Related Topics
Personal Reminiscences
One of the features of aging past ninety is accumulating many stories to tell. Perhaps fewer are left alive to challenge insignificant details.
Right Angle Club 2017
Dick Palmer and Bill Dorsey died this year. We will miss them.
Suited To A "T"

|
| Mucous Membrane Pemphigoid |
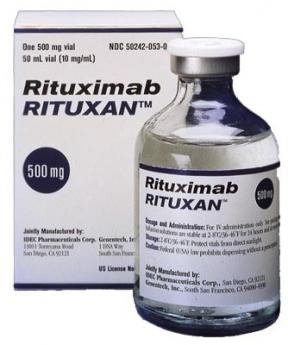
After sixty years as a doctor, it's a little disconcerting to find I have a disease I never heard of. It's better in a way, but in this sense it is worse, to be cured by a treatment I never heard of, either. The disease is mucous membrane pemphigoid, and the cure is Rituxamide. Am I right? Most readers have never heard of either one, but like just about every other patient, I think you all must just be panting to hear about it.
|
| Rituximab |
It turns out I had heard about the disease, but someone had changed its name from lichen planus to mucous membrane pemphigoid. The drug, Rituximab, has been around since 1997, treating rheumatoid arthritis, so it's not completely novel, either. It simply hadn't been used for this condition, which was rare. When we got semantic issues straightened out, and I had experienced a second round of treatment, I attended a seminar on lung cancer. That's the sort of thing doctors do for entertainment.
To my puzzlement, I was told a "me, too" variant of this same drug extended the life of lung cancer patients, but only if they were heavy smokers who quit smoking. That sounded peculiar, essentially saying you live longer from lung cancer if you smoke heavily and don't quit. You get a little euphoric when you take a steroid drug to ease the Rituximab, so I was overcome with the audacity to go to the microphone and announce I thought they lived longer, not because it helped the lung cancer, but because they lived longer by having fewer heart attacks and strokes from the smoking they had quit. Of course, I was politely told I didn't know what I was talking about. But an immunologist in the audience rose to say he agreed with me, because he had been giving the drug to practically every patient in his immunology practice, and quite a few of them got better. (To explain, the drug knocks out the T cells, which mediate most autoimmune diseases, so it sounded plausible.) So that's where matters stand. After everybody scrambles to try the drug on various autoimmune patients, some sort of order will probably emerge.)
But before everyone who reads this demands that his doctor gives him this drug for itchy skin, let me tell you the subsequent story. My insurance company sent me what is known as an "EOB" (explanation of benefits) which had two numbers on it. In the upper left-hand corner, it said my bill was $67,000. In the lower right -hand corner, it said the amount owed was $0.00. Somewhere between the two numbers is the amount you would have to pay if you didn't have insurance, the rest is someone's mark-up. I set about to find out how much the drug really costs to manufacture, and it's hard to find out. Someone said $4, but I can scarcely believe it.
Originally published: Wednesday, March 15, 2017; most-recently modified: Wednesday, June 05, 2019