal, nor is it always valid.
 If we cured all the diseases, even the poorest could afford to spend nothing at all on health care. 
|
To make it last, maybe someone has to cut costs. The hospitals are the single largest source of medical spending, so somebody's unspoken plan is to let them put on fat for the coming winter, and then suddenly cut them off at the knees. After all, hotels seem to be considerably cheaper, and retirement communities run infirmaries at a fraction of the cost. We instinctively know state licensing agencies are somehow protecting some monopolies, which will disappear if we pass a few laws, although the Maricopa decision shows the weakness in acting on that hunch. All in favor, signify by saying aye, and it's as good as done. As somebody once said, nobody ever won a war without taking casualties.
It has been noticed by others we tend to make systematic prediction errors. If you predict what you will accomplish in a year, I'm sorry to say you can't get that much done in a year. But if you predict what will occur in twenty years, you always underestimate the enormous changes to take place in two decades. If you experiment between short-term extrapolation failures for what can change in a year, on the one hand, and imagination failures for what will take place in twenty, at the other extreme, it appears that predictions for about six years come out closest to what does actually happen. I think I got that from The Economist.
Will medical costs be substantially lower in six years? Probably not, but they will probably be somewhat lower, just from extending the scientific advances we have already made, to more or less everybody within our borders. Beyond that, much will depend on the scientists. Whether major discoveries will emerge, or how often, is beyond present prediction. But in five or six jumps, we can expect present accommodations to health costs, to become quite obsolete. Read the proposals to deal with them, which appear in a later section, in that light.
Although the language of exceptionalism really isn't my native language, right now the general sense it conveys seems roughly correct. Although I'm not as reckless as some would be with research funding, I do believe the general sense of it is correct. With a little bit of luck, and considerable help from newly developed centers of foreign research, present trends do seem to be leading to a drop in both research costs and health delivery costs reasonably soon, let's say during the next generation. Improved transportation, telemedicine, and extended longevity seem to hold the promise of slimming most medical costs as we now know them. And it does seem to be reasonable to make most general hospitals into tertiary care centers, and then to shift the center of bread and butter medical care to the suburban and exurban retirement centers. Mostly, we need better transportation arrangements, to do so fairly soon.
What seems to be retaining the center of gravity in the present urban Medical Centers, seems to be: the location of research already present in those places, and the use of indigent populations for teaching purposes. When research (read: government funding) begins to dry up, it is my prediction the center of healthcare delivery will shift with the population centers, adjusted for their sickness content. My guidepost is the Hershey Medical Center, located on the most fertile farmland in the world, and only a few miles from where my ancestors lived for two hundred years. Each year I make a trip there, and every year there are more mini-mansions. A dear friend of mine advised Milton Hershey on how to build a medical school in the boonies, and frankly, all it takes is money. When present funding dries up, the center of Medicine will move to where the sickness is, unless the government gets in the road of it. As far as I can predict things, it seems to mean medical care will move to retirement centers (CCRC). Some people prefer high-rise apartment buildings, but building vertically is invariably more expensive than building horizontally. Very likely, the migration of both healthcare and retirement will be dominated by making financial resources stretch further. Research? Well, research is a young person's game, so let them plan to retire earlier and become administrators later.
My ability to predict politics is poor, so I notice politicians can sometimes direct funding into wasteful directions. We might annex Canada, Mexico, and Cuba, and thereby jumble up the American economy in unrecognizable, unpredictable ways. Or we might annex Canada, Iceland, Ireland, and England, for a different unpredictable future. Any of that would just be our Exceptionalism, carried out in another direction. But somebody else's exceptionalism might turn us all into a lump of molten ash, so this is a better choice. Using the same unconstrained reasoning, our leaders may decide the direction started by the careless Maricopa decision was ill-advised, and the people trained by the system Abraham Flexner set into motion are better qualified to run research systems than the people elected on the second Tuesday in November. Governing this, however, will be the nature of the reaction when the taxpayers discover a few awkward things, like who benefits most when an employer gives health insurance to his employees as a tax-deductible gift.
Second Edition: The Cost of Alternative Solutions
When the Democrats select their candidate for President, I will probably have more to say about their plans for paying for healthcare. Currently, Mrs. Clinton is defending Obamacare for the primaries, implying that she leans toward "Single payer" for a permanent program. If she reverts to HMOs as she once did for Clintoncare, I will definitely have something to say. At the moment, however, Mr. Sanders of Vermont looks like a promising candidate, and he is unabashedly in favor of Single Payer.
And he is supported in this by Henry J. Aaron, the economist at the Brookings Institute who for many years was a consultant for the real cause of the cost problem, the employer-based system. Other economists, such as Paul Krugman, have emerged with the cost argument against Single Payer (i.e. Medicare for everyone) that has frustrated them ever since Single Payer has been under discussion. It costs too much. Obamacare has suffered from this criticism with a budget of SEVERAL trillion dollars for ten years, which might have been sustainable under ordinary circumstances, but threatens to capsize the national economy in the midst of the worst recession in eighty years. Kenneth E. Thorpe of Emory University estimates the total ten-year spending of Mr. Sanders at above thirty trillion dollars. That's somewhat between five and ten times as much as the Obamacare era.
To repeat a point made in other places, Medicare is currently the big budget-buster. For all the premiums and payroll deductions, Medicare is supported by a 50% subsidy from general funds. General funds will not support such a deficit, so recently we have been borrowing it from the Chinese government, through the mechanism of selling them U.S. Treasury bonds. Is that what we have in mind, when we talk about Single Payer?
Suggested Additions.

|
| Lanhee J. Chen |
Soon after the release date of the first edition of this book, an article appeared in the Wall Street Journal by Lanhee J. Chen and James C. Capretta of Stanford University, entitled Instead of Obamacare: Giving Healthcare to the People. The authors were in general sympathy with the Health Savings Account approach and made three other suggestions with which I more-or-less agree. But they add a fourth which makes me unhappy :
1. Continuous Coverage Protection. They rightly notice many mandatory auto insurance recipients take out insurance, pay a single month's premium, during which time they obtain their drivers' license. And then no further payments are made for the insurance. The authors propose higher premiums for those who do the same thing with healthcare insurance, but presumably waive the higher cost if insurance is continued for a full year. There are many people who are suspicious of making anything mandatory, but if it's mandatory, it's unfair to allow obvious loopholes of this sort to persist.
2. Medicaid Reform. The two commenting authors are evidently aware of the unsatisfactory quality of many state Medicaid programs and propose splitting Medicaid into two parts, one for able-bodied adults and their children, and another for the disabled and elderly. Essentially, this is a rewording of high-risk pools, partially achieved by splitting Medicaid from federal plans. While this division might mesh more easily with existing workers and their families in the event of universal coverage (under a single-payer system), by itself it would not address much else.
A more useful split would be between inpatients and outpatients. That would match Medicare A and B, as well as the underlying Blue-Cross/Blue Shield organization of paperwork. Moreover, splitting helpless inpatients from ambulatory outpatients could surprisingly enable the marketplace to influence inpatient costs. Since a large number of outpatient and inpatient services are identical, it would establish a comparison framework for approximating inpatient to outpatient prices through a two-step market mechanism, which ultimately approximates market prices. For those inpatient services which have no outpatient match, a relative value system would provide a more stable way to set prices for the remainder of helpless inpatients. Doing this would close a loophole commonly employed to cost-shift inpatient costs to the outpatient area, resulting in vast confusion between two pricing systems for identical procedures. Hospital administrators would resist losing the ability to shift prices, so ultimately this is an argument about who is to dominate prices, the consumers or the providers. The "market" is a compromise between the two.
3. Medicare Reform. The main reason Medicare is often preferred to Medicaid is, it is potentially available to everyone regardless of income. But Medicare itself is 50% subsidized by the general taxpayer. No wonder Medicare doesn't need to mandate coverage. Effectively Medicare is subsidized more generously than Medicaid and thus is the main source of healthcare deficits. You might subsidize Medicaid more generously, or you could apply a 50% subsidy to a single-payer system. Either way will cost more, not less. Speaking politically, it is a question of whether you wish to offend the elderly Medicare patients or the younger indigent ones. Essentially, Congress has already chosen sides once and is unlikely to change its preference for current voters rather than potential ones. Finally, there remains one suggestion in the article which does make me uncomfortable, because of what it fails to say.
(4.) Retaining Employer Coverage. It still costs less to provide health insurance for employees, than to pay them wages and let them buy the same health insurance with what is left. Employers are therefore better off giving health insurance as a gift, even though recent inflation has held back wages more than health costs. Presumably, this anomaly would not survive tax reform, because employer-basing has turned into one big tax dodge.

|
| James C. Capretta |
But if it should survive, it presents the alternative to rectify the injustice to the other half of (small business) employees, whose employers usually cannot donate the coverage and then make it up at a spuriously higher corporate tax rate. Persisting eighty years after World War II which created the pretext, this is an unnecessary reminder of the many irregularities in the tax code. However, a one-line amendment to the HSA Law would suffice to extend the same tax exemption to outsiders, allowing other issues to remain dormant. This simple amendment would permit the premiums of a catastrophic health plan to be paid by the Health Savings Account itself, thereby extending its own tax shelter to HSA owners, at less additional commotion to the Treasury than a full exemption. The present inflation distortion should not be missed as an opportunity to restore fairness, which almost everyone now recognizes to be nothing but a lobbying plum.
16 Blogs
Second Edition: The Coming Shape of American Healthcare
New blog 2016-02-22 20:30:38 description
Employer Based Health Insurance
Henry Kaiser's Cleverness Out of Control
Nations will do almost anything to win a war. But to keep doing it for eighty years after the war is over is preposterous.
Hospital Cost-Shifting by Age Group, Patient Income, and Payer Class
Healthcare costs for all ages are almost exclusively financed by working-age people, 21-66.
Diagnosis Related Groups (DRG), in Relation to Medical Electronic Records.
 The DRG classification system was developed independently of the hospital payment system, for a different purpose. The hybrid use for hospital reimbursement has worked surprisingly well but needs extensive revision.
The DRG classification system was developed independently of the hospital payment system, for a different purpose. The hybrid use for hospital reimbursement has worked surprisingly well but needs extensive revision.
Hospital Cost-Shifting Reacts to the DRG
Payment by Diagnosis (DRG) turned out to be a rationing system. Hospitals responded by shifting inpatient costs to outpatients.
The Doc Fix
For eighteen years, a Federal law required a reduction of physician Medicare payments if the Medicare costs rose too fast. At the last moment, Congress would always relent and pay the doctors. Presumably, it showed them who was boss. As soon as Republicans gained a majority in both houses of Congress, the law was repealed, so it isn't hard to guess who was behind it from the beginning.
Amending Laws Rather than Rejecting Them
Two centuries of shifting power to the federal unit, has left other units with very limited taxing power. The resulting game is to shift federal funds to pay for state and local obligations.
Heath Insurance Companies Reach for the Brass Ring
As long as insurance remains profitable, the companies will try to dominate.
Is It Better to Die in America?
New blog 2016-02-17 21:20:34 description
Sometimes, Even the Supreme Court Looks Negligent
On motion of summary judgment, by a vote of 4 to 3, the Supreme Court muddled up medical care.
Psychiatry: Scientific Frontier, or Stormy Seas ?
The American Health Plan; Only in America is it Imaginable
People with roots still in European culture, deride American exceptionalism, point to alternative ways to spend our disposable income and feel it is dispositive that no other advanced nation imitates our health system. But our system has a logic that is seldom acknowledged because nobody else has the money to do it.
Second Edition: The Cost of Alternative Solutions
New blog 2016-02-17 23:18:27 description